What is the drug of choice for myasthenia gravis?
Monoclonal antibody. Rituximab (Rituxan) and the more recently approved eculizumab (Soliris) are intravenous medications for myasthenia gravis. These drugs are usually used for people who don't respond to other treatments.
How long do you take prednisone for myasthenia gravis?
The high-dose regimen consists of prednisone 1.0 to 1.5 mg/kg/d (but usually not >100 mg/d) for 2 to 4 weeks. After this period, a decision is made to immediately switch to every other day or to continue daily high-dose therapy.
What is the most effective treatment for myasthenia gravis?
What Are the Treatments for Myasthenia Gravis? There is no cure for myasthenia gravis, but it is treated with medications and sometimes surgery. You may be put on a drug called pyridostigmine (Mestinon), that increases the amount of acetylcholine available to stimulate the receptors.
Why is prednisone given in myasthenia gravis?
These illnesses are referred to as “autoimmune diseases.” Some autoimmune diseases, including myasthenia gravis, are caused by antibodies. Prednisone suppresses the production of antibodies.
Can steroids worsen myasthenia gravis?
Corticosteroids may produce a paradoxical worsening of myasthenia gravis (MG) symptoms within the first weeks of treatment.
What is the first line treatment for myasthenia gravis?
Pyridostigmine. The first medicine used for myasthenia gravis is usually a tablet called pyridostigmine, which helps electrical signals travel between the nerves and muscles. It can reduce muscle weakness, but the effect only lasts a few hours so you'll need to take it several times a day.
Is Mestinon a steroid?
Pyridostigmine (Mestinon) is not a steroid (or corticosteroid). It is an acetylcholinesterase inhibitor, so it works very differently from steroids.
How do you reverse myasthenia gravis?
By preventing or reversing the muscle weakness, the other symptoms are prevented or reversed as well. Myasthenia gravis can't be cured, but it is sometimes be treated with surgery to remove the thymus (which plays a role in the immune system) or with various drugs.
Can myasthenia gravis go away?
There is no cure for myasthenia gravis, but the symptoms can generally be controlled. Myasthenia gravis is a lifelong medical condition. Early detection is key to managing this condition. The goal of treatment is to increase general muscle function and prevent swallowing and breathing problems.
Which is more potent prednisone or prednisolone?
Prednisolone and prednisone doses are equivalent in a milligram to milligram comparison. In other words, 5 mg of prednisolone is as strong as 5 mg of prednisone.
How long does it take prednisone to work for ocular myasthenia gravis?
Conclusions: Moderate-dose daily prednisone for 4 to 6 weeks, followed by low-dose alternate-day therapy as needed, can control the diplopia in patients with ocular myasthenia gravis.
Can Mestinon and prednisone be taken together?
Interactions between your drugs PredniSONE may reduce the effects of pyridostigmine in the treatment of myasthenia gravis, at least temporarily. If you have been receiving treatment with pyridostigmine, you may experience increased muscle weakness when predniSONE is first initiated.
How long does it take for corticosteroids to work?
The clinical response to corticosteroids can start within days, and most patients experience initial benefits within the first 2 weeks. 19Patients attain maximal improvement on corticosteroids in the first 6 months, although some may take as long as 2 years or more.19There are 2 prevalent approaches to oral corticosteroids administration: a high-dose, rapid treatment induction regimen, and a low-dose and slow titration regimen (see Table 1). The slow titration regimen is designed to reduce the risk of initial worsening seen in as many as one-half the patients started on corticosteroids, but more commonly in the patient subset with severe MG or marked bulbar manifestations. The high-dose regimen consists of prednisone 1.0 to 1.5 mg/kg/d (but usually not >100 mg/d) for 2 to 4 weeks. After this period, a decision is made to immediately switch to every other day or to continue daily high-dose therapy. Switching immediately to alternate day high-dose corticosteroids may be used for patients who are Myasthenia Gravis Foundation of America (MGFA) grade 2 (mild). However, higher grade patients with MG usually require daily corticosteroid dosing for extended periods. Whether the patient is switched to a higher daily dosing at 2 to 4 weeks or left on high-dose daily therapy, the patient is usually kept on that dose (eg, 100 mg every other day or 50 mg/d) for another 4 to 8 weeks, at which time improvement should be noted and a slow taper by 5 to 10 mg a month can be initiated.
What is MG in neuromuscular transmission?
Myasthenia gravis (MG) is the most common acquired disorder of neuromuscular transmission. It occurs due to the production of pathogenic autoantibodies that bind to components of the neuromuscular junction, the most common being the acetylcholinesterase receptor (AChR). The incidence is estimated at 0.3 to 2.8 per 100,000 and the worldwide prevalence at 700,000.1In 1934, cholinesterase inhibition was demonstrated as the first effective treatment for MG.2Until the last 20 years, most MG treatment was investigated through retrospective clinical studies. More recently, there have been a number of randomized controlled clinical trials (Box 1). The decades that various MG treatments were introduced is shown in Box 2. This development has been associated with dramatic improvements in survival and prognosis in MG.3The primary reasons for reduced mortality rates are the improvement in intensive respiratory care and the introduction of immunosuppressive treatments. Although the mortality rate was previously quite high, resulting in the name MG, the current mortality rate in MG is reported as 0.06 to 0.89 per million person-years.4The various treatments for MG and the approximate time lag to onset of action are outlined in Table 1.
How long does pyridostigmine take to work?
A typical starting dose is 60 mg every 6 hours during daytime hours (see Table 1). Dosage may be titrated up to 60 to 120 mg every 3 hours aiming to minimize symptoms, but at these higher doses side effects are more likely to occur. Clinical effect onset is 15 to 30 minutes and its duration is about 3 to 4 hours. For patients who awaken at night or in the morning with impairing weakness, a 180-mg extended release formulation of pyridostigmine may be taken before sleep. However, owing to uneven absorption and unpredictable effect, the use of this medication has been limited.
What is pyridostigmine?
Pyridostigmine, a synthetic acetylcholinesterase inhibitor, inhibits the hydrolysis of the acetylcholine neurotransmitter in the synaptic cleft. This agent increases the number of interactions between the acetylcholine and the acetylcholine receptor in the neuromuscular junction. Pyridostigmine does not cross the blood–brain barrier, thereby limiting central nervous system toxicity, and may be mildly effective in ocular and generalized MG.
What are the side effects of corticosteroid treatment?
They include weight gain, diabetes, hypertension, eye disease (cataract and glaucoma), accelerated bone demineralization, and neuropsychiatric disturbances. Potential complications should be discussed before the initiation of treatment, and prevention and monitoring plans should be established in collaboration with the patient’s primary care physician. We recommend placing a tuberculin skin test or obtaining a QuantiFERON-TB Gold test to identify patients previously exposed to tuberculosis before starting corticosteroids therapy. Prophylactic therapy is indicated in those who test positive for prior exposure. Patients should be counseled about a low carbohydrate, low calorie, and low salt diet. If the patient is hospitalized, this can be done by the dietician. However, dieticians are often not available in the outpatient setting and, therefore, it is up to the neurologist to provide some dietary guidance. The advice of “no junk food/no salt when food gets to the table” is a good starting point, and should be reinforced on follow-up visits. A dual energy x-ray absorptiometry scan and an ophthalmologic examination should be obtained at baseline and repeated annually. Calcium (500 mg 2 to 3 times daily) and vitamin D (400 IU/d) supplements should be taken to reduce the risk of pathologic fractures. Patients should also remain up to date on all vaccinations, including the flu and pneumococcal vaccines, but no live or live attenuated vaccines should be used by patients on immunotherapy.29
When were acetylcholinesterase inhibitors first used?
Acetylcholinesterase inhibitors were discovered and introduced into medical practice during the 19th century.5In 1934, Walker hypothesized that physostigmine, an agent used as a partial antagonist to curare, may counteract the curare poisoning-like features of MG and described rapid onset and dramatic but temporary improvement in a 56-year-old woman with generalized MG.2,6She followed this with a brief and also positive report of prostigmine for generalized MG.7Prostigmine was the acetylcholinesterase inhibitor of the time from the mid-1930s to the mid-1950s, when pyridostigmine was introduced.8-11To our knowledge, branded Prostigmin is no longer available in the United States, but generic neostigmine is.
Does immunotherapy reduce MG?
Several retrospective studies have provided evidence that immunotherapy ( including treatment with corticosteroids) may reduce the risk of developing generalized MG in patients with ocular MG.27,28In the largest of these studies, after 2 years of follow-up, 36% of patients not treated on prednisone progressed to generalized MG versus only 7% of patients treated with prednisone.27In another retrospective study, pyridostigmine was used without prednisone in 59 of 97 patients with ocular MG with 12 developing generalized MG, whereas none of the 38 prednisone-treated cases developed generalized MG.16
What is acquired myasthenia gravis?
Acquired myasthenia gravis (MG) is an autoimmune disease in which antibodies reduce the number of available acetylcholine receptors and thereby impair neuromuscular transmission. The annual incidence of MG is between 0.25 and 2.00 per 100,000 population (Vincent 2003). The cardinal features of MG are weakness and fatigability of skeletal and extraocular muscles. In more than half of cases the initial symptoms are ptosis and diplopia, often followed by involvement of bulbopharyngeal and skeletal muscles. The natural history of MG is characterised by exacerbations and more or less complete remissions. Respiratory and swallowing difficulties during myasthenic crisis are life‐threatening and may require intubation and mechanical ventilation. In 382 patients whose disease began between 1940 and 1960, Grob (Grob 1981) reported death in 33%, remission in 11% and improvement in 20%. Recently, the death rate was reported to be less than 10% (Thomas 1997). Oosterhuis reported remission in 38% and improvement in 25% of 537 patients followed between 1960 and 1994 with changing treatment modalities (Oosterhuis 1997). Treatments tried include oral and intravenous glucocorticosteroids, azathioprine, ciclosporin, cyclophosphamide, methotrexate, intravenous immunoglobulin, plasma exchange (Hohlfeld 2003) and most recently mycophenolate mofetil (Chaudhry 2001; Ciafaloni 2001; Schneider 2001).
How does myasthenia gravis affect the body?
Myasthenia gravis is caused by the body's antibodies impairing transmission of nerve impulses to muscles, resulting in fluctuating weakness and fatigue. Acute attacks can be life threatening because of swallowing or breathing difficulties. Seven randomised controlled trials which included in all 199 participants are published. None fulfilled the presently accepted standards of a high‐quality trial. All these studies have risks of bias and have a weak statistical power. Limited evidence from randomised controlled trials suggests that corticosteroids offer short‐term benefit compared with placebo (dummy treatment). This supports the conclusions of observational studies and expert opinion. Limited evidence from randomised controlled trials does not show any difference in efficacy between corticosteroids and either azathioprine or intravenous immunoglobulin. All trials had design flaws which limit the strength of the conclusions. Further randomised controlled trials are needed.
Why do people take corticosteroids?
The rationale for using corticosteroids is the autoimmune nature of the disease and the beneficial effects of this group of drugs in other autoimmune diseases. The mechanisms of action of corticosteroids in MG are poorly understood. Effects on the activation of helper T cells and the proliferation of B cells, activated T cells and antigen‐presenting cells are considered to play a role (Lewis 1995). A beneficial effect of adrenocorticotrophic hormone (ACTH) was first observed by Simon in 1935 (Simon 1935) and later when it was given with the aim of 'shrinking thymoma' (Soffler 1948). In the early years exacerbation of myasthenic symptoms and a lethal outcome due to respiratory and swallowing difficulties were observed during the onset of high‐dose corticosteroid treatment (von Reis 1966). In a co‐operative study some 300 courses of ACTH were given to 100 patients, and 'good improvement' was reported (Genkins 1971). High‐dose alternate‐day administration of prednisone was also reported to have a beneficial effect (Warmolts 1971). Brunner et al. reported on nine patients treated with multiple short courses of intramuscular methylprednisolone in doses of 60 mg daily (Brunner 1972). To overcome the problem of initial worsening of MG, as reported with oral doses of 60 to 100 mg, Seybold and Drachman developed a safer regime with gradually increasing doses (Seybold 1974). In this open‐label trial the best results were achieved with courses of combined therapy including intramuscular or intravenous methylprednisolone followed by oral prednisone, with improvement being maintained for up to four months. A gradually increasing therapeutic effect of prednisone started after a few days but was usually obvious after two weeks or exceptionally after four to six weeks (Sghirlanzoni 1984). Initial exacerbation may occur despite slowly increasing alternate day schedules (Sghirlanzoni 1984). In the last 20 years several retrospective studies have reported very good efficacy of prednisone used with different dosages. A rate of 80.2% good results (remission or marked improvement) and 27.6 % remission in a series of 116 generalised MG patients was reported (Pascuzzi 1984). In other case series these figures were respectively 71.6% and 41.6% (n = 60) (Sghirlanzoni 1984), 63.4% and 33.8% (n = 142) (Cosi 1991) and 81.7% and 39.4% (n = 104) (Evoli 1992). Numerous side effects of varying severity were reported in all series including: osteoporosis, diabetes mellitus, infection, gastric ulcer, glaucoma and others. In the four series cited above at least one side effect was observed in 52.2% of the patients. Short courses of large intravenous doses were employed to manage exacerbations with good results (Arsura 1985). Serious complications were not reported in this study, but another study reported a severe myopathy following high dose pulses of systemic glucocorticosteroids (Panegyres 1993).
How has the outcome of MG improved?
With the introduction of mechanical ventilation, corticosteroids and other immunosuppressive agents and therapeutic plasma exchange, mortality has dropped to less than 10% . However, due to these therapeutic options the percentage of patients with a chronic and severe course of the disease is likely to have increased, but no exact figures are available. If in earlier decades the most severe patients tended to die during myasthenic crisis, the survivors would not reflect the same spectrum of the disease as the patients encountered more recently. This may introduce bias, when comparing treatment trials over the last 30 years, which is difficult to quantify.
Do corticosteroid treatments work for myasthenia gravis?
Limited evidence from randomised controlled trials suggests that corticosteroid treatment offers short‐term benefit in myasthenia gravis compared with placebo. This supports the conclusions of observational studies and expert opinion. Limited evidence from randomised controlled trials does not show any difference in efficacy between corticosteroids and either azathioprine or intravenous immunoglobulin.
Where are the search strategies in the MEDLINE appendix?
The search strategies are in the appendices: MEDLINE Appendix 1, EMBASE Appendix 2and the Cochrane Central Register of Controlled Trials (CENTRAL) Appendix 3.
Is glucocorticosteroid an immunosuppressive drug?
Although widely accepted as an appropriate immunosuppressive therapy, the efficacy of glucocorticosteroid treatment has only rarely been tested in controlled studies. This is an update of a Cochrane review first published in 2005 and previously updated in 2006 and 2007.
What is the treatment for myasthenia gravis?
Include medications, surgery, and other therapies. Myasthenia gravis (MG) can be treated with drugs, surgery and other therapies – alone or in combination. What’s right for you depends on the severity of your disease, which muscles are affected, your age, and the presence of other medical problems. Medications Thymectomy Intravenous Immune Globulin ...
How to help myasthenia patients?
Eat healthy. Like everyone, myasthenia patients should eat a healthy diet and maintain a healthy weight. This advice is critical for MG patients, because extra pounds make it even more fatiguing to get around and aggravate a host of other diseases. Talk to your doctor to see if a diet change will help ease medication side effects like fluid retention, bone loss or anemia.
Why do immunosuppressants help with MG?
Immunosuppressants help prevent your body from producing the harmful antibodies that cause MG weakness in the first place. At the same time, they also reduce the body’s production of good antibodies—which makes you more susceptible to infection and other diseases.
When was Myasthenia Gravis Fact Sheet published?
The Myasthenia Gravis Fact Sheet published by the National Institute of Neurological Disorders (updated February 19, 2016) and retrieved April 27, 2016.
How often is Rituximab given?
Rituximab (Rituxan) is given as a series of IV infusions every six months, and is especially effective in the MuSK variant of MG. The treatment suppresses the immune system by reducing B-lymphocytes.
What is immunoglobulin therapy?
Immune globulin therapy can be used to treat rapidly worsening MG. Immune globulin is a human blood product pooled from multiple donors who are carefully screened. By providing the body with normal antibodies from donated blood, IVIg treatments appear to temporarily modify the immune system.
How to treat MG?
MG treatment also includes self-care: getting plenty of sleep, resting your eyes, pacing your activity, eating healthy foods, exercising, and managing your stress. Listen when your body says “that’s too much.”. And cut yourself some slack. Recog nizing your body’s signals can take some trial and error.
How to diagnose myasthenia gravis?
To diagnose myasthenia gravis, doctors will test the nerve repeatedly to see if its ability to send signals worsens with fatigue.
What are some medications that can help with muscle contraction?
Cholinesterase inhibitors. Medications such as pyridostigmine (Mestinon, Regonal) enhance communication between nerves and muscles. These medications aren't a cure, but they can improve muscle contraction and muscle strength in some people.
What is the name of the tumor that is removed from the thymus gland?
Some people with myasthenia gravis have a tumor in the thymus gland. If you have a tumor, called a thymoma , doctors will surgically remove your thymus gland (thymectomy).
How long does IVIG last?
This therapy provides your body with normal antibodies, which alters your immune system response. Benefits are usually seen in less than a week and can last 3 to 6 weeks.
Does Mayo Clinic treat myasthenia gravis?
Our caring team of Mayo Clinic experts can help you with your myasthenia gravis-related health concerns Start Here
Does prednisone inhibit antibody production?
Corticosteroids. Corticosteroids such as prednisone (Rayos) inhibit the immune system, limiting antibody production. Prolonged use of corticosteroids, however, can lead to serious side effects, such as bone thinning, weight gain, diabetes and increased risk of some infections.
Is thymectomy a minimally invasive procedure?
A thymectomy can be performed as an open surgery or as a minimally invasive surgery. In open surgery, your surgeon splits the central breastbone (sternum) to open your chest and remove your thymus gland.
How to treat myasthenic crisis?
Treatment for a myasthenic crisis requires a hospital stay. That is because the person needs to be watching closely and may need help breathing as they receive other treatments. The other treatments used include: 1 1 Breathing support 2 Intravenous immunoglobulin (IVIG) 3 Plasmapheresis 4 High doses of steroids 5 Correcting nutritional issues 6 Treating underlying infections or other triggers
When do steroids kick in?
This means the steroids start to kick in about the time the effects of IVIG or plasma exchange are starting to decrease. Once the person is improving, the steroid dose is lowered. 1. After a myasthenic crisis, the person often goes home from the hospital taking a higher dose of steroids than they were taking before the crisis.
What is the first part of responding to a myasthenic crisis?
Helping the person breathe better is the first part of responding to a myasthenic crisis. If caught early enough, the person may only need breathing support from a bilevel positive airway pressure (BiPAP) machine.
What is IVIG injection?
Intravenous immunoglobulin (IVIG) Intravenous immunoglobulin (IVIG) is an injection filled with healthy antibodies. IVIG is most often given to people who have severe MG symptoms (a severe flare or myasthenic crisis) for a short time. It is a treatment that helps reduce the body’s attack on the nervous system. 1.
How long does IVIG last?
IVIG usually starts to work in 4 to 5 days, and the benefits last for 4 to 8 weeks. 1. IVIG may also be used on a regular basis if someone’s MG is more serious or does not get better using other treatments.
How often does a myasthenic crisis occur?
Myasthenic crisis is not a common problem of MG, but it does happen to about 1 in 5 people with MG at least once. 1,2. A myasthenic crisis leads to weakness of the breathing (respiratory) muscles. It is a potentially life-threatening situation that requires emergency care. A crisis often develops after days or weeks of slowly worsening symptoms ...

Overview
- Myasthenia gravis affecting multiple muscle groups throughout the body is called generalized myasthenia gravis. Other common muscle groups that are affected may make it difficult for you to chew, swallow, smile, shrug, lift your arm up, grip, rise to a stand, or walk up stairs. When the muscles necessary for breathing are affected, a patient is said to be in myasthenic crisis. This i…
- Lambert-Eaton (myasthenic) syndrome is also known as Eaton-Lambert syndrome. It is a rare autoimmune disorder of adulthood in which antibodies abnormally attack certain proteins on the surface of nerve endings that regulate calcium levels (calcium channels), resulting in inadequate release of acetylcholine. It is characterized by muscle weakness and fatigue, particularly of the h…
- Myasthenia gravis (my-us-THEE-nee-uh GRAY-vis) is characterized by weakness and rapid fatigue of any of the muscles under your voluntary control. It's caused by a breakdown in the normal communication between nerves and muscles.There's no cure for myasthenia gravis, but treatment can help relieve signs and symptoms, such as weakness of arm or leg muscles, double vision, dr…
Treatment
- Various treatments, alone or in combination, can relieve symptoms of myasthenia gravis. Your treatment will depend on your age, how severe your disease is and how fast it's progressing.
- Even though no rigorously tested treatment trials have been reported and no clear consensus exists on treatment strategies, myasthenia gravis (MG) is one of the most treatable neurologic disorders. Several factors (eg, severity, distribution, rapidity of disease progression) should be considered before therapy is initiated or changed. Treatment regimens are individualized depen…
- Once uniformly disabling and sometimes fatal, MG can be managed effectively with therapies that include anticholinesterase agents, rapid immunomodulatory therapies, chronic immunosuppressive agents, and thymectomy. Treatment is individualized and depends upon the age of the patient; the severity of the disease, particularly dictated by respiratory or bulbar involv…
- Treatment Decisions about specific treatment are based on specifics of each patients case. Recommended treatments for myasthenia gravis may include various measures that may alleviate symptoms, including anticholinesterase drugs (cholinesterase inhibitors) or alter the disease course, such as immunosuppressive drugs or surgery (thymectomy). Initial treatment c…
Symptoms
- Myasthenia gravis is a chronic condition that causes muscles to tire and weaken easily. For example, if you have myasthenia gravis, you may notice that during a meal, your jaw muscles become tired and weak, interfering with your ability to chew food. After you have rested for a little while, the muscles may become strong again, allowing you to resume eating. This waxing-and-w…
- Symptoms may be variable, with disease involvement potentially localized to certain muscles or affecting multiple muscle groups. In some affected individuals, the disease process may be limited to certain eye muscles, which is often described as ocular myasthenia gravis. In those with more generalized disease or generalized myasthenia gravis, affected muscles may include thos…
- Muscle weakness caused by myasthenia gravis worsens as the affected muscle is used. Because symptoms usually improve with rest, muscle weakness can come and go. However, the symptoms tend to progress over time, usually reaching their worst within a few years after the onset of the disease.Although myasthenia gravis can affect any of the muscles that you control …
- Among the first symptoms that persons affected by this disease notice are weakness in their eye muscles, trouble swallowing, and difficulty with muscles controlling facial expressions. People often do not recognize symptoms of Myasthenia Gravis immediately. Other people experience difficulty with slurred speech or trouble with breathing; the disease can affect any voluntary mus…
Diagnosis
- Your doctor will review your symptoms and your medical history and conduct a physical examination. Your doctor might use several tests, including:
- 1. Myasthenic syndromes: diseases of neuromuscular junction result from immune, toxic, genetic pathologies, including: 1. Lambert-Eaton myasthenic syndrome - associated with small-cell lung cancer; may occur many years before detectable lesion. 2. Autoimmune disorders. 3. Congenital myasthenic syndromes. 2. Multiple sclerosis (MS) - hyperreflexia and extensor plantar response …
- Definition of ocular MG (based on dysfunction due to MG at a specified point in time, and not dependent upon the duration of disease): MGFA Class I: Any ocular muscle weakness. May have weakness of eye closure. Strength in all other facial, bulbar, and limb muscles is normal. (It is recognized that some patients report fatigue when strength testing is normal. The physician sho…
- Symptoms of the following disorders may be similar to those of myasthenia gravis (MG). Comparisons may be useful for a differential diagnosis: Myasthenia gravis is diagnosed based upon a thorough clinical evaluation, detection of characteristic symptoms and physical findings, a detailed patient history, and a variety of specialized tests. The diagnosis is suspected based on …
Prognosis
- Treatments have improved over a period of 30 years, leading to significantly fewer deaths and better quality of life.The increasing use of immunomodulating therapies in recent years has been a major factor in improving the prognosis for patients with MG.However, while the disease usually responds to standard and nonspecific immunosuppression, current treatments frequently fail to …
- Definition of impending myasthenic crisis: Rapid clinical worsening of MG that, in the opinion of the treating physician, could lead to crisis in the short term (days to weeks). MG is a chronic disease that may worsen acutely over days or weeks (and on rare occasions, over hours). Treatment requires scheduled reevaluation and a close doctor-patient relationship. Patients wit…
- Often the symptom improvement may be mixed; as an example, there may be resolution of neck weakness and ptosis with persistence of diplopia. In general, limb and bulbar symptoms (dysphagia, fatigable chewing, and dysarthria) respond better to anticholinesterase drugs than the ocular manifestations (ptosis and diplopia). Diplopia is particularly resistant to these medication…
- The course of the myasthenia gravis is highly variable. For example, the degree of muscle weakness may vary over hours, from day to day, or over weeks and months, tending to increase with repeated muscle use and to improve with rest. In addition, particularly during the first years after disease onset, some affected individuals may experience alternating periods in which sym…
Cause
- Though anyone can develop myasthenia gravis, those most likely to do so are women between age 20 and 40 or men between age 50 and 70. If a woman with myasthenia gravis gives birth, the baby may have some temporary, and potentially life-threatening, muscle weakness (neonatal myasthenia) because of antibodies that have transferred from the mother's bloodstream. Typica…
- Congenital myasthenia is caused by genetic defects of muscle and nerve communication (neuromuscular transmission), and not an abnormal immune system. Congenital myasthenia usually occurs in infants but may become evident in adulthood. Other features may vary in severity among patients. Such abnormalities may include feeding difficulties, sudden episodes o…
- Your nerves communicate with your muscles by releasing chemicals (neurotransmitters) that fit precisely into receptor sites on the muscle cells at the nerve-muscular junction.In myasthenia gravis, your immune system produces antibodies that block or destroy many of your muscles' receptor sites for a neurotransmitter called acetylcholine (as-uh-teel-KOH-leen). With fewer rece…
- Myasthenia Gravis is caused by a malfunction of the person's immune system, although the causative factor remains unknown. The disease may have a genetic link. Potential causes include a form of genetic defect, resulting in congenital Myasthenia Gravis, and the circulation of maternal antibodies through the placenta, resulting in transient neonatal Myasthenia Gravis. There is a ne…
Pathophysiology
- The specific cause of abnormal autoimmune responses in patients with myasthenia gravis is unknown. However, researchers suggest that the thymus has some role in this process. According to reports in the medical literature, up to approximately 75 percent of individuals with myasthenia gravis have distinctive abnormalities of the thymus. In most cases, there are increas…
- MG is the result of an antibody-mediated autoimmune response, causing the body's immune system to target and attack certain muscle receptors that receive nerve impulses. In normal muscle contraction, when the impulse reaches the nerve ending at the neuromuscular junction, a chemical called acetylcholine is released that binds to receptors, causing the muscle to contract…
Definition
- MGFA Task Force defined goals of treatment of MG to achieve Minimal Manifestation Status (MMS) or better, with no more than grade 1 Common Terminology Criteria for Adverse Events (CTCAE) medication side effects. Operational definitions were set as follows:
- Myasthenia gravis (MG) is a chronic autoimmune disease characterized by fatigue and muscular weakness, especially in the face and neck, that results from a breakdown in the normal communication between nerves and muscles caused by the deficiency of acetylcholine at the neuromuscular (nerve-muscle) junctions. MG is the most common primary disorder of neuromu…
Management
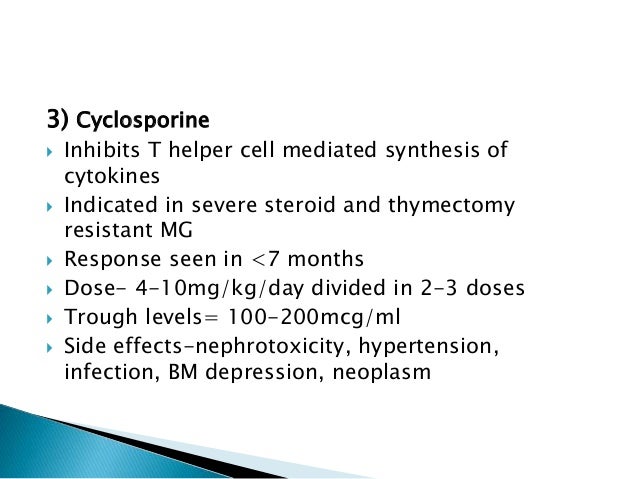
- Symptomatic treatment with acetylcholinesterase inhibition is usually combined with immunosuppression. Pyridostigmine is the preferred symptomatic treatment. For patients who do not adequately respond to symptomatic therapy, corticosteroids, azathioprine and thymectomy are first-line immunosuppressive treatments.Alternative immunosuppressive options to azathio…
- The indications, timing, and pre- and postoperative care of a patient with MG undergoing thymectomy should be managed by the surgeon in close collaboration with anesthesiology and a neurologist or other practitioner with expertise in MG to minimize the risk of perioperative worsening and respiratory failure due to MG. (See \"Anesthesia for the patient with myasthenia g…
Medications
- 1. Anti-acetylcholinesterase agents – Mestinon® (pyridiostigmine bromide)– allows acetylcholine to remain at the neuromuscular junction for a longer period, which in turn allows activation of more receptor sites, resulting in increased conductivity and muscle engagement. Mestinon® comes in two forms, fast-acting 60 mg tablets and long-lasting slow-release 180 mg capsules k…
- Your doctor may prescribe the following medications to treat myasthenia gravis:Aticholinesterase agents such as neostigmine and pyridostigmine (Mestinon) can help improve neuromuscular transmission and increase muscle strength.Possible side effects may include: 1. Gastrointestinal upset 2. Nausea 3. Excessive salivation and sweatingImmunosuppressive drugs such as predni…