Chronic inhaled corticosteroid use is safe in adults and children, and inhaled corticosteroids are recommended as first-line therapy in adults and children with persistent asthma, even if the disease is mild.
Full Answer
What is the best over the counter for asthma?
7 rows · Dec 08, 2010 · Beta-agonists are considered first-line therapy for intermittent asthmatics. If frequent use of ...
What are the best treatments for asthma?
For persistent asthma, low-dose inhaled corticosteroids are recommended in addition to reliever medication. Compliance to regular therapy can pose problems for disease management, and while intermittent controller therapy regimens have been shown to be effective, it is imperative to stress the value of regular therapy especially if an exacerbation occurs.
Should steroids be the first line treatment for asthma?
Jan 28, 2019 · People with mild persistent asthma experience symptoms more than twice per week but not as frequently as once per day. At this stage, your doctor will likely prescribe some form of daily medication...
What is the best OTC medication for asthma?
persistent asthma, either of the following two treatments are recommended as part of step 2 therapy: 1) a daily low-dose ics and as-needed saba for quick-relief therapy, or 2) intermittent as-needed saba and ics used one after the other for worsening asthma. 9 one approach to intermittent therapy is 2–4 puffs of albuterol followed by 80–250 mcg …
What medication is used for mild persistent asthma?
Theophylline. You take this bronchodilator daily in pill form to treat mild asthma. Theophylline (Theo-24, others) relaxes the airways and decreases the lungs' response to irritants. It can be helpful for nighttime asthma symptoms.
What is the first-line treatment for the management of asthma?
First-line treatment for acute asthma is an inhaled short-acting beta2 agonist (such as salbutamol) given as soon as possible. For children with mild to moderate acute asthma, a pressurised metered-dose inhaler and spacer device is the preferred option.
What is the recommended treatment for asthma?
Quick-relief inhalers (bronchodilators) quickly open swollen airways that are limiting breathing. In some cases, allergy medications are necessary. Long-term asthma control medications, generally taken daily, are the cornerstone of asthma treatment.Mar 5, 2022
What is the treatment for mild intermittent asthma?
International guidelines recommend as-needed inhaled steroids for mild asthma. For many years, as-needed albuterol or another short-acting β-agonist (SABA) has been the standard of care for patients with intermittent asthma, with an added daily inhaled corticosteroid (ICS) for patients with mild persistent asthma.Sep 26, 2019
What are 5 treatments for asthma?
Types of long-term control medications include:Inhaled corticosteroids. These are the most common long-term control medications for asthma. ... Leukotriene modifiers. These include montelukast (Singulair), zafirlukast (Accolate) and zileuton (Zyflo). ... Combination inhalers. ... Theophylline. ... Biologics.
Is Symbicort first-line for asthma?
International guidelines recommend their use as first-line treatment in asthma and the dose should be increased stepwise in accordance with asthma severity.
What is the gold standard for asthma treatment?
The gold standard in asthma therapy is still a low-dose ICS as a controller together with an on-demand Short-acting beta-2-agonist (SABA). An LTRA (Leucotriene-receptor antagonist) can be tried as a second choice.Jul 1, 2016
What is the second line treatment for asthma?
Medium dose inhaled corticosteroid (ICS), Leukotriene receptor antagonist (LTRA), or anti-IgE therapy are one of choices of stepping up asthma treatments. Tiotropium bromide is an anticholinergic drug, categorized as a long-acting muscarinic antagonist (LAMA) or long-acting anticholinergic bronchodilator.Oct 15, 2015
What is mild persistent asthma?
Mild persistent asthma is defined as requiring a low dose of ICS to achieve control, moderate asthma as requiring a higher dose of ICS or additional medication, and severe asthma as requiring high ICS doses plus add-on medication with or without oral corticosteroids.
How is moderate persistent asthma treated?
A small randomized trial found that patients with moderate persistent asthma who were started on a high-dose corticosteroid followed by the step-down approach experienced a more prompt improvement in respiratory function and asthma symptoms, as well as a lower maintenance dose of inhaled corticosteroids, compared with ...Sep 15, 2016
Should mild asthma be treated?
The condition can be very mild and require little or no medical treatment. It can also be severe and require daily treatment. Many cases of asthma, however, fall between those two ends. People who have symptoms of asthma more than two days per week but not daily may have mild persistent asthma.Jan 28, 2019
What is the best way to treat asthma?
Quick-acting bronchodilators: These short-acting medicines work to reduce inflammation and open your airways so you can recover from symptoms quickly. Sometimes, inhalers are used proactively, such as before exercise, to prevent symptoms. Others are used as rescue medication when symptoms of an asthma flare-up occur.
How to get rid of asthma?
Remove carpets for hard flooring. Use dust-resistant bedding, and wash curtains and linens regularly. Use an air conditioner: Open windows are great for natural air, but natural air is teeming with pollen, grasses, and humidity, which can all trigger asthma.
What are the symptoms of asthma?
Symptoms of mild persistent asthma include: shortness of breath. whistling when you breathe ( wheezing) coughing. mucus buildup in the airways. chest tightness, pain, or pressure.
How to prevent asthma flares?
Here are five ways to avoid asthma triggers: 1 Allergen-proof your home: Dust mites can cause asthma flares, so try to eliminate as much dust where you can. Remove carpets for hard flooring. Use dust-resistant bedding, and wash curtains and linens regularly. 2 Use an air conditioner: Open windows are great for natural air, but natural air is teeming with pollen, grasses, and humidity, which can all trigger asthma. Shut your window and use air conditioning to cut down on outdoor irritants. 3 Stay healthy: People with the flu, pneumonia, or even a routine common cold may experience more asthma symptoms. Get vaccines and wash your hands during peak disease seasons. 4 Protect your face: Cold air can trigger asthma symptoms when you breathe it in through your mouth or nose. Wear a scarf or jacket that can cover your face in frigid temps. 5 Clean regularly: Prevent mold accumulation by regularly cleaning damp areas inside your house and removing mold traps, such as leaves or firewood, in your yard.
How is asthma classified?
Asthma classifications are determined by how frequent your symptoms are, how much the symptoms interfere with your activities, and how often you have flare-ups that are higher risk (such as needing hospitalization or oral glucocorticosteroid therapy).
How many days a week does asthma last?
It can also be severe and require daily treatment. Many cases of asthma, however, fall between those two ends. People who have symptoms of asthma more than two days per week but not daily may have mild persistent asthma.
What is the FEV1 test for asthma?
Diagnosis. People with mild persistent asthma have lung function of over 80 percent of predicted normal during FEV1 breathing testing. That means your lungs have the ability to forcefully breathe out over 80 percent of volume in one second that’s predicted for lungs that aren’t affected by the disease.
What is the best treatment for asthma?
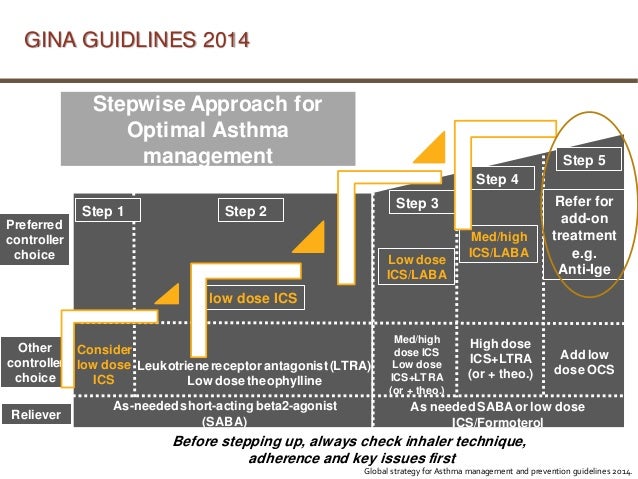
For individuals with mild persistent asthma, either of the following two treatments are recommended as part of Step 2 therapy: 1) a daily low-dose ICS and as-needed SABA for quick-relief therapy, or 2) intermittent as-needed SABA and ICS used one after the other for worsening asthma.
What is the focus of the 2020 Asthma Management Guidelines?
This Clinician’s Guide summarizes the 2020 Focused Updates to the Asthma Management Guidelines: A Report from the National Asthma Education and Prevention Program Coordinating Committee Expert Panel Working Group to help clinicians integrate the new recommendations into clinical care. The full 2020 Report, which is focused on selected topics rather than a complete revision of the 2007 Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma (EPR-3), can be found at nhlbi.nih.gov/asthmaguidelines. This summary guide should be used in conjunction with the full report. The Guide is organized by the following topics:
When to use subcutaneous immunotherapy?
In individuals ages 5 years and older with mild to moderate allergic asthma , the Expert Panel conditionally recommends the use of subcutaneous immunotherapy as an adjunct treatment to standard pharmacotherapy in those individuals whoseasthma is controlled at the initiation, build up, and maintenance phases of immunotherapy.
When to start ICS for wheezing?
In children ages 0–4 years with recurrent wheezing, a short (7–10 day) course of daily ICS with as-needed inhaled short-acting beta2-agonist (SABA) for quick-relief therapy is recommended starting at the onset of a respiratory tract infection.
Does asthma have an allergic component?
In some individuals, asthma can have an allergic component. Allergen mitigation strategies (e.g., air purifiers, impermeable pillow and mattress covers, HEPA filters) aim to decrease an individual’s exposure to allergens.
Does BT help with asthma?
BT may reduce severe asthma exacerbations compared with standard care after treatment. Although the benefits could last 5 years or more, only limited data demonstrate that this treatment improves long-term asthma outcomes.
Can you get BT for asthma?
Most individuals ages 18 years and older with uncontrolled, moderate to severe, persistent asthma should not undergo BT to treat asthma because the benefits are small, the risks are moderate, and the long-term outcomes are uncertain.
How often do you have asthma symptoms?
The effects of asthma pose minor limitations on normal activities. The occurrence of symptoms is more than two days per week but not every day. Nighttime symptoms occur three to four times a month. Symptoms require the use of a short-acting inhaler less than once per week.
What is intermittent asthma?
Intermittent asthma is the mildest form of asthma, with infrequent symptoms and no interference with normal activity. It is possible that, with proper trigger control and treatment, your mild persistent asthma could be downgraded to this classification.
How is asthma classified?
Asthma is classified based on several factors, including the frequency, severity, and impact of your symptoms. Your doctor will consider your medical history, perform a physical examination, and order diagnostic tests to determine if your asthma is mild persistent or not. The first time this is done, they will base the assessment on your asthma ...
What are the symptoms of asthma?
Symptoms. Your asthma symptoms may include difficulty breathing, wheezing, chest tightness, and coughing, like all cases of asthma. The criteria for mild persistent asthma criteria further define the presentation of symptoms for this type: The effects of asthma pose minor limitations on normal activities.
Can pollen cause asthma?
For example, if you meet the above criteria and physical activity is what brings on your asthma symptoms, you likely have mild persistent exercise-induced asthma. If exposure to pollen exacerbates your condition, you likely have mild persistent allergic asthma .
Can asthma be life threatening?
If your asthma fluctuates over time, your medication will need to be adjusted—the goal is always optimal disease control with minimal side effects. Keep in mind that anyone who has asthma can experience a life-threatening asthma attack, even if the asthma is classified in one of the milder categories.
Can asthma be controlled with medication?
If you have been diagnosed with mild persistent asthma, make sure to have an asthma action plan in place . Medications can help keep mild persistent asthma under control, but this is just one step in caring for your health.
What is the first line of treatment for asthma?
A doctor will typically recommend inhaled corticosteroid (ICS) therapy as the first-line of treatment if a person has mild persistent asthma.
How to diagnose asthma?
To diagnose asthma, a doctor will ask the individual to describe their symptoms. They may also ask the individual if their symptoms worsen when they have exposure to some common asthma triggers. The doctor is also likely to: examine the individual’s lower respiratory tract for signs of wheezing.
What is the most common type of asthma?
The most common kinds of asthma are mild intermittent asthma and mild persistent asthma. Asthma is a chronic condition that affects a person’s airways. It often develops during childhood, although adults can develop it too. The American Lung Association report that asthma is the most common chronic condition in children.
How often do you show symptoms of asthma?
A person is likely to have mild, persistent asthma if their symptoms are as follows: they show daytime symptoms more than twice per week, but less than once per day. flare-ups sometimes affect their physical activity. they experience nighttime symptoms more than twice per month.
Why do my airways swell?
Trusted Source. explains, when the airways are chronically inflamed, they can become hyper-responsive to specific triggers, which causes them to swell. This swelling can make it hard for oxygen to reach a person’s lungs. In a person with asthma, swollen airways have associations with some common asthma symptoms.
What information do doctors ask about asthma?
When a doctor evaluates a person’s asthma symptoms, they will ask for information about the following: the frequency and severity of daytime symptoms. the frequency and severity of flare-ups. the frequency of nighttime symptoms.
Is asthma persistent or mild?
Asthma can range from mild and intermittent, to severe and persistent. Asthma symptoms are generally more or less the same, but asthma can vary in severity and persistence. Asthma can range from mild and intermittent to severe and persistent. of all people with asthma have mild persistent asthma.
What is the best treatment for asthma?
Inhaled corticosteroids are recommended as first-line treatment in children with acute asthma. A. 2, 8, 9. The combination of a beta 2 agonist and an inhaled corticosteroid is superior to the addition of a leukotriene modifier.
What is the 1997 guidelines for asthma?
The 1997 guidelines from the National Asthma Education and Prevention Program (NAEPP) 1 noted that inhaled corticosteroid therapy offered multiple benefits in patients with persistent asthma, but some uncertainty remained about its use in certain patients. The NAEPP’s recent update 2 of the 1997 guidelines clarifies such treatment issues ...
What is the National Asthma Education and Prevention Program?
The National Asthma Education and Prevention Program recently updated its guidelines for the management of asthma. An evidence-based approach was used to examine several key issues regarding appropriate medical therapy for patients with asthma. The updated guidelines have clarified these issues and should alter the way physicians prescribe asthma ...
Is inhaled corticosteroids better for asthma?
The previous NAEPP guidelines 1 stated that inhaled corticosteroids were superior to other agents in the treatment of asthma. However, use of inhaled corticosteroids as initial therapy in patients with mild disease and in children was controversial.
Is it safe to take corticosteroid for asthma?
Chronic inhaled corticosteroid use is safe in adults and children, and inhaled corticosteroids are recommended as first-line therapy in adults and children with persistent asthma, even if the disease is mild.
Can corticosteroids help with asthma?
In addition to the previously known benefits of inhaled corticosteroid therapy in patients with asthma, recent data 6, 7 show that regular use of inhaled corticosteroids can reduce hospital admissions and dramatically decrease deaths from asthma.
How effective are corticosteroids for asthma?
Inhaled corticosteroids are the most effective long-term medication for asthma. 10, 15 – 18 They have been shown to reduce symptom severity, systemic steroid use, emergency department visits, hospitalizations, and deaths caused by asthma, and improve asthma control, quality of life, and objective measures of lung function. 10, 15 – 18 Adverse effects of inhaled corticosteroids are limited, with only a slight effect on linear growth of approximately 0.5 cm per year noted in children. The effect on linear growth lessens after the first year of medication use and seems to be independent of patient age or the type of corticosteroid, dose, or delivery mechanism. It is unclear if inhaled corticosteroid use has an impact on final adult height. 19 Other adverse effects, such as dysphonia, are generally self-limited or may be improved by changing the delivery mechanism of the inhaled corticosteroid. 20
How effective is immunotherapy for asthma?
Immunotherapy is effective in reducing exacerbations, need for medication use, and overall cost of care in patients with allergic asthma. 51 – 53 A 2010 Cochrane review found a number needed to treat of 4 to avoid one deterioration in asthma symptoms, but it could not determine the size of effect compared with other therapies. 54 Immunotherapy should be considered in patients with asthma triggered by confirmed allergies who are experiencing adverse effects from medication or have other comorbid allergic conditions.
What is the best combination of corticosteroid and laba?
The combination of an inhaled corticosteroid and an LABA is considered a preferred therapy by the EPR-3 for the control of moderate persistent asthma in children five to 11 years of age and those 12 years and older. 10 Combination therapy offers the best prevention of severe asthma exacerbations. 28 A 2013 study confirmed the overall safety of combination inhaled corticosteroid and LABA therapy, especially compared with LABA monotherapy. 29 Combination therapy dosing should be managed in a step-up or step-down approach similar to the management of inhaled corticosteroid therapy. Slight differences in when to start combination therapy are noted between the EPR-3 and Global Initiative for Asthma (GINA) guidelines. 10, 30 For example, according to step 3 of the EPR-3 stepwise approach for patients 12 years and older, either a low-dose inhaled corticosteroid plus an LABA, or a medium-dose inhaled corticosteroid alone is appropriate ( Figure 2). 10 The GINA guidelines recommend a low-dose inhaled corticosteroid plus an LABA as the preferred selection in this age group, with a medium-dose inhaled corticosteroid considered the secondary option.
What is the rate of CAM in asthma?
The rate of complementary and alternative medicine (CAM) use in children and adolescents with asthma is as high as 71% to 84%, but 54% of parents do not disclose the use of these methods. 55, 56 CAM use is more common among children with poorly controlled asthma and those with barriers to treatment. 57, 58 However, data indicate that CAM treatment is typically not used as a substitute for conventional medicine. 57 Patients who are receiving CAM substances should be cautioned that there is little regulation to ensure the consistency and purity of the contents and that CAM is never a substitute for rescue medication. Common CAM treatments and their effects on asthma symptoms are listed in Table 3. 59 – 74
Is methylxanthine a bronchodilator?
Theophylline, the most commonly used methylxanthine in asthma patients, acts as a bronchodilator at high serum concentrations (10 to 20 mcg per L [56 to 111 μmol per L]), but has an anti-inflammatory effect at lower serum concentrations (5 to 10 mcg per L [28 to 56 μmol per L]). 36, 37 Theophylline administered with inhaled corticosteroids decreases exacerbations, 38 but it has similar effects to increasing the dosage of the inhaled corticosteroid. 39, 40 The EPR-3 specifies that theophylline is a nonpreferred alternative to inhaled corticosteroid. 10 The GINA guidelines recommend a trial of increased dosage of inhaled corticosteroid before considering theophylline, unless steroid sparing is necessary, such as in patients with severe glaucoma or active tuberculosis infection. 30 Patients in developing countries are more likely to use low-dose theophylline than inhaled corticosteroids because it is a cheaper option. 39, 40 Although theophylline is considered safer at lower serum concentrations, care of patients who use theophylline should be comanaged with an asthma subspecialist because of the narrow therapeutic range of this drug and the risk of death from an overdose. 36, 40 Theophylline is metabolized in the liver and is susceptible to drug-drug interactions through cytochrome P450 1A2 ( Table 2). 37, 41
Is Butterbur effective for asthma?
Possibly effective. Butterbur. Traditionally used in Taiwan to treat asthma. Has anti-inflammatory properties. 61 A small non-randomized open trial showed 48% decrease in exacerbations, and 40% of patients were able to reduce their dosage of inhaled corticosteroids, but results potentially biased due to study design.
Can beta 2 be used as monotherapy?
Long-acting beta 2 agonists are effective for control of persistent asthma symptoms and are the preferred agents to add to inhaled corticosteroids in patients 12 years and older, but they are not recommended for use as monotherapy. A. 10, 27, 29.
How to help asthma?
Regular exercise can strengthen your heart and lungs, which helps relieve asthma symptoms. If you exercise in cold temperatures, wear a face mask to warm the air you breathe. Maintain a healthy weight. Being overweight can worsen asthma symptoms, and it puts you at higher risk of other health problems.
How to stop asthma attacks?
Treatment. Prevention and long-term control are key to stopping asthma attacks before they start. Treatment usually involves learning to recognize your triggers, taking steps to avoid triggers and tracking your breathing to make sure your medications are keeping symptoms under control.
How is asthma classified?
How asthma is classified. To classify your asthma severity, your doctor will consider how often you have signs and symptoms and how severe they are. Your doctor will also consider the results of your physical exam and diagnostic tests. Determining your asthma severity helps your doctor choose the best treatment.
What test is used to diagnose asthma?
Other tests to diagnose asthma include: Methacholine challenge. Methacholine is a known asthma trigger. When inhaled, it will cause your airways to narrow slightly. If you react to the methacholine , you likely have asthma. This test may be used even if your initial lung function test is normal. Imaging tests.
How to reduce asthma triggers?
Taking steps to reduce your exposure to asthma triggers is a key part of asthma control. To reduce your exposure, you should: Use your air conditioner. Air conditioning reduces the amount of airborne pollen from trees, grasses and weeds that finds its way indoors.
What is the best bronchodilator for asthma?
Like other bronchodilators, ipratropium (Atrovent HFA) and tiotropium (Spiriva, Spiriva Respimat) act quickly to immediately relax your airways, making it easier to breathe. They're mostly used for emphysema and chronic bronchitis, but can be used to treat asthma. Oral and intravenous corticosteroids.
What is the test for lung function?
Lung function tests often are done before and after taking a medication to open your airways called a bronchodilator (brong-koh-DIE-lay-tur), such as albuterol. If your lung function improves with use of a bronchodilator, it's likely you have asthma.