Is there a cure for Leigh's disease?
The most common treatment for Leigh's disease is thiamine or Vitamin B1. Oral sodium bicarbonate or sodium citrate may also be prescribed to manage lactic acidosis. Researchers are currently testing dichloroacetate to establish its effectiveness in treating lactic acidosis.
What is the best diet for Leigh’s disease?
Mar 27, 2019 · Treatment The most common treatment for Leigh's disease is thiamine or Vitamin B1. Oral sodium bicarbonate or sodium citrate may also be prescribed to manage lactic acidosis. Researchers are currently testing dichloroacetate to establish its …
What is Leigh's disease?
Oct 08, 2008 · The most common treatment for Leigh's disease is thiamine or Vitamin B1. Oral sodium bicarbonate or sodium citrate may also be prescribed to manage lactic acidosis. Researchers are currently testing dichloroacetate to establish its …
What imaging is used in the diagnosis of Leigh syndrome?
in the ideal case, muscle biopsy should be performed under general anaesthesia, since local anaesthetics applied into the skin and subcutaneous fat tissue might also come into contact with muscle tissue and potentially inhibit respiratory chain complex activity. 42 however, especially in adults, general anaesthesia is uncommon for diagnostic …
What is the best treatment for Leigh's disease?
The most common treatment for Leigh's disease is thiamine or Vitamin B1. Oral sodium bicarbonate or sodium citrate may also be prescribed to manage lactic acidosis. Researchers are currently testing dichloroacetate to establish its effectiveness in treating lactic acidosis.
How does Leigh's disease develop?
Leigh's disease can be caused by mutations in mitochondrial DNA or by deficiencies of an enzyme called pyruvate dehydrogenase. Symptoms of Leigh's disease usually progress rapidly.
How does Leigh's disease affect the brain?
Rarely, it occurs in teenagers and adults. Leigh's disease can be caused by mutations in mitochondrial DNA or by deficiencies of an enzyme called pyruvate dehydrogenase. Symptoms of Leigh's disease usually progress rapidly. The earliest signs may be poor sucking ability,and the loss of head control and motor skills.These symptoms may be accompanied by loss of appetite, vomiting, irritability, continuous crying, and seizures. As the disorder progresses, symptoms may also include generalized weakness, lack of muscle tone, and episodes of lactic acidosis, which can lead to impairment of respiratory and kidney function. In Leigh’s disease, genetic mutations in mitochondrial DNA interfere with the en...
What is the NINDS research?
The NINDS supports and encourages a broad range of basic and clinical research on neurogenetic disorders such as Leigh's disease. The goal of this research is to understand what causes these disorders and then to apply these findings to ne...
What is a NINDS trial?
NINDS Clinical Trials. Definition. Leigh's disease is a rare inherited neurometabolic disorder that affects the central nervous system. This progressive disorder begins in infants between the ages of three months and two years. Rarely, it occurs in teenagers and adults.
What are the symptoms of Leigh's disease?
As the disorder progresses, symptoms may also include generalized weakness, lack of muscle tone, and episodes of lactic acidosis, which can lead to impairment of respiratory and kidney function. In Leigh’s disease, genetic mutations in mitochondrial DNA interfere with the en... ×. Definition.
What is the function of mitochondria in Leigh's disease?
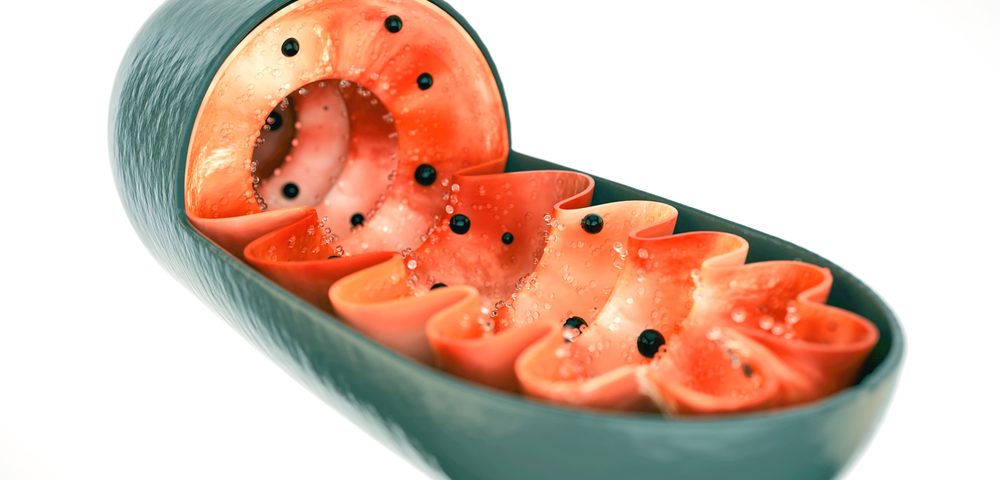
The primary function of mitochondria is to convert the energy in glucose and fatty acids into a substance called adenosine triphosphate ( ATP).
What are the symptoms of Leigh's disease?
Symptoms begin in infancy and include poor sucking ability, the loss of head control and motor skills, loss of appetite, vomiting, irritability, continuous crying, and seizures. As the disorder progresses, symptoms may also include generalized weakness, lack of muscle tone, and episodes of lactic acidosis, which can lead to impairment of respiratory and kidney function.
How do you know if you have Leigh's disease?
Symptoms of Leigh's disease usually progress rapidly. The earliest signs may be poor sucking ability, and the loss of head control and motor skills. These symptoms may be accompanied by loss of appetite, vomiting, irritability, continuous crying, and seizures. As the disorder progresses, symptoms may also include generalized weakness, ...
What is the brain disorder that causes seizures?
Epilepsy is a brain disorder in which the person has seizures. There are two kinds of seizures, focal and generalized. There are many causes of epilepsy. Treatment of epilepsy (seizures) depends upon the cause and type of seizures experienced.
What are the symptoms of encephalopathy?
The main symptom of encephalopathy is an altered mental state. Other symptoms include: coma. Treatment of encephalopathy depends on the type of encephalopathy (anoxia, diabetic, Hashimoto's, hepatic, hyper - hypotensive, infectious, metabolic, infections, uremic, or Wernicke's) are examples of types of encephalopathy.
What are the diseases caused by mitochondria?
Mitochondrial Disease. Learn about mitochondrial disease, genetic disease in which include a group of neuromuscular diseases that are caused by damage to the mitochondria Common mitochondrial myopathies include Kearns–Sayre syndrome, myoclonus epilepsy, and mitochondrial encephalomyopathy.
What is the function of mitochondria in Leigh's disease?
The primary function of mitochondria is to convert the energy in glucose and fatty acids into a substance called adenosine triphosphate (ATP).
What are the two types of seizures?
Seizures are divided into two categories: generalized and partial. Generalized seizures are produced by electrical impulses from throughout the brain, while partial seizures are produced by electrical impulses in a small part of the brain. Seizure symptoms include unconsciousness, convulsions, and muscle rigidity.
What is the prognosis for Leigh's disease?
The prognosis for individuals with Leigh's disease is poor. Individuals who lack mitochondrial complex IV activity and those with pyruvate dehydrogenase deficiency tend to have the worst prognosis and die within a few years.
What is Leigh's disease?
Description. Leigh’s disease is a rare inherited neurometabolic disorder that affects the central nervous system. This progressive disorder begins in infants between the ages of three months and two years. Rarely, it occurs in teenagers and adults. Leigh’s disease can be caused by mutations in mitochondrial DNA or by deficiencies ...
What is the NINDS registry?
The NINDS supports and encourages a broad range of basic and clinical research on neurogenetic disorders such as Leigh's disease. The goal of this research is to understand what causes these disorders and then to apply these findings to new ways to diagnose, treat, and prevent them. A registry for individuals with Leigh syndrome has been established at the University of Texas Health Science Center in Houston to collect valuable information about the medical status of patients and to increase understanding of how the disease progresses. The registry will also serve as a resource to researchers conducting clinical trials, speeding up the process of finding potential study subjects. To enroll, see https://peopleagainstleighs.org/registry/. Information from the National Library of Medicine’s MedlinePlusDegenerative Nerve Diseases
What is the genetic mutation of mitochondria?
Genetic mutations in mitochondrial DNA, therefore, result in a chronic lack of energy in these cells, which in turn affects the central nervous system and causes progressive degeneration of motor functions. There is also a form of Leigh’s disease (called X-linked Leigh’s disease) which is the result of mutations in a gene ...
What is the function of mitochondria in Leigh's disease?
The primary function of mitochondria is to convert the energy in glucose and fatty acids into a substance called adenosine triphosphate ( ATP).
What is the phone number for Mitoaction?
Website: https://www.mitoaction.org. Phone: 888-648-6228. Works to improve quality of life for adults and children affected by mitochondrial disease and to raise awareness about mitochondrial disorders and their relationship to other diseases. United Mitochondrial Disease Foundation.
Does dichloroacetate help with lactic acidosis?
Researchers are currently testing dichloroacetate to establish its effectiveness in treating lactic acidosis. In individuals who have the X-linked form of Leigh’s disease, a high-fat, low-carbohydrate diet may be recommended.
What is the best treatment for Leigh disease?
Currently, there is no treatment that is effective in slowing the progression of Leigh disease. Thiamine or vitamin B1 is usually given. Sodium bicarbonate may also be prescribed to help manage lactic acidosis.
What is the treatment for Leigh syndrome?
Treatment for Leigh syndrome is aimed at easing the disease-related symptoms and involves neurologists, pediatricians, clinical geneticists, nurses, and other related caretakers. Psychological counseling and support for family members caring for a child with Leigh disease is often encouraged.
How does Leigh syndrome develop?
In Leigh syndrome, symptoms usually develop within the first year of life; rarely, symptoms can develop during later childhood. The infant usually initially develops symptoms that include hypotonia (decreased muscle tone), vomiting, and ataxia (balance or coordination abnormalities). Overall, failure to grow and thrive is usually the primary reason parents seek medical help. Eventually, the infant experiences seizures , lactic acidosis (an excess of lactic acid, a normal product of carbohydrate metabolism, in the body), and respiratory and kidney impairment.
Why is Leigh syndrome so difficult to diagnose?
In general, diagnosis of Leigh syndrome is often difficult due to the broad variability in clinical symptoms as well as the many different genetic explanations that cause this disease. Genetic testing for specific nuclear or mitochondrial DNA mutation is helpful in this regard.
What is Leigh syndrome?
Leigh syndrome is caused by defective cellular respiration that supplies many tissues with energy. The disorder is severe and can be particularly difficult for family members, as infants are among the severely affected. Leigh syndrome is also known as necrotizing encephalopathy .
Is there a cure for Leigh's disease?
As there is no cure for Leigh disease and the nature of the disorder is rapidly progressive, maintaining function for as long as possible is the primary focus rather than recovery. Physical therapists often assist in exercises designed to maintain strength and range of motion. As the disease progresses, occupational therapists can provide positioning devices for comfort.
What is the Leigh syndrome?
Leigh syndrome (LS), also referred to as subacute necrotising encephalopathy, was first described by the British psychiatrist and neuropathologist Denis Archibald Leigh in 1951. 1 He reported the case of a 7-month-old boy, who presented with progressive neurological symptoms including developmental regression, somnolence, bulbar palsy and spasticity of the limbs. The child was born at term and appeared completely normal until 6 weeks before admission. The disease onset was probably triggered by an infection. Postmortem investigations revealed focal, bilateral symmetrical subacute necrotic lesions, extending from the thalamus to the pons, the inferior olives and the posterior columns of the spinal cord.
When was Leigh syndrome first diagnosed?
However, also late-onset cases have been reported. Since its first description by Denis Archibald Leigh in 1951, it has evolved from a postmortem diagnosis, strictly defined by histopathological observations, ...
What are the hallmarks of a symmetrical lesions in the basal ganglia?
Hallmarks of the disease are symmetrical lesions in the basal ganglia or brain stem on MRI, and a clinical course with rapid deterioration of cognitive and motor functions. Examinations of fresh muscle tissue or cultured fibroblasts are important tools to establish a biochemical and genetic diagnosis.
What is the function of mitochondria?
A key function of mitochondria is to produce energy via the oxidative phosphorylation (OXPHOS) pathway. This process takes place at the inner mitochondrial membrane and is executed by four respiratory chain complexes (reduced nicotinamide adenine dinucleotide (NADH) ubiquinone reductase=complex I, succinate ubiquinone reductase=complex II, ubiquinol cytochrome c oxidoreductase=complex III and cytochrome c oxidase=complex IV). Within the respiratory chain, coenzyme Q10 (ubiquinone) functions as an electron carrier from complex I and II to complex III. The energy released by electrons flowing through the respiratory chain is used to transport protons across the inner mitochondrial membrane. The proton gradient, generated by this translocation, and the ensuing inward-negative mitochondrial membrane potential across the inner mitochondrial membrane provide the driving force for ATP synthesis by complex V (adenosine triphosphate (ATP) synthase). Of note, cells which require high amounts of OXPHOS-derived energy, such as muscle cells and neurons, are specifically vulnerable to mitochondrial dysfunction.
Why are fibroblasts important?
Furthermore, fibroblasts are essential for molecular-genetic testing and prenatal diagnosis of respiratory chain disorders. Nevertheless, muscle manifesting OXPHOS disorders may be less pronounced or even absent in cultured fibroblasts.
What is the POLG gene?
If there is evidence for mtDNA depletion, but mtDNA mutations are not detectable, POLG gene mutations have to be taken into account. This nuclear gene encodes polymerase gamma, a mtDNA polymerase responsible for mtDNA replication and repair. Its deficiency can cause phenotypes like Alper's syndrome and LS. 49.
What are the three groups of mitochondrial disorders?
Here, genetic counselling is essential to divide mitochondrial disorders into three groups: (1) diseases with an identified mutation in a nuclear-encoded gene, (2) diseases with an identified mutation in a mtDNA-encoded gene and (3) diseases with OXPHOS deficiency and unknown genetic cause. 72.
What is Leigh's disease?
Leigh's disease is a rare inherited neurometabolic disorder that affects the central nervous system. This progressive disorder begins in infants between the ages of three months and two years. Rarely, it occurs in teenagers and adults. Leigh's disease can be caused by mutations in mitochondrial DNA or by deficiencies of an enzyme called pyruvate ...
What is an organization dedicated to the welfare of people with epilepsy?
Organizations. National charitable organization dedicated to the welfare of people with epilepsy. Works to ensure that people with seizures are able to participate in all life experiences; to improve how people with epilepsy are perceived, accepted and valued in society; and to promote research for a cure.
What is a NINDS disorder?
NINDS Disorders is an index of neurological conditions provided by the National Institute of Neurological Disorders and Stroke. This valuable tool offers detailed descriptions, facts on treatment and prognosis, and patient organization contact information for over 500 identified neurological disorders.
What is the NINDS research?
The NINDS supports and encourages a broad range of basic and clinical research on neurogenetic disorders such as Leigh's disease. The goal of this research is to understand what causes these disorders and then to apply these findings to new ways to diagnose, treat, and prevent them.
How long do you live with mitochondrial complex IV?
Those with partial deficiencies have a better prognosis, and may live to be 6 or 7 years of age. Some have survived to their mid-teenage years.
How do you know if you have a lactic acid disorder?
The earliest signs may be poor sucking ability,and the loss of head control and motor skills. These symptoms may be accompanied by loss of appetite, vomiting , irritability, continuous crying, and seizures. As the disorder progresses, symptoms may also include generalized weakness, lack of muscle tone, and episodes of lactic acidosis, ...
What is the cause of the lack of energy in mitochondria?
The energy in ATP drives virtually all of a cell's metabolic functions. Genetic mutations in mitochondrial DNA, therefore, result in a chronic lack of energy in these cells, which in turn affects the central nervous system and causes progressive degeneration of motor functions.There is also a form of Leigh’s disease ...

Definition
Description
- The most common treatment for Leigh's disease is thiamine or Vitamin B1. Oral sodium bicarbonate or sodium citrate may also be prescribed to manage lactic acidosis. Researchers are currently testing dichloroacetate to establish its effectiveness in treating lactic acidosis. In individuals who have the X-linked form of Leigh’s disease, a high-fat, l...
Demographics
Causes and Symptoms
Diagnosis
Treatment Team
Treatment
Recovery and Rehabilitation
Clinical Trials
Prognosis