For this reason, they believe that hypertension and renal failure can be significantly improved by performing percutaneous transluminal renal angioplasty (PTRA) with a stent placement as the preferred treatment instead of medical therapy.
What is the end stage of renal disease?
The report highlights the trends prevalent in the global late stage chronic kidney disease drugs market, and the drivers and deterrents pertaining to its growth. Late-stage renal disease, also called end-stage kidney disease, occurs when chronic kidney disease (the gradual loss of kidney function) reaches an advanced state.
What causes high blood pressure in kidneys?
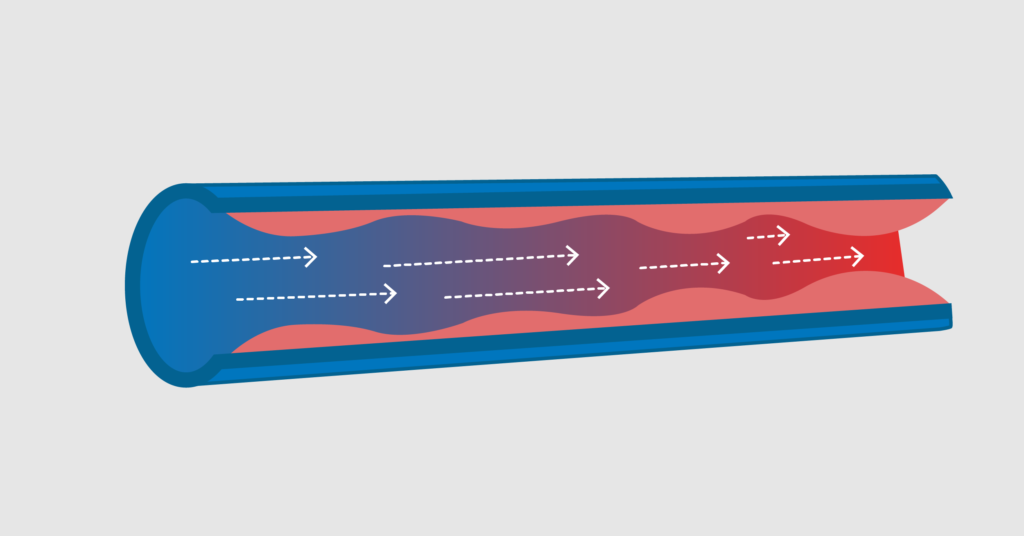
Renal hypertension (or renovascular hypertension) is high blood pressure caused by the narrowing of your arteries that carry blood to your kidneys. It is also sometimes called renal artery stenosis. Because your kidneys are not getting enough blood, they react by making a hormone that makes your blood pressure rise.
What are the symptoms of renal hypertension?
What are the symptoms of high blood pressure and kidney disease?
- loss of appetite, nausea, or vomiting
- drowsiness, feeling tired, or sleep problems
- headaches or trouble concentrating
- increased or decreased urination
- generalized itching or numbness, dry skin, or darkened skin
- weight loss
- muscle cramps
- chest pain or shortness of breath
What are the guidelines for hypertension?
• Use an average threshold of 140/90 mm Hg for office diagnosis of hypertension, but 135/85 mm Hg for home and 130/80 mm Hg for 24-hour ambulatory monitoring. • Initial assessment in a patient who is hypertensive should evaluate for cardiovascular risk and any hypertension-mediated organ damage.

How do you manage hypertension in chronic kidney disease?
The main approaches to the management of hypertension in CKD include dietary salt restriction, initiation of treatment with angiotensin-converting enzyme inhibitors or angiotensin receptor blockers, and diuretic therapy.
What medications treat renal hypertension?
The most important blood pressure medications to treat renal hypertension include:ACE inhibitors(angiotensin converting enzyme inhibitors). These include ramipril, benazepril, captopril, lisinopril, and others.ARBs (angiotensin II receptor blockers). Examples include candesartan, losartan, olmesartan and valsartan.
Which antihypertensive medication is best avoided in chronic kidney disease?
Spironolactone is contraindicated in patients with acute kidney injury and creatinine clearances less than 10 mL/min. Eplerenone, a more selective mineralocorticoid antagonist, is contraindicated for use when creatinine clearance falls less than 30 mL/min.
Which hypertension drug is the first choice for diabetic and renal failure patients?
Renin–angiotensin system inhibitors have been undoubtedly studied the most and are suggested by guidelines and experts as first choice in patients with hypertension and renal injury, particularly in those with diabetes, as they have repeatedly shown to significantly reduce proteinuria.
What is the best blood pressure medicine for CKD?
Blood pressure should be controlled to less than 130/80 if you have CKD. medications for your treatment are angiotensin converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs). an ACE inhibitor or an ARB for you, even if your blood pressure is normal.
What blood pressure medicine is easiest on the kidneys?
ACE inhibitors and ARBs are two types of blood pressure medicine that may slow the loss of kidney function and delay kidney failure. You can tell if you're taking one of these medicines by its generic name.
Is amlodipine safe in renal failure?
The drug was rated as of clinical benefit in 27 of the 35 patients (77.1%), and as slightly beneficial in another 5 patients (14.3%). Thus, amlodipine significantly decreased the blood pressure while causing little or no aggravation of renal dysfunction in hypertensive patients with renal impairment.
What is the first drug of choice for hypertension?
The strongest body of evidence indicates that for most patients with hypertension, thiazide diuretics are the best proven first-line treatment in reducing morbidity and mortality.
Why are loop diuretics preferred in kidney disease?
Loop diuretics in high doses are the drugs of choice in the treatment of both acute renal failure (ARF) and chronic renal failure (CRF). Their pharmacokinetic and pharmacodynamic properties give them a high efficacy, even in severely compromised renal function.
What is the goal of treatment for patients with hypertension and either diabetes or kidney disease?
The essential goals of therapy in the management of diabetic nephropathy are treatment of hypertension and reduction of albuminuria. The presence of microalbuminuria is the first clinical manifestation of renal disease in patients with diabetes.
Why are thiazide diuretics avoided in patients with renal failure?
It is generally thought that thiazides are ineffective in patients with more advanced CKD because of more proximal sodium reabsorption in the nephron. This results in less sodium being delivered to the distal tubule and therefore less thiazide diuretic action in the distal tubule.
Is CKD a cardiovascular disease?
Chronic kidney disease (CKD) is an increasingly prevalent condition globally and is strongly associated with incident cardiovascular disease (CVD). Hypertension is both a cause and effect of CKD and affects the vast majority of CKD patients.
Does HIV cause hypertension?
HIV is associated with an increased prevalence of both hypertension and CKD [131]. In those treated with ART aged > 50 years, more than 50% will be hypertensive, with an approximately four times higher prevalence of microalbuminuria than the general population [132].
Does weight loss help with CKD?
Weight loss is effective in reducing BP and proteinuria and may slow CKD progression [60]. In overweight patients (body mass index [BMI] > 27 kg/m2) with CKD and proteinuria (> 1 g/24 h), a mean weight loss of ~ 4% can reduce proteinuria by ~ 30% [61].
What is the blood pressure for CKD?
The National Kidney Foundation clinical practice guidelines recommend a blood pressure goal of <130 mmHg systolic and <80 mmHg diastolic for all CKD patients.
What is the first line of treatment for non diabetics?
For non-diabetics with less than 200 mg protein/gram creatinine on a random urine sample, no specific first-line drug class is recommended. After initial dosing with an ACEi, ARB or other drug, a diuretic should be added to the regimen.
How many people have kidney disease?
It is estimated that nearly 20 million Americans have some degree of chronic kidney disease defined as an estimated glomerular filtration rate of less than sixty milliliters per minute or evidence of kidney damage by …. Chronic kidney disease (CKD) is a major public health problem in the United States. It is estimated that nearly 20 million ...
How many people have CKD?
Chronic kidney disease (CKD) is a major public health problem in the United States. It is estimated that nearly 20 million Americans have some degree of chronic kidney disease defined as an estimated glomerular filtration rate of less than sixty milliliters per minute or evidence of kidney damage by imaging study, biopsy, ...
Does hypertension cause CKD?
Hypertension is present in more than 80% of patients with CKD and contributes to progression of kidney disease toward end stage (ESRD) as well as to cardiovascular events such as heart attack and stroke. In fact the risk for cardiovascular death in this patient population is greater than the risk for progression to ESRD.
What is the first line of treatment for BP reduction?
Angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), and beta-blockers are reasonable first-line agents for most patients. ACE inhibitors and ARBs exert cardioprotective effects that are independent of BP reduction.
Is antihypertensive medicine considered end stage renal disease?
Antihypertensive Medications in End-Stage Renal Disease. Hypertension is almost universal in end-s tage renal disease (ESRD) and contributes to the substantial cardiovascular (CV) morbidity and mortality observed in these patients.
Can dialysis be used for intradialytic hypotension?
Medications that are removed with dialysis may be preferred in patients who are prone to develop intradialytic hypotension. Intradialytic hypertension can be managed with challenging the patient's dry weight and using nondialyzable medications.