What is CPT code 90837 for Psychotherapy?
Centers for Medicare Services CPT Code 90837 definition: individual outpatient psychotherapy services rendered for 60 minutes. Code 90837: Psychotherapy, 60 minutes with patient and/or family member
What does 90837 stand for?
Code 90834: Psychotherapy, 45 minutes with patient and/or family member • Code 90837: Psychotherapy, 60 minutes with patient and/or family member In general, providers should select the code that most closely matches the actual time spentperforming psychotherapy.
Can I Bill 90837 for a session?
If your session extends beyond 53 minutes, don't shy away from billing for the full session. In order to ensure that your use of the code is justified, first make sure your services are covered. Check your contract with the payer to ensure that 90837 is available for reimbursement, and verify that your client is covered for that service.
What is Section 3 of the PA code 90853?
Section III: Group Psychotherapy (procedure Code 90853) Group Psychotherapy is a form of treatment administered in a group setting with a trained group leader in charge of several patients. Since it involves psychotherapy it must be led by a person, authorized by state statute to perform this service.

What is CPT code 90837 used for?
PsychotherapyKey facts for utilizing psychotherapy codesPsychotherapy CodesCPT® CodeDescriptor90837Psychotherapy, 60 minutes with patient90845Psychoanalysis90846Family psychotherapy (without the patient present), 50 minutes5 more rows
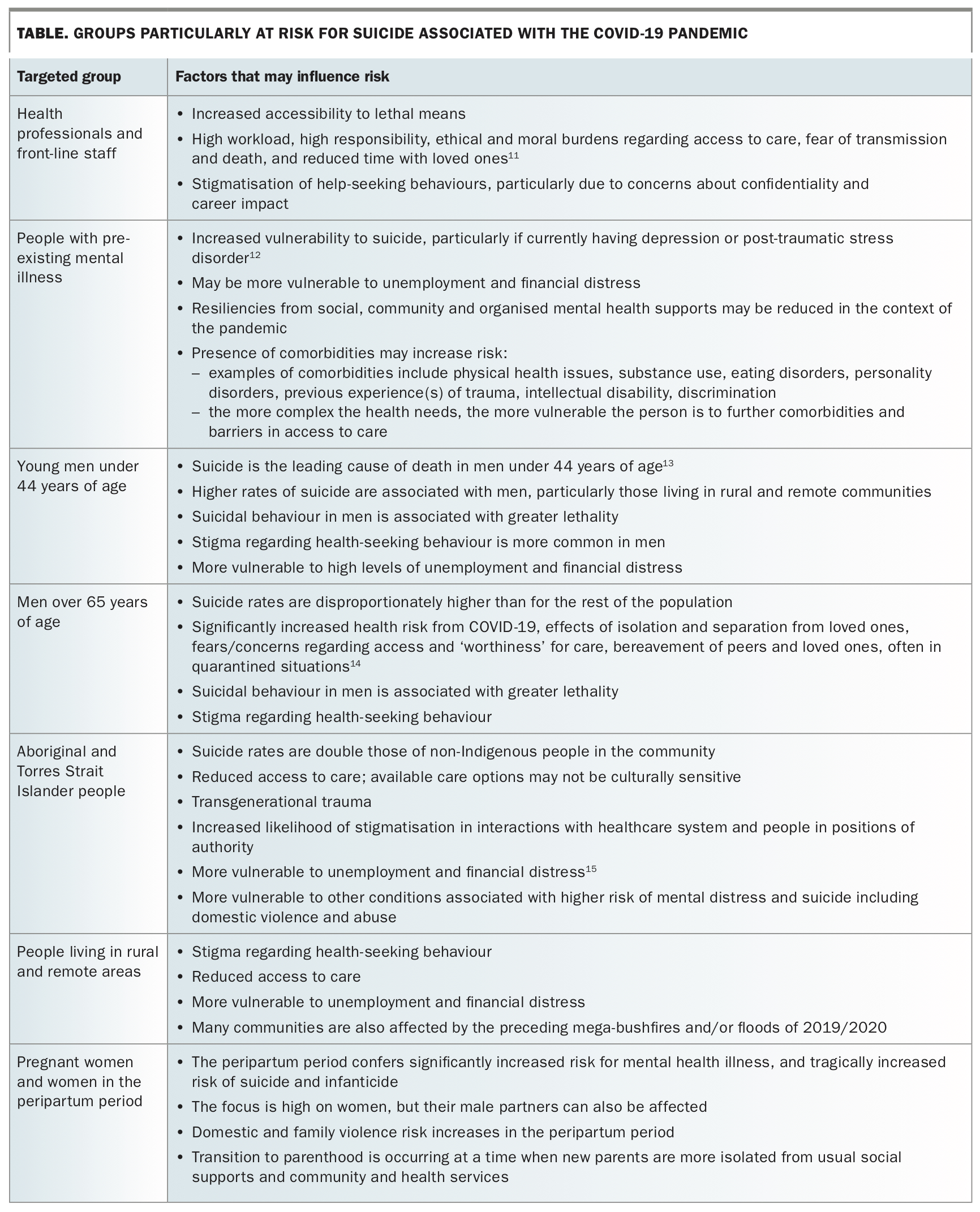
Who can bill for CPT code 90837?
Psychologists who conduct sessions that require more than 60 minutes should report CPT® code 90837: Psychotherapy, 60 minutes with patient. Regardless of how long the session lasts, the psychologist's reimbursement will be based on the payment amount ultimately associated with 90837.
How many minutes is CPT 90837?
60 minutes90837 – Psychotherapy 60 minutes. Some health insurance companies may consider 90834 as the standard psychotherapy session.
Is 90837 a timed code?
The Background Of The 90837 Each of these codes are timed and are well-known to many therapists, as they represent the majority of regularly billed codes, which are the 90832, 90834, and 90837. These, respectively, are described as providing individual psychotherapy for 30 minutes, 45 minutes, or 60 minutes.
How long is a 60 minute therapy session?
How to Bill Extended Sessions for Psychotherapy Over 60 MinutesIndividual Therapy CPT CodeAdd-On CPT Code for Extended SessionServices Rendered90834Psychotherapy, 45 minutes90837Psychotherapy, 60 minutes9083799354Psychotherapy, 1:30 hrs - 2:14 hrs9083799354 99355Psychotherapy, 2:15 hrs - 2:44 hrs4 more rows
Does 90837 require authorization?
CPT code 90837 represents a 60 minute individual therapy session and now requires authorization with UHC.
Can you bill 90837 family session?
The American Medical Association (AMA) clarified in 2016 that CPT codes 90832, 90834, and 90837 were individual therapy codes, and should only be used for a family session if a family member comes once or occasionally into a session where ongoing individual therapy is taking place.
What is the difference between 90837 and 90834?
Both 90834 and 90837 are designed to bill for the same service – psychotherapy. The primary distinguishing factor between the two codes is time; 90834 is defined as 45 minutes of psychotherapy, while 90837 is defined as 60 minutes.
Can you Bill 90837 twice on the same day?
If two psychotherapy sessions took place on the same day, you would add the two and code one claim with the combined time. Since it is 90 minutes, you would code 90837.
How Much Does Medicare pay for 90837?
$132.69What is the difference between the “facility rate” and “nonfacility rate” for telehealth services?CodeService2021 Facility Rate90832Psychotherapy 30-minutes$68.7490837Psychotherapy 60-minutes$132.6996132Neuropsych Test Eval$106.0896158Hlth Bhvr Intrv Indvl$58.971 more row•Dec 10, 2021
What is the difference between 90837 and 90847?
90847 involves family group therapy whereas 90837 is an individual session. The time frame is also different. 90837 sessions must be at least 53 minutes, and 90847 must be at least 26 minutes.
How to get authorization for 90837?
Get authorization from United Health Care for 90837 sessions via a phone call: (800) 888-2998. UHC sets limits on the number of 90837 sessions and provides you a unique authorization number for your approved sessions. File your CMS1500 forms with that auth number! Call before your auth expires for more 90837 sessions.
What is the CPT code for mental health?
United Health Care, Optum, and United Behavioral Health (UBH) have set limits for CPT code 90837 used by mental health outpatient providers. CPT code 90837 represents a 60 minute individual therapy session and now requires authorization with UHC.
Does UHC require authorization for 90834?
UHC does not require authorization for CPT code 90834, a 45 – 55 minute individual therapy session. If you file to UHC with 90837 without authorization, your claim may be denied.
Overview
The clinical examples and their procedural descriptions, which reflect typical clinical situations found in the health care setting, are included in this text with many of the codes to provide practical situations for which the codes would be appropriately reported.
Typical patient description
An adult undergoes psychotherapy due to anxiety and depressive symptoms. Psychosocial stressors at work and home have increased anxiety and depression since a recent hospital discharge.
Care components
During the visit, face-to-face therapeutic communication is conducted with the patient and/or the patient's family. Objective information and an interval history are obtained.
About the CPT code set
Medical knowledge and science are constantly advancing, so the CPT Editorial Panel manages an extensive process to make sure the CPT code set advances with it.
Coding Education Audit (TPE)
Medicare Administrative Contractors (MACs) conduct Medicare TPE audits of psychotherapists billing practices, utilization rates, or potential claim error rates that vary from their peers. TPE audits are also used to intervene and influence psychotherapist billing for services that have high national rates.
Risk Adjustment Audits
Risk Adjustment Audits are conducted annually and are required of commercial health plans by the Federal Department of Health and Human Services (HHS). Risk Adjustment Audits come in a letter usually from a contractor acting on behalf of a Healthplan under the authority of HHS. The audits are required by HHS to assess a risk pool of insurers.
Abuse & Waste Audits
A reviewer, during an abuse audit, is examining a patient’s medical records and comparing those to the associated billing. The purpose is to look for waste, overcharging, or fraud. These audits are usually initiated based on information provided by 3rd party auditors, employees or patients.
Record Review Audits (record keeping)
An auditor, during a record review audit, examines patients’ medical records for completeness. The focus is on identifying records that are incomplete rather than on their quality. The auditor is not trained or tasked to audit for waste or abuse. At most, they are looking for patterns that may constitute negligent behavior.
Recovery Audit
Recovery Audit Contractors (RAC) are companies contracted by CMS to identify Medicare overpayments and underpayments and to return Medicare overpayments to the Medicare Trust Funds. RACs review claims submitted in an attempt to identify improper payments.
Medical Necessity is an Important Element of Audits
A functional definition of medical necessary services is documentation in the patient’s medical record concluding that…
Commercial Healthplan (Private Payor) Audits
Psychotherapists may find themselves subject to third-party payor audits by commercial insurers. These audits are similar to those conducted by the Center for Medicare and Medicaid (CMS). The audit process will vary depending on the third-party payor.
What is CPT code 90837?
• Code 90837: Psychotherapy, 60 minutes with patient and/or family member In general, providers should select the code that most closely matches the actual time spentperforming psychotherapy . CPT® provides flexibility by identifying time ranges that may be associated with each of the three codes:
Is psychotherapy an integral part of treatment?
Psychotherapy must be provided as an integral part of an active treatment plan for which it is directly related to the patient’s identified condition/diagnoses. Some patients receive psychotherapy alone, and others receive psychotherapy along withmedical evaluation and management services.
Is a psychotherapy code dependent on the location?
Psychotherapy codes are no longer dependent on the service location (i.e., office, hospital, residential setting, or other location is not a factor). However, effective January 1, 2014, when E&M services are paid under Medicare’s Partial Hospitalization Program (PHP) and not in the physician office setting, the CPT outpatient visit codes ...
Is psychotherapy considered medically reasonable?
Psychotherapy services are not considered to be medically reasonable and necessary when they primarily include the teaching of grooming skills, monitoring activities of daily living, recreational therapy (dance, art play), or social interaction. Psychotherapy times are for face-to-face services with the patient.
What is the code for prolonged therapy?
For psychotherapy sessions lasting 90 minutes or longer, the appropriate prolonged service code should be used (99354-99357). The duration of a course of psychotherapy must be individualized for each patient. Prolonged treatment may be subject to medical necessity review.
When should a psychotherapy code not be billed?
A psychotherapy code should not be billed when the service is not primarily a psychotherapy service, that is, when the service could be more accurately described by an evaluation and management or other code. The duration of a course of psychotherapy must be individualized for each patient.
What is psychotherapy services?
Psychotherapy services include ongoing assessment and adjustment of psychotherapeutic interventions and may include involvement of family member (s) or others in the treatment process.
What is the major concept and addition to the psychotherapy section?
A major concept and addition to the psychotherapy section is the addition of codes for psychotherapy for crisis when psychotherapy services are provided to a patient who presents in high distress with complex or life threatening circumstances that require immediate attention.
What is the treatment of mental illness?
Psychotherapy is the treatment of mental illness and behavior disturbances, in which the provider establishes a professional contact with the patient and through therapeutic communication and techniques, attempts to alleviate the emotional disturbances, reverse or change maladaptive patterns of behavior, facilitate coping mechanisms and/or encourage personality growth and development.
What is the procedure code for psychoanalysis?
Description: Procedure code 90845 involves the practice of psychoanalysis using special techniques to gain insight into and treat a patient’s unconscious motivations and conflicts using the development and resolution of a therapeutic transference to achieve therapeutic effect. It is a different therapeutic modality than psychotherapy.
Is behavior modification a separate service?
Behavior modification is not a separate service , but is an adjunctive measure in psychotherapy. Additionally, a periodic summary of goals, progress toward goals, and an updated treatment plan must be included in the medical record. Prolonged treatment must be well supported by the content of the medical documentation.
What is CPT code 90837?
Payers including Highmark BCBS and Anthem have sent letters to providers who they deem to be high submitters of CPT code 90837 with a warning that claims billed as 90837 could be subject to additional review and re-submission requirements. While the payers emphasized that these letters are meant to be educational, many providers interpreted their warnings as imminent threats against the use of 90837.
What to do if you are denied 90837?
If you are denied the ability to bill 90837, talk to your insurance provider representative or have your client call their member services representative.
How long is 90834?
As defined by the CPT, 90834 should be used when you spend an estimated 38–52 minutes on therapy with the client, and 90837 is for all therapy sessions that are at least 53 minutes long.
Does Highmark reimburse 90837?
Nevertheless, some providers have been reporting difficulty getting reimbursed for 90837. YouTube.