What are the treatment options for post-thrombotic syndrome?
Compression is the main treatment for post-thrombotic syndrome. This helps to increase the blood flow in your veins, and decrease your symptoms. You may be given prescription-grade compression stockings. These apply more pressure than the type you can buy over-the-counter. These are worn during the day, on the leg that had the DVT.
What is the prognosis of post-thrombotic syndrome (PTS)?
Post-thrombotic syndrome, recurrence, and death 10 years after the first episode of venous thromboembolism treated with warfarin for 6 weeks or 6 months. Below-knee elastic compression stockings to prevent the post-thrombotic syndrome: a randomized, controlled trial.
What is post thrombotic syndrome?
Post-Thrombotic Syndrome. Overview. Post-thrombotic syndrome (PTS) is a long-term condition that occurs as a result of a deep vein thrombosis (DVT). The veins in our arms and legs have small valves inside that ensure the blood flows correctly back toward the heart.
What are the treatment options for post-thrombotic venous ulcers?
Post-thrombotic venous ulcers are treated with compression therapy, leg elevation, topical dressings and sometimes hemorheological agents like pentoxifylline but can be refractory to therapy and tend to recur. Guidance Statement
Is post-thrombotic syndrome permanent?
Symptoms can come and go over time, but PTS is a chronic, lifelong condition. PTS leads to suffering and disability and is costly to society. Severe PTS can cause painful venous ulcers or sores on the arms or legs that are difficult to treat and tend to recur.
Can you recover from post-thrombotic syndrome?
Approximately 60% of patients will recover from a leg DVT without any residual symptoms, 40% will have some degree of post-thrombotic syndrome, and 4% will have severe symptoms. The symptoms of post-thrombotic syndrome usually occur within the first 6 months, but can occur up 2 years after the clot.
How long does post-thrombotic syndrome last?
It usually affects veins in your leg, but it's also possible in your arm. Signs of the condition, like skin ulcers on your leg or swelling, can be painful or uncomfortable. They can happen a few months or up to 2 years after you have DVT. They could last for years or stick around for good.
Does exercise help post-thrombotic syndrome?
The authors conclude that exercise does not increase symptoms in patients with post-thrombotic syndrome and improves flexibility in the affected leg. Treadmill or similar exercise is not likely to worsen symptoms related to post-thrombotic syndrome.
Is massage good for post-thrombotic syndrome?
While there is nothing physically preventing you from going and getting a massage if you have deep vein thrombosis, it is not advisable. The small blood clots that cause your deep vein thrombosis could break loose. When this happens it can cause serious, potentially fatal health problems such as a pulmonary embolism.
Does vein scar tissue go away?
Eventually, the vein will become scar tissue and disappear.
How long does it take for a blood clot to go away with blood thinners?
After being stopped, warfarin takes 5–7 days to clear the body. Takes 24 to 48 h to clear after being stopped.
What happens when you stop taking blood thinners?
One of the major risks is that blood clots may begin to form, which could lead to a stroke and a lack of oxygen to the brain. This could also potentially lead to partial paralysis or even death. Stopping a blood-thinning drug suddenly can also raise the risk for a blood clot in the brain, which is often fatal.
Do blood clots ever go away?
Blood clots can also cause heart attack or stroke. Blood clots do go away on their own, as the body naturally breaks down and absorbs the clot over weeks to months. Depending on the location of the blood clot, it can be dangerous and you may need treatment.
Can you wear compression socks while on blood thinners?
Blood thinners can cause serious bleeding problems. Try to walk several times a day. Wear compression stockings if your doctor recommends them. These stockings are tighter at the feet than on the legs.
How can I improve my circulation after DVT?
Take a Quick Motion Break Every Hour. A great solution to having to sit still all day is to take a quick break every hour. Get up and walk around for a few minutes or stretch out your legs. Regular activity will help improve your circulation.
Why does Post-Thrombotic Syndrome occur?
Post-thrombotic syndrome, or PTS, is a serious and painful condition that can last a long time. It occurs because of deep vein thrombosis (DVT). The veins found in your legs and arms have small valves inside that help ensure the blood flows in the proper direction, back to the heart.
What is the best treatment for post thrombotic syndrome?
Compression is the main treatment for post-thrombotic syndrome. This helps to increase the blood flow in your veins, and decrease your symptoms. You may be given prescription-grade compression stockings. These apply more pressure than the type you can buy over-the-counter.
What is post thrombotic syndrome?
Key points about post-thrombotic syndrome. Post-thrombotic syndrome is a condition that can happen to people who have had a deep vein thrombosis (DVT) of the leg. It can cause chronic pain, swelling, and other symptoms in your leg. It may develop in the weeks or months following a DVT.
What test is used to check for clotting problems in the leg?
You may also need some tests, such as: Ultrasound. This is done to look for problems with the leg vein valves. Blood test. This is done to check for clotting problems with your blood. Healthcare providers often use something called a Villalta score to assess post-thrombotic syndrome.
What are the symptoms of a DVT?
Symptoms of infection of an ulcer on your leg (heat, redness, warmth, fluid leakage, or a fever) Symptoms of DVT, such as leg swelling, pain, or warmth.
What is the best treatment for leg sores?
Barrier creams that contain zinc oxide can also be helpful. In some cases, you may need a steroid cream or ointment to treat your skin. If you develop leg sores (ulcers), they may need special treatment.
What are the risks of getting a DVT?
A variety of conditions can increase your chance of getting a DVT, such as: Recent surgery, which decreases your mobility and increases inflammation in the body, which can lead to clotting. Medical conditions that limit your mobility, such as an injury or stroke. Long periods of travel, which limit your mobility. Injury to a deep vein.
Is DVT a common condition?
DVT is a common condition, especially in people over age 65. Post-thrombotic syndrome affects a large number of people who have had DVT. It can happen in men and women of any age.
What is post thrombotic syndrome?
Post-thrombotic syndrome (PTS) is a common late complication of lower extremity deep vein thrombosis (DVT). 1 The incidence of PTS is approximately 40% in adult patients with a symptomatic first episode DVT within two years. 2 Manifestations of PTS include chronic lower extremity pain, swelling, heaviness and/or fatigue, which may progress to stasis dermatitis or limb ulceration in a minority of patients. 1,2 Patients with advanced PTS suffer major physical limitations and impairment of health-related quality of life (QOL). 3 Advanced PTS symptoms include severe pain, uncontrolled edema, venous ulcers and short-distance claudication. Venous ulcers contribute to marked impairments in QOL, rise in healthcare costs, predisposition to infections and the need for endovascular or surgical interventions. 4,5
What is PCDT in DVT?
Pharmacomechanical catheter-directed thrombolysis (PCDT) refers to the use of CDT in conjunction with a device used to aspirate/macerate thrombus, enabling faster treatment. The ATTRACT (Acute Venous Thrombosis: Thrombus Removal with Adjunctive Catheter-Directed Thrombolysis) trial was developed to determine if PCDT prevents PTS after acute proximal lower extremity DVT. The trial compared the first-line use of PCDT along with standard therapy versus standard therapy alone in 691 patients. 13 In this study, PCDT 1) had no effect on the development of PTS over two years; 2) reduced the severity of PTS over two years; 3) decreased the degree of leg pain and swelling within the first month after treatment; and 4) increased major bleeding within 10 days of treatment (absolute risk difference 1.4%). 14 The study investigators concluded that PCDT should not be used routinely as first-line DVT therapy. However, selective use to reduce PTS severity may be justified in highly symptomatic patients <65 years of age with low expected risk of bleeding who respond poorly to initial anticoagulant therapy. Those with iliofemoral DVT will most likely comprise a subgroup that benefits, since these patients have a higher baseline risk for PTS and are more likely to exhibit poor symptom response to initial anticoagulation. Furthermore, based on clinical experience, PCDT is recommended as first-line therapy for patients with DVT causing acute limb-threatening circulatory compromise. 15
Is PTS a complication of DVT?
PTS is a common, late complication of DVT, which causes significant morbidity and im pairs QOL. The best methods to prevent PTS are the primary prevention of DVT and ensuring optimal anticoagulant therapy after DVT. ECS may improve symptoms among those with edema, but are unlikely to prevent PTS.
Can a catheter eliminate a thrombus?
Preliminary studies suggest that catheter-directed endovascular therapies can rapidly eliminate thrombus and resolve venous obstruction. Catheter-directed thrombolysis (CDT), in which a recombinant tissue plasminogen activator is infused into the thrombus via a multi-sidehole catheter, was studied in the CaVenT (Catheter-Directed Venous Thrombolysis in Acute Iliofemoral Vein Thrombosis) study, a multicenter open-label RCT that included 189 patients. This study demonstrated a 26% reduction (55.6% vs. 41.1%; p = 0.047) in the risk of developing PTS over two years' follow-up in patients with iliac and/or upper femoral DVT who underwent CDT in addition to anticoagulation and compression, compared with anticoagulation and compression alone. However, there was no difference in long-term venous disease-specific or general health-related quality of life. 12
How long does post thrombotic syndrome last?
The symptoms of post-thrombotic syndrome can persist for months to years. For some people, symptoms remain mild and stable. For others, the condition can progress to the point of disablement. Fortunately, with good treatment, most patients are able to compensate for their symptoms and live healthy, active lives.
What percentage of people have post thrombotic syndrome?
Population and Demographics and Risk Factors. Post-thrombotic Syndrome is a condition that affects around 50% of people who have had a deep vein thrombosis, or DVT, or the legs. Risk factors for post-thrombotic syndrome are still being studied but there are some criteria we can use to help predict who is most at risk.
What happens if you don't take blood thinners for DVT?
Post thrombotic syndrome typically occurs after someone has dealt with DVT. Usually, the condition occurs if the individual is not engaging in the proper treatment for DVT, such as taking blood thinners or wearing compression stockings. However, it can occur in other situations, too.
How to tell if you have DVT?
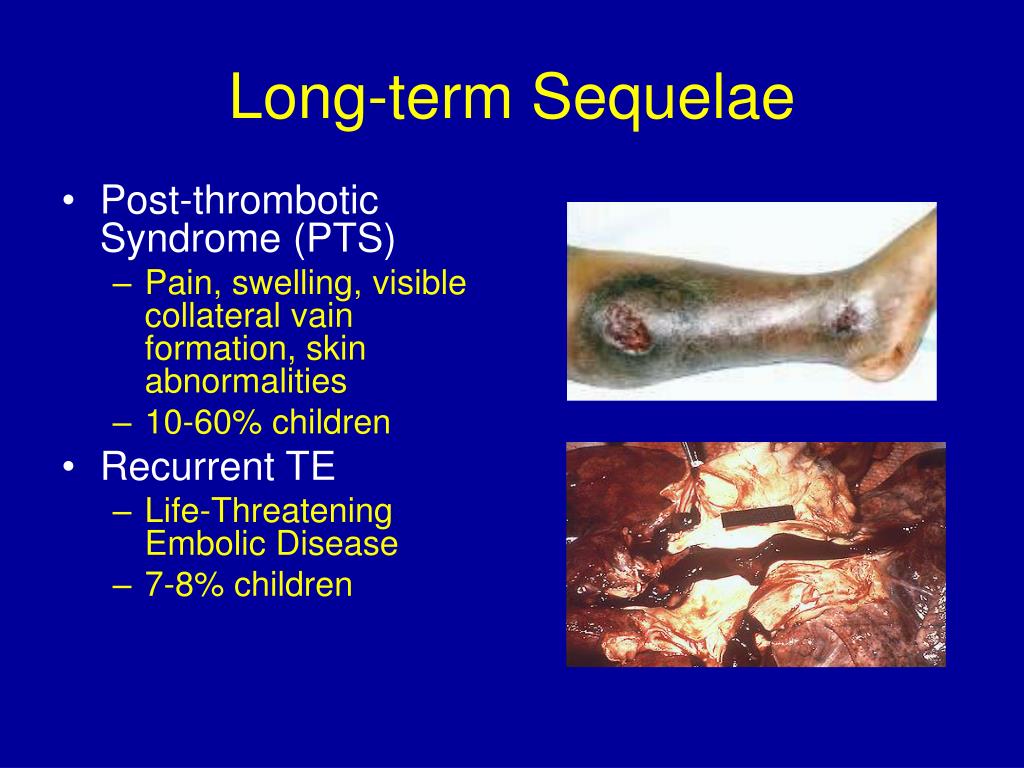
Sometimes, cases of post-thrombotic syndrome only cause a few minor symptoms. However, in other situations, it may cause serious symptoms. Usually, the symptoms appear in the same leg affected by DVT. Some of the most common include: 1 Redness or darkening of affected skin on the leg 2 The feeling of heaviness in the leg 3 Leg swelling 4 Cramping, tingling, or itching in the leg 5 Widening of the veins in the leg 6 Leg pain that becomes worse when standing and better when raising or resting the leg 7 Sores or Leg Ulcers
What happens if you have a DVT?
If the valves are damaged, blood may begin to flow the wrong way. This is referred to as reflux, and it causes pressure to start building up in your veins in the lower portion of your legs. This is what causes discomfort and swelling. The vein walls may also be scarred and damaged after a DVT occurs.
What is the name of the condition that can last a long time?
Post-thrombotic syndrome, or PTS, is a serious and painful condition that can last a long time. It occurs because of deep vein thrombosis (DVT). The veins found in your legs and arms have small valves inside that help ensure the blood flows in the proper direction, back to the heart. If DVT occurs, it means there is a clot or blockage in the way ...
Why is it important to treat DVT?
Receiving prompt diagnosis and treatment for a DVT is needed to help prevent this damage from occurring . After the walls and valves in the vein have been damaged, there is no way to repair them. The valves in your veins are needed to make sure blood is flowing upward, toward your heart.
ABSTRACT
The treatment of symptomatic postthrombotic syndrome is a difficult, evolving, and lifelong undertaking. This chronic disease is not only characterized by the possibility of leg ulcer formation, but more often disabling pain and swelling with minimal skin changes.
INTRODUCTION
Symptoms in patients with a previous history of deep venous thrombosis (DVT) may vary from minimal swelling to pain, skin changes, and venous ulcerations. Compression therapy is still considered by many to be the cornerstone of management of not only post-thrombotic symptoms, but of all venous disease.
INVASIVE TREATMENT OF VENOUS OBSTRUCTION
Venous outflow obstructions are often observed following acute deep vein thrombosis due to subsequent absent or poor venous recanalization.
FEMORO-ILIO-CAVAL STENTING
The introduction of percutaneous iliac venous balloon dilation and stenting has dramatically changed the treatment of the iliofemoral outflow obstruction. The endovascular technique has emerged as the efficient “method of choice” to relieve at least proximal iliofemoral obstruction.
OPEN BYPASS SURGERY
A crossover bypass can be constructed by using either the contralateral saphenous vein (either by rotation or as a free saphenous graft) or a prosthetic graft.
CORRECTION OF REFLUX
The only objective means of measuring advanced postthrombotic disease is to estimate the ulcer healing rate and ulcer recurrence rate in the presence of ulcer. It is much more difficult to objectively assess ulcer-free limbs for improvement in swelling, discoloration, pain, and discomfort.
ABLATION OF SUPERFICIAL REFLUX
There are several methods for the treatment of truncal and nontruncal superficial reflux. It is generally accepted that liquid compression sclerotherapy is effective in the treatment of venectasias and nontruncal varicosities in the absence of GSV or short saphenous vein (SSV) trunk reflux.
What are the long term effects of DVT?
Postphlebitic syndrome is a chronic condition characterized by leg swelling, pain, edema, venous ectasia, and skin induration.
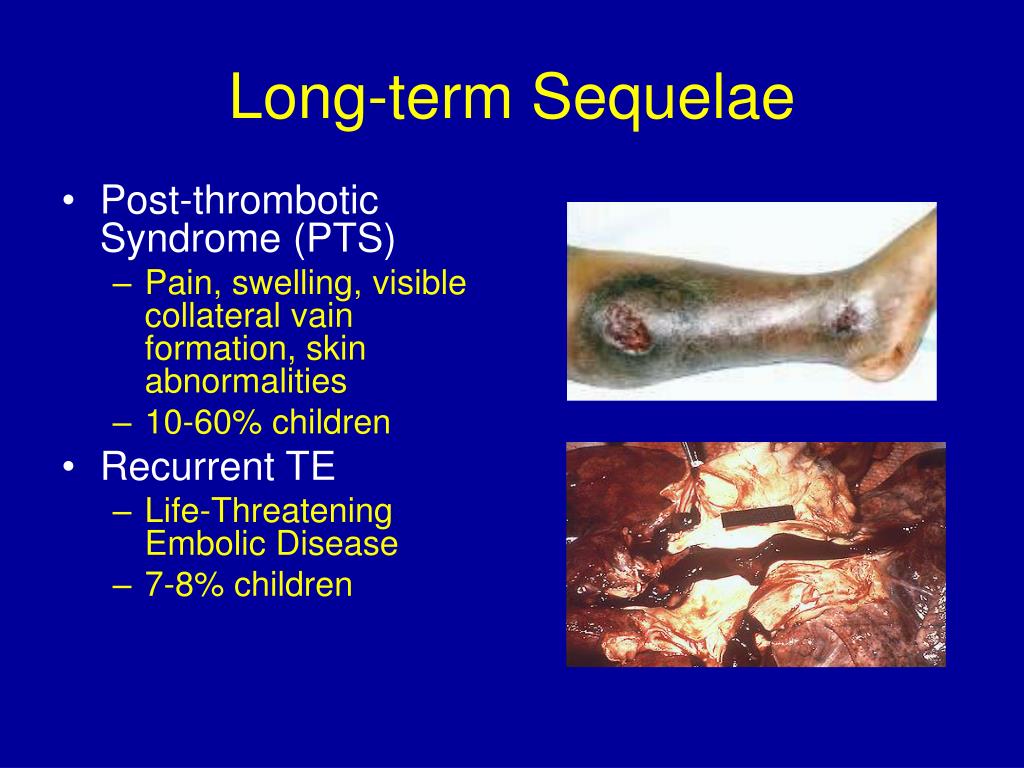
How long does it take for a DVT to manifest?
Studies have shown that it usually manifests itself within the first 2 years after an episode of DVT.2,3Severe postphlebitic syndrome can lead to intractable venous leg ulcers, which are painful, decrease mobility, and require ongoing medical and nursing care.
What are the factors that predict postphlebitic syndrome?
Factors predictive of postphlebitic syndrome in retrospective studies have included age, female gender, hormone therapy, varicose veins, and abdominal surgery. However, for some of these “predictors,” the temporality of the association is questionable (e.g., varicose veins, as prior DVT may lead to secondary varicose veins).
What does a postphlebitic score of 15 mean?
A score of 5 to 14 on 2 consecutive visits 6 months apart indicates mild or moderate postphlebitic syndrome, and a score of 15 or more or the presence of a venous ulcer indicates severe postphlebitic syndrome.
How long does it take for postphlebitis to manifest?
Despite the long-held belief that it takes 5 to 10 years for postphlebitic syndrome to manifest, these 2 studies showed that most cases become clinically apparent within the first 1 to 2 years of the acute DVT. Risk Factors for Postphlebitic Syndrome.
Is postphlebitic syndrome comparable to DVT?
A limited number of studies have prospectively measured the incidence of postphlebitic syndrome after DVT, and these are not directly comparable because of differences in follow-up time, patient selection, and definition of postphlebitic syndrome.
What is post thrombotic syndrome?
Postthrombotic syndrome (PTS) is a chronic complication of deep venous thrombosis (DVT) that reduces quality of life and has important socioeconomic consequences. More than one-third of patients with DVT will develop PTS, and 5% to 10% of patients will develop severe PTS, which may manifest as venous ulceration.
How to treat postthrombotic ulcers?
Postthrombotic venous ulcers are generally treated conservatively with compression bandages or stockings, leg elevation, topical dressings , and various pharmacologic compounds, but they can be refractory to therapy and tend to recur. Patients with ulcers should be managed by a specialist with expertise in managing postthrombotic ulcers. Depending on the center, this may include dermatologists, internists, or vascular or plastic surgeons. Surgery may be advocated in select patients when ulcers do not respond to conservative treatment. Although detailed discussion of the management of venous ulcers is beyond the scope of this article, the interested reader is referred to recent reviews or guidelines that have addressed this topic. 11, 56, 73
What is PTS research?
PTS is a relatively untapped area of venous thrombosis research , and research needs are substantial. Important subjects for future investigation include better elucidation of the pathophysiology of PTS; identification of clinical, anatomic, physiologic, and genetic risk factors for PTS; and development of PTS risk prediction models that integrate clinical and biomarker information. Further work to investigate the association between inflammation and PTS could lead to identification of new therapeutic targets for preventing PTS after DVT. Finally, rigorous evaluation of the long-term effectiveness and safety of catheter-directed thrombolytic techniques to prevent PTS as well as endovascular or surgical procedures to treat moderate-to-severe PTS is required.
What is PTS in the upper extremity?
74, 75 Upper-extremity PTS is a potentially disabling condition that adversely affects quality of life, particularly if the dominant arm is involved. 76 Symptoms include arm swelling, heaviness, and fatigue with exertion. 75, 76 On examination, dilation of the superficial veins of the upper arm and chest wall, as well as dependent cyanosis of the arm, may be noted. To date, no controlled studies have evaluated the effectiveness of elastic bandages, compression sleeves (as are used for lymphedema), or venoactive drugs to prevent or treat PTS after upper-extremity DVT. Anecdotal evidence suggests that patients with persistent arm swelling and pain after upper-extremity DVT may derive symptomatic relief from elastic bandages or compression sleeves. 56 Because these are unlikely to cause harm, they should be tried.
What is DVT in medical terms?
Deep vein thrombosis (DVT) is a common vascular condition that is associated with significant rates of morbidity and mortality. Although pulmonary embolism and recurrent venous thrombosis are well-known consequences of DVT, an important, underappreciated, chronic consequence of DVT is postthrombotic syndrome (PTS).
What is PTS in a patient?
Postthrombotic syndrome (PTS) is a chronic complication of deep venous thrombosis (DVT) that reduces quality of life and has important socioeconomic consequences. More than one-third of patients with DVT will develop PTS, and 5% to 10% of patients will develop severe PTS, which may manifest as venous ulceration. The principal risk factors for PTS are persistent leg symptoms 1 month after the acute episode of DVT, extensive DVT, recurrent ipsilateral DVT, obesity, and older age. Daily use of elastic compression stockings (ECSs) for 2 years after proximal DVT appears to reduce the risk of PTS; however, there is uncertainty about optimal duration of use and compression strength of ECSs and the magnitude of their effect. The cornerstone of managing PTS is compression therapy, primarily using ECSs. Venoactive medications such as aescin and rutoside may provide short-term relief of PTS symptoms. The likelihood of developing PTS after DVT should be discussed with patients, and symptoms and signs of PTS should be monitored during clinical follow-up. Further studies to elucidate the pathophysiology of PTS, to identify clinical and biologic risk factors, and to test new preventive and therapeutic approaches to PTS are needed to ultimately improve the long-term prognosis of patients with DVT.
How to treat PTS?
Endovascular or surgical treatment of PTS 1 Prevent index DVT with the use of thromboprophylaxis in high-risk patients and settings as recommended in evidence-based consensus guidelines. 2 Prevent recurrent ipsilateral DVT by providing anticoagulation of appropriate intensity and duration for the initial DVT and by targeted use of appropriate thromboprophylaxis if long-term anticoagulation is discontinued. 3 Use of knee-length, 30- to 40-mm Hg ECS elastic compression stockings for up to 2 years after DVT; optimal duration uncertain. 4 The role of thrombolysis for the prevention of PTS is not yet established. Catheter-directed thrombolytic techniques require further evaluation in properly designed trials before being endorsed as effective and safe in reducing the risk of PTS.

Causes
- The primary cause of PTS is when the valves and walls of the veins become damaged as a result of a DVT. Prompt diagnosis and treatment of a DVT is necessary to prevent this damage from occurring, as once the valves and walls of the vein are damaged, they cannot be repaired.
Clinical significance
- Vein valves are necessary to ensure that the blood flows in an upward direction toward the heart. They are incredibly fragile and can become damaged easily. When valves are damaged, blood can flow the wrong way. This is called reflux. It causes pressure to build up in the veins in the lower part of our legs, which leads to swelling and discomfort. The walls of the vein can also become …
Symptoms
- Eventually, this can cause damage to the skin on the leg. It becomes dry around the ankles, discoloured, and itchy. It later becomes brown in colour, hard, and leathery to touch. A minor abrasion can then become a larger sore that doesnt heal. This is called a venous ulcer. The most usual symptoms of PTS are:
Diagnosis
- If you develop any of these symptoms, particularly if you know youve had a recent DVT, you should see your doctor as soon as possible. Your doctor can diagnose PTS on the basis of these symptoms. There are no diagnostic tests.
Treatment
- Treatment options differ depending on how severe the condition is. Treatment usually includes elevation of the affected limb, exercise, and compression therapy or stockings. Doctors can also prescribe blood-thinners, to prevent any further clots forming in the veins, and pain medication. …
Prognosis
- The complications of PTS are often developed when the condition isnt promptly treated and effectively managed. When leg ulcers develop, they are incredibly difficult to heal and can become infected. This threatens your mobility and in rare cases can lead to sepsis. PTS is a long-term condition that is difficult to treat and manage. It usually causes discomfort and can lead to great…
What Is Post-Thrombotic Syndrome?
Population and Demographics and Risk Factors
Causes of The Disease
Signs and Symptoms
Diagnosis
Treatment
- Post thrombotic syndrome treatment is based on the severity of your condition. Usually, treatment will include elevating the affected leg, the use of compression stockings or therapy, and exercise. Doctors may also prescribe you blood thinners to help prevent any more clots from showing up in the veins, along with pain medication. Exercise and Elev...
Intervention
Prognosis
Prevention
Disease Progression