
Healthline.com
1. Psyllium seed/husk...
2. Boswellia...
3. Bromelain...
4. Probiotics...
5. Turmeric...
6. Gingko biloba...
Learn More...Top10homeremedies.com
1. Olive Oil...
2. Aloe Vera...
3. Wheat Grass Juice...
4. Fish Oil...
5. Slippery Elm...
6. Psyllium Seeds...
7. Calendula...
8. Fenugreek...
Learn More...Everydayhealth.com
1. Avoid Foods That May Exacerbate UC Symptoms...
2. Get Regular Exercise to Reduce UC Inflammation...
3. Stress Less to Aid Digestion Problems in UC...
4. Consider Therapy to Help Manage Stress and Pain...
5. Consider Omega-3 Fatty Acids to Ease Symptoms...
6. Experiment With Herbal Remedies for Ulcerative Colitis...
Learn More...Homeremedyshop.com
1. Cut Refined Carbohydrates...
2. Probiotic Foods...
3. Licorice Root...
4. Hemp Seed Oil...
5. Cod Liver Oil...
6. Aloe Vera...
7. Boswellia...
8. Olive Oil...
Learn More...Trueremedies.com
1. Turmeric...
2. Gingko Biloba...
3. Boswellia...
4. Bromelain...
5. Probiotics...
6. Aloe Vera...
7. Psyllium Seed / Husk...
8. Olive Oil...
Learn More...What are the natural remedies for ulcerative colitis?
Supplements and herbal remedies for ulcerative colitis
- Probiotics. Probiotics introduce healthy gut bacteria to restore and maintain a natural microbial flora in the gut.
- Ginseng. Although there is a lack of human research studying how ginseng affects UC, some animal studies have shown that ginseng may be effective in the treatment of UC by ...
- Psyllium seed/husk. ...
- Boswellia. ...
- Bromelain. ...
- Turmeric. ...
- Gingko biloba. ...
Will natural remedies ease ulcerative colitis?
UC may also affect a person’s general health and quality of life, such as:
- lack of appetite
- weight loss
- nausea
- fatigue
- fever
- low red blood cell count ( anemia)
- delayed growth and development in children
What is the best antibiotic for colitis?
ulcerative colitis, inflammation can develop in the pouch (pouchitis). Pouchitis is often effectively managed with antibiotics. Medication Details Although there are several antibiotics that may be effective, the most commonly prescribed in IBD are: • Metronidazole (Flagyl®) • Ciprofloxacin (Cipro®) • Vancomycin (Vancocin®)
What medication is used to treat colitis?
Ulcerative Colitis Medication
- Aminosalicylates. This group of medication contains a chemical compound called 5-aminosalicylate acid. ...
- Corticosteroids. These medicines, also known simply as steroids, are typically used to treat flares of ulcerative colitis.
- Immunomodulators. ...
- Biologics. ...
- Janus Kinase (JAK) Inhibitors. ...
- Antibiotics. ...
What is the goal of ulcerative colitis?
What is the best medicine for UC?
When was Infliximab approved?
What is a fecal transplant?
Why is a colon removed after a colonectomy?
Does methotrexate help with UC?
See more
About this website
What is the most effective treatment for ulcerative colitis?
Balsalazide, mesalamine, olsalazine, and sulfasalazine are the main medications used to treat ulcerative colitis. They come in pills and suppositories. Let your doctor know if you are allergic to sulfa before taking one of these drugs. They can prescribe a sulfa-free 5-ASA.
What is the new treatment for ulcerative colitis?
Taken daily as a capsule, ozanimod is the first in a class of drugs known as “sphingosine 1-phosphate receptor modulators” to be approved for ulcerative colitis. The drug works by acting on certain types of immune cells called lymphocytes that are centrally involved in the autoimmune attack on the large intestine.
How close is a cure for ulcerative colitis?
Right now, there's no medical cure for UC. Current medical treatments aim to increase the amount of time between flare-ups and to make flare-ups less severe. This may include a variety of medications or surgeries.
What is the safest treatment for ulcerative colitis?
Aminosalicylates. Aminosalicylates, also known as 5-ASAs, are medicines that help to reduce inflammation. This in turn allows damaged tissue to heal. They're usually the first treatment option for mild or moderate ulcerative colitis.
What is the latest treatment for ulcerative colitis 2021?
Federal regulators have approved the new drug Zeposia for treating moderate to severe ulcerative colitis in adults. The medication is the latest in a line of drugs used to treat symptoms of this particular type of inflammatory bowel disease (IBD).
What is the latest research on ulcerative colitis?
New and upcoming treatments Xeljanz is a Janus kinase (JAK) inhibitor that blocks certain proteins involved in inflammation. It is 34.3% to 40.6% effective at bringing ulcerative colitis into remission after 52 weeks of treatment, according to one 2021 review.
Has anyone cured their ulcerative colitis?
Currently, there is no known cure for ulcerative colitis, and a person may have the condition throughout their life. Flare-ups can come and go, and people can go for periods of time without experiencing any symptoms of the condition.
What is the main cause of ulcerative colitis?
Many experts believe ulcerative colitis is an autoimmune condition (when the immune system mistakenly attacks healthy tissue). The immune system normally fights off infections by releasing white blood cells into the blood to destroy the cause of the infection.
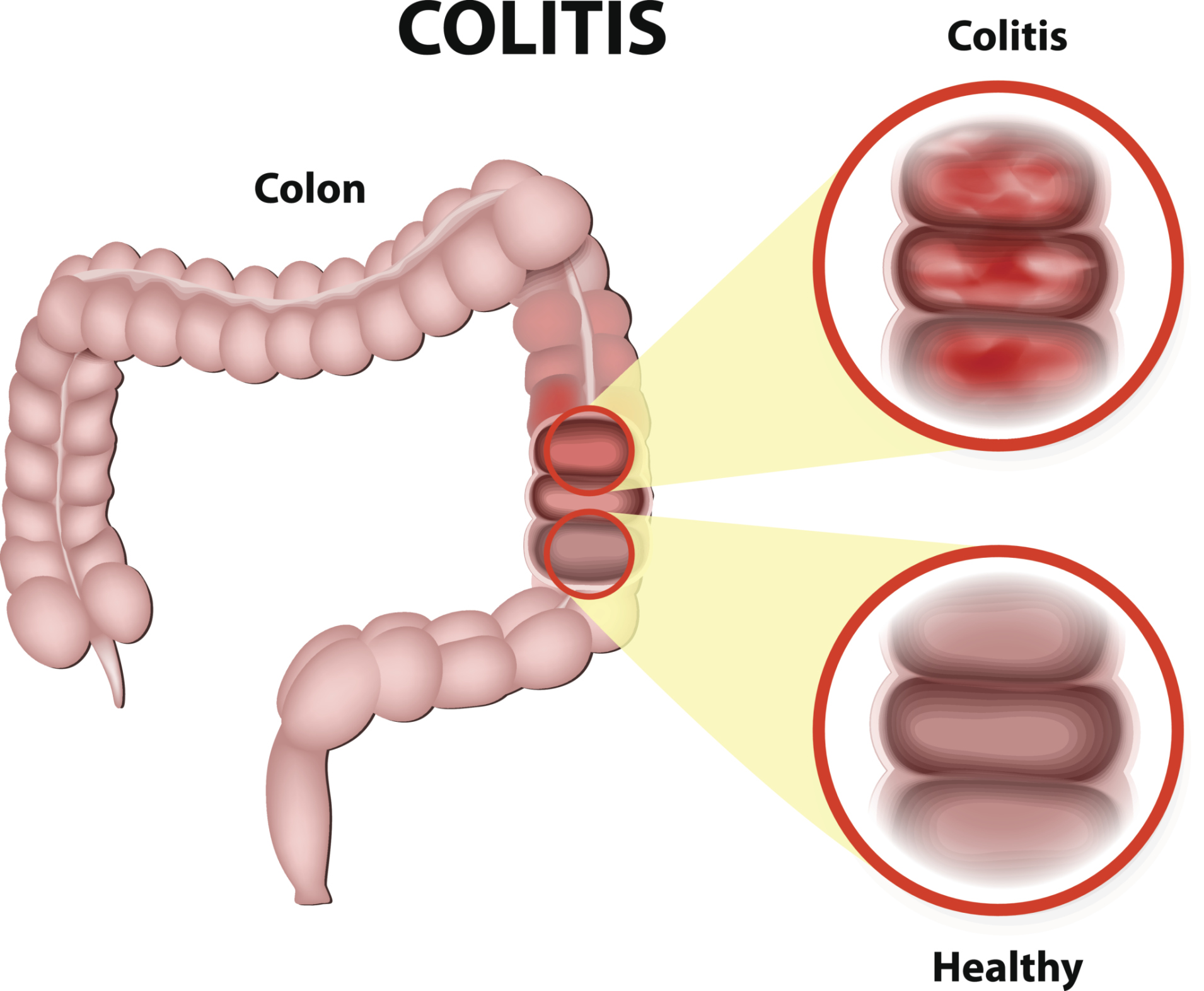
What organs does ulcerative colitis affect?
Ulcerative colitis (UL-sur-uh-tiv koe-LIE-tis) is an inflammatory bowel disease (IBD) that causes inflammation and ulcers (sores) in your digestive tract. Ulcerative colitis affects the innermost lining of your large intestine (colon) and rectum.
Which hospital is best for ulcerative colitis?
Mayo Clinic in Rochester, Minn., ranks No. 1 for digestive disorders in the U.S. News & World Report Best Hospitals rankings.
Can mesalamine be used long term?
Mesalazine can be taken long term. However your doctor will want to check how your kidneys are working during treatment. In rare cases mesalazine can cause kidney problems. These checks usually happen once every 3 months for the first year.
Is there an alternative to mesalamine?
HMPL-004, an extract of Andrographis paniculata, has an efficacy similar to mesalazine for the treatment of ulcerative colitis with a good safety profile, reports a new study from China.
New Therapeutics for Ulcerative Colitis - PubMed
Ulcerative colitis (UC) is a relapsing and remitting inflammatory disease of the colon with a variable course. Despite advances in treatment, only approximately 40% of patients achieve clinical remission at the end of a year, prompting the exploration of new treatment modalities. This review explore …
Ozanimod as effective in treating ulcerative colitis, study shows
Ozanimod, a novel drug molecule, is moderately effective in the treatment of ulcerative colitis, researchers have demonstrated. Ulcerative colits is a debilitating autoimmune disease that causes ...
List of 36 Ulcerative Colitis, Active Medications Compared - Drugs.com
Compare risks and benefits of common medications used for Ulcerative Colitis, Active. Find the most popular drugs, view ratings and user reviews.
List of 63 Ulcerative Colitis Medications Compared - Drugs.com
Drugs.com provides accurate and independent information on more than 24,000 prescription drugs, over-the-counter medicines and natural products. This material is provided for educational purposes only and is not intended for medical advice, diagnosis or treatment. Data sources include IBM Watson Micromedex (updated 17 June 2022), Cerner Multum™ (updated 3 June 2022), ASHP (updated 16 May ...
What is the best treatment for ulcerative colitis?
Anti-inflammatory drugs. Anti-inflammatory drugs are often the first step in the treatment of ulcerative colitis and are appropriate for the majority of people with this condition. These drugs include: 5-aminosalicylates.
What is the only way to diagnose ulcerative colitis?
Endoscopic procedures with tissue biopsy are the only way to definitively diagnose ulcerative colitis. Other types of tests can help rule out complications or other forms of inflammatory bowel disease, such as Crohn's disease.
What is the name of the drug that neutralizes the immune system?
Infliximab (Remicade), adalimumab (Humira) and golimumab (Simponi). These drugs, called tumor necrosis factor (TNF) inhibitors, or biologics, work by neutralizing a protein produced by your immune system. They are for people with severe ulcerative colitis who don't respond to or can't tolerate other treatments.
What does it mean when you have a white blood cell in your stool?
Stool studies. White blood cells or certain proteins in your stool can indicate ulcerative colitis.
What is the procedure to remove a colon and rectum?
In most cases, this involves a procedure called ileoanal anastomosis (J-pouch) surgery. This procedure eliminates the need to wear a bag to collect stool.
How often do you need a colonoscopy?
If your disease involves more than your rectum, you will require a surveillance colonoscopy every one to two years, beginning as soon as eight years after diagnosis if the majority of your colon is involved, or 15 years if only the left side of your colon is involved.
What is the test for sigmoid colon?
A tissue sample is necessary to make the diagnosis. Flexible sigmoidoscopy . Your doctor uses a slender, flexible, lighted tube to examine the rectum and sigmoid colon — the lower end of your colon. If your colon is severely inflamed, your doctor may perform this test instead of a full colonoscopy.
Can a colonectomy be done for ulcerative colitis?
In all patients, elective colectomy can be a cure for ulcerative colitis. Almost always, the procedure is a total colectomy, meaning the entire colon is removed. Surgical procedures include:
Is ileostomy permanent?
An ileostomy can be temporary or permanent. Restorative proctocolectomy with ileal pouch-anal anastomosis. Removal of the entire colon and most of or the entire rectum. A new rectum is created from the small bowel.This procedure can be performed laparoscopically to ease recovery and reduce scarring.
What is the best medicine for ulcerative colitis?
Ulcerative colitis medicines that reduce inflammation in the large intestine include. aminosalicylates, which doctors prescribe to treat mild or moderate ulcerative colitis or to help people stay in remission. , also called steroids, which doctors prescribe to treat moderate to severe ulcerative colitis and to treat mild to moderate ulcerative ...
How do doctors treat ulcerative colitis?
Doctors treat ulcerative colitis with medicines and surgery. Each person experiences ulcerative colitis differently, and doctors recommend treatments based on how severe ulcerative colitis is and how much of the large intestine is affected. Doctors most often treat severe and fulminant ulcerative colitis in a hospital.
What are the most common treatments for severe complications?
Doctors most often treat severe complications in a hospital. Doctors may give. antibiotics. NIH external link. , if severe ulcerative colitis or complications lead to infection. blood transfusions. NIH external link. to treat severe anemia. IV fluids and electrolytes to prevent and treat dehydration.
What type of surgery is used for ulcerative colitis?
The most common types of surgery for ulcerative colitis are. ileoanal reservoir surgery. Surgeons create an internal reservoir, or pouch, from the end part of the small intestine, called the ileum. Surgeons attach the pouch to the anus. Ileoanal reservoir surgery most often requires two or three operations.
How many operations are required for ileoanal reservoir surgery?
Ileoanal reservoir surgery most often requires two or three operations. After the operations, stool will collect in the internal pouch and pass through the anus during bowel movements. ileostomy. Surgeons attach the end of your ileum to an opening in your abdomen called a stoma.
What supplements are recommended for osteoporosis?
To prevent or slow loss of bone mass and osteoporosis. NIH external link. , doctors may recommend calcium and vitamin D supplements or medicines, if needed. For safety reasons, talk with your doctor before using dietary supplements.
Can corticosteroids be used for long term?
Doctors typically don’t prescribe corticosteroids for long-term use or to maintain remission. Long-term use may cause serious side effects. immunosuppressants, which doctors may prescribe to treat people with moderate to severe ulcerative colitis and help them stay in remission. Doctors may also prescribe immunosuppressants to treat severe ...
How much Zeposia is needed for ulcerative colitis?
Zeposia is an oral medication taken once a day. The dose is 0.92 milligrams. Dr. Rudolph Bedford, a gastroenterologist at Providence Saint John’s Health Center in Santa Monica, told Healthline that Zeposia is a potential game changer for people with ulcerative colitis who don’t respond to traditional therapies.
How long does it take for Zeposia to go into remission?
The participants were receiving treatment with oral aminosalicylates or corticosteroids before and during the induction period. At 10 weeks, 18 percent of people taking Zeposia reached clinical remission. That compares to 6 percent in the placebo group.
Can ulcerative colitis be removed?
Currently, the only potential cure for ulcerative colitis is surgery to remove the colon. But there are several types of medications to help manage the disease. adults in the United States have been diagnosed with ulcerative colitis or Crohn’s disease, another type of IBD. The FDA approved Zeposia in 2020 as a disease-modifying therapy ...
What is the best treatment for ulcerative colitis?
Anti-inflammatory drugs: Anti-inflammatory drugs, such as 5-aminosalicylates ( Sulfasalazine, Balsalazides, etc.) and corticosteroids ( Prednisolone, Budesonide, etc.), suppress the cells causing inflammation. These drugs are usually the first step in the treatment of ulcerative colitis (UC) and are well tolerated by most patients.
What causes ulcerative colitis?
The exact cause of ulcerative colitis (UC) is unknown; the possible causes are as follows: Genetics: This may play a role in the development of this condition. Immune reactions: The body’s own antibodies attack the inner lining of the large intestine (an autoimmune disorder). Environmental factors:
What are the symptoms of a swollen colon?
Symptoms of the inflammation of the colon lining include diarrhea, pain, and blood in the stool. There are several causes of colitis, including infection, ischemia of the colon, inflammatory bowel disease (Crohn's disease, ulcerative colitis, infectious colitis like C. difficile, or microscopic colitis). Treatment depends on the cause of the ...
How to prevent flare ups?
Management of psychological stress and emotional support is important to prevent and reduce flare-ups. Regular exercises and a healthy diet are important as well. A low-fat diet with vitamin B6, sulfur, and milk is advised.
Is colitis a lifelong illness?
It is also associated with various manifestations outside of the colon, such as inflammation of the eyes, joints, skin, and lungs. Ulcerative colitis is a lifelong illness with no specific cause or cure. Patients have repeated cycles of flare-ups and disappearance of the disease.
Is colitis contagious?
Colitis has many different causes. Some types of colitis are contagious and some are not contagious. Symptoms and signs of colitis include diarrhea, abdominal discomfort, cramping, pain, and blood in the stools. Treatment for colitis depends on the cause and type of colitis.
Is ulcerative colitis a chronic disease?
Symptoms include abdominal pain, diarrhea, and rectal bleeding. Ulcerative colitis is closely related to Crohn's disease, and together they are referred to as inflammatory bowel disease . Treatment depends upon the type of ulcerative colitis diagnosed.
What is the best treatment for IBD?
Medical therapies for IBD have traditionally focused on symptom control. While the use of oral aminosalicylates and corticosteroids can be effective in suppressing the inflammatory process and inducing symptomatic remission, this approach has not been shown to alter the natural history of IBD, reduce incidence of long-term complications ...
What is the disease that causes progressive functional and structural damage to the gastrointestinal tract?
Advances in the treatment of Crohn's disease and ulcerative colitis. Inflammatory bowel disease (IBD) is a chronic inflammatory disease that can cause progressive functional and structural damage to the gastrointestinal tract. IBD is a global disease with increasing prevalence. In this article, Mayo gastroenterologists provide an overview ...
When was tofacitinib approved?
Approved in 2018, tofacitinib is a selective Janus kinase (JAK) inhibitor and the first oral medication approved for treatment of moderate to severe ulcerative colitis. The Food and Drug Administration examined results from three controlled clinical trials to assess tofacitinib's efficacy and safety. In two placebo-controlled induction trials — ...
Is IBD a global disease?
IBD is a global disease with increasing prevalence. In this article, Mayo gastroenterologists provide an overview of new treatment approaches for Crohn's disease and ulcerative colitis.
Is Ustekinumab approved for Crohn's disease?
And ustekinumab, a biologic that targets cytokines interleukin-12 and interleukin-23 (IL-12 and IL-23 ), has been approved for Crohn's disease treatment. According to Michael F. Picco, M.D., Ph.D., the approach to maximizing the effectiveness of these medications often includes therapeutic drug monitoring. Dr.
Is etrolizumab effective in ulcerative colitis?
Etrolizumab, an anti-β7 integrin, was effective in moderate to severe ulcerative colitis in a phase II trial and so far in an open-label induction trial in phase III. It also looks promising in induction of moderate to severe Crohn's disease. The anti-mucosal addressin cell adhesion molecule (MAdCAM) monoclonal antibody (renamed SHP647) ...
What is the goal of ulcerative colitis?
When you have ulcerative colitis (UC), the goal of treatment is to stop your immune system from attacking the lining of your intestine. This will bring down the inflammation causing your symptoms and put you into remission.
What is the best medicine for UC?
Aminosalicylates (5-ASA drugs) This group of drugs contains the ingredient 5-aminosalicylic acid (5-ASA). They include: When you take these drugs by mouth or as an enema, they help bring down inflammation in your intestine. Aminosalicylates work best for mild-to-moderate UC, and they can help prevent flare-ups.
When was Infliximab approved?
infliximab-abda (Renflexis), FDA approved in May 2017. infliximab-axxq (Avsola), FDA approved in December 2019. infliximab-dyyb (Inflectra), FDA approved in April 2016. The Remicade biosimilars are the only ones currently available for purchase in the United States.
What is a fecal transplant?
A fecal transplant, or stool transplant, is an experimental technique that places healthy bacteria from a donor’s stool into the colon of someone with UC. The idea may sound unappealing, but the good bacteria help heal damage from UC and restore a healthy balance of germs in the gut.
Why is a colon removed after a colonectomy?
Proctocolectomy is the most common type. In this procedure, the entire rectum and colon are removed in order to prevent further inflammation. After surgery, you won’t have a colon to store wastes. Your surgeon will create a pouch inside of your body from part of your small intestine (ileum).
Does methotrexate help with UC?
According to a 2018 study, methotrexate may not be effective at helping people with UC remain in remission. People who take methotrexate also have an increased risk of stomach and intestinal problems. Immunomodulators haven’t been approved by the Food and Drug Administration (FDA) for the treatment of UC.

Diagnosis
Treatment
- Ulcerative colitis treatment usually involves either drug therapy or surgery. Several categories of drugs may be effective in treating ulcerative colitis. The type you take will depend on the severity of your condition. The drugs that work well for some people may not work for others, so it may take time to find a medication that helps you. In addi...
Clinical Trials
- Explore Mayo Clinic studiestesting new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Lifestyle and Home Remedies
- Sometimes you may feel helpless when facing ulcerative colitis. But changes in your diet and lifestyle may help control your symptoms and lengthen the time between flare-ups. There's no firm evidence that what you eat actually causes inflammatory bowel disease. But certain foods and beverages can aggravate your signs and symptoms, especially during a flare-up. It can be helpfu…
Alternative Medicine
- Many people with digestive disorders have used some form of complementary and alternative medicine (CAM). However, there are few well-designed studies showing the safety and effectiveness of complementary and alternative medicine. Although research is limited, there is some evidence that adding probiotics along with other medications may be helpful, but this has …
Preparing For Your Appointment
- Symptoms of ulcerative colitis may first prompt you to visit your primary care doctor. Your doctor may recommend you see a specialist who treats digestive diseases (gastroenterologist). Because appointments can be brief, and there's often a lot of information to discuss, it's a good idea to be well prepared. Here's some information to help you get ready, and what to expect from your doct…