Medication
What is the treatment for DKA (diabetes-related ketoacidosis)? If DKA is caught early enough, people with diabetes can sometimes treat DKA from home with specific instructions from their healthcare provider. If you think you might be developing DKA, call …
Therapy
Initial treatment should focus on fluid resuscitation to restore tissue perfusion and correction of acidosis with a gradual controlled correction of serum glucose levels. Fluid resuscitation to restore tissue perfusion ─ Administer normal saline 20ml/kg (up to 1 liter) IV over 1 hour; this may be repeated based upon the severity of dehydration.
Self-care
Jan 19, 2021 · When treating patients with DKA, the following points must be considered and closely monitored: Correction of fluid loss with intravenous fluids Correction of hyperglycemia with insulin Correction of electrolyte disturbances, particularly potassium loss Correction of acid-base balance Treatment of ...
Nutrition
Treatment of DKA If you get diagnosed with DKA then the treatment options available are fluid replacement, electrolyte replacement, and insulin therapy. The goals of the treatment of DKA are to optimize volume status, hyperglycemia, and ketoacidosis, electrolyte abnormalities, and potential precipitating factors.
What type of insulin is given for DKA?
Severe DKA is defined by a pH <7.15 and usually will require treatment in the ICU. Moderate DKA is defined by a pH of 7.15-7.25 and can usually be treated on the ward. A pH >7.25 is mild DKA and usuallycan be treated in the ED over a 4-6 hour time period, or on the floor, if admission is otherwise required. II. Causes of DKA:
Which is insulin used for DKA?
Aug 01, 1999 · The initial priority in the treatment of diabetic ketoacidosis is the restoration of extra-cellular fluid volume through the intravenous administration of a normal saline (0.9 percent sodium...
How to treat ketoacidosis naturally?
Apr 02, 2022 · Initial workup should include aggressive volume, glucose, and electrolyte management. Read More Related Questions: What may cause false findings in lab tests for diabetic ketoacidosis (DKA)? What...
How is DKA treated?
Explore
What is the first step in treating DKA?
The initial priority in the treatment of diabetic ketoacidosis is the restoration of extra-cellular fluid volume through the intravenous administration of a normal saline (0.9 percent sodium chloride) solution.1 Aug 1999
What is the protocol for DKA?
A mix of 24 units of regular insulin in 60 mL of isotonic sodium chloride solution usually is infused at a rate of 15 mL/h (6 U/h) until the blood glucose level drops to less than 180 mg/dL; the rate of infusion then decreases to 5-7.5 mL/h (2-3 U/h) until the ketoacidotic state abates.19 Jan 2021
How is primary care treated in DKA?
The recommended mode of treatment of DKA is bolus intravenous (IV) or intramuscular (IM) short-acting insulin followed by continuous IV infusion. The IV therapy has the advantage of rapid onset of action and maintenance of a steady level of insulin in the blood.
What are the three key actions for the management of DKA?
Key DKA management pointsStart intravenous fluids before insulin therapy.Potassium level should be >3.3 mEq/L before the initiation of insulin therapy (supplement potassium intravenously if needed).Administer priming insulin bolus at 0.1 U/kg and initiate continuous insulin infusion at 0.1 U/kg/h.More items...•30 Jun 2014
How do hospitals manage DKA?
If you're diagnosed with diabetic ketoacidosis, you might be treated in the emergency room or admitted to the hospital....Treatment usually involves:Fluid replacement. You'll receive fluids — either by mouth or through a vein — until you're rehydrated. ... Electrolyte replacement. ... Insulin therapy.11 Nov 2020
How do pediatrics manage DKA?
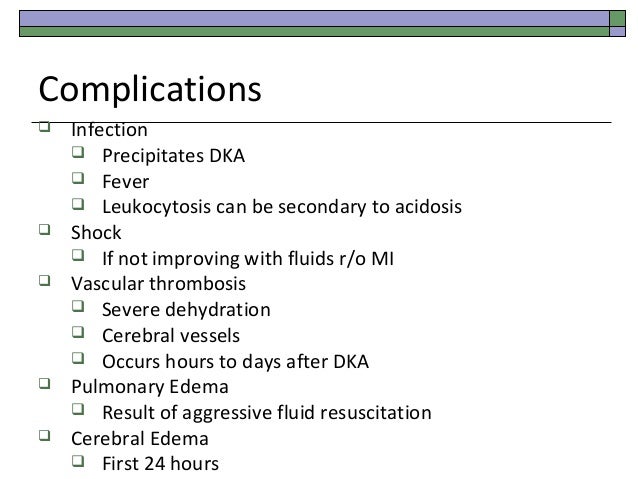
Treatment involves administration of intravenous fluids and insulin. Children with diabetic ketoacidosis require serial laboratory studies for electrolyte derangements and close clinical monitoring for signs of cerebral edema, an uncommon but potentially fatal complication of pediatric diabetic ketoacidosis.7 May 2021
What type of insulin is given for DKA?
The mainstay in the treatment of DKA involves the continuous intravenous (IV) infusion of regular insulin or the frequent subcutaneous (SC) injections of regular or rapid-acting insulin analogs.
What are the three criteria for DKA?
DIFFERENTIAL DIAGNOSIS Three key features of diabetic acidosis are hyperglycemia, ketosis, and acidosis. The conditions that cause these metabolic abnormalities overlap.1 May 2005
Why is potassium given in DKA?
After insulin treatment is initiated, potassium shifts intracellularly and serum levels decline. Replacement of potassium in intravenous fluids is the standard of care in treatment of DKA to prevent the potential consequences of hypokalemia including cardiac arrhythmias and respiratory failure.27 Nov 2014
What are the therapeutic goals of DKA?
The therapeutic goals of DKA management include optimization of 1) volume status; 2) hyperglycemia and ketoacidosis; 3) electrolyte abnormalities; and 4) potential precipitating factors. The majority of patients with DKA present to the emergency room. Therefore, emergency physicians should initiate the management of hyperglycemic crisis while a physical examination is performed, basic metabolic parameters are obtained, and final diagnosis is made. Several important steps should be followed in the early stages of DKA management: 1 collect blood for metabolic profile before initiation of intravenous fluids; 2 infuse 1 L of 0.9% sodium chloride over 1 hour after drawing initial blood samples; 3 ensure potassium level of >3.3 mEq/L before initiation of insulin therapy (supplement potassium intravenously if needed); 4 initiate insulin therapy only when steps 1–3 are executed.
Is ketoacidosis a type 1 or 2 diabetes?
Diabetic ketoacidosis (DKA) is a rare yet potentially fatal hyperglycemic crisis that can occur in patients with both type 1 and 2 diabetes mellitus. Due to its increasing incidence and economic impact related to the treatment and associated morbidity, effective management and prevention is key. Elements of management include making ...
Can DKA cause hypokalemia?
A “normal” plasma potassium concentration still indicates that total body potassium stores are severely diminished, and the institution of insulin therapy and correction of hyperglycemia will result in hypokalemia.
What is a DKA?
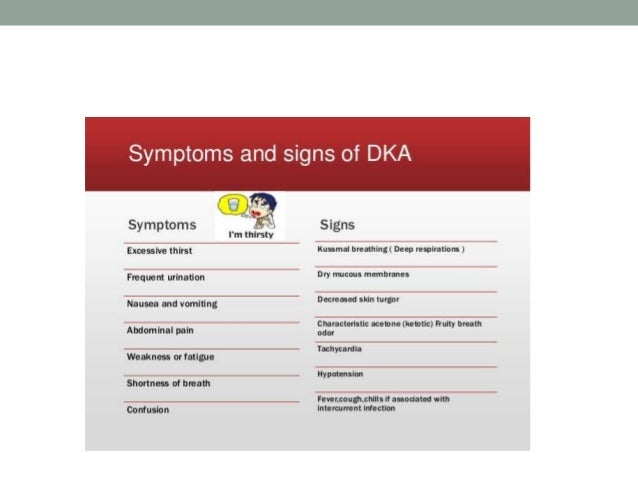
Diabetic ketoacidosis (DKA) is a serious complication of diabetes that can be life-threatening. DKA is most common among people with type 1 diabetes. People with type 2 diabetes can also develop DKA. DKA develops when your body doesn’t have enough insulin to allow blood sugar into your cells for use as energy.
What happens when you have too many ketones?
When too many ketones are produced too fast, they can build up to dangerous levels in your body. Read on to learn more about DKA, how you can prevent DKA, and how to treat it if needed.
How to prevent DKA?
Prevent DKA. DKA is a serious condition, but you can take steps to help prevent it: Check your blood sugar often, especially if you’re sick. Keep your blood sugar levels in your target range as much as possible. Take medicines as prescribed, even if you feel fine.
What causes DKA in diabetics?
Missing insulin shots, a clogged insulin pump, or the wrong insulin dose. Other causes of DKA include: Heart attack or stroke. Physical injury, such as from a car accident. Alcohol or drug use. Certain medicines, such as some diuretics (water pills) and corticosteroids (used to treat inflammation in the body).
What to do if your ketones are high?
Call your doctor if your ketones are moderate or high. Elevated ketones are a sign of DKA, which is a medical emergency and needs to be treated immediately. Go to the emergency room or call 911 right away if you can’t get in touch with your doctor and are experiencing any of the following:
How long to treat diabetic ketoacidosis?
Managing diabetic ketoacidosis (DKA) in an intensive care unit during the first 24-48 hours always is advisable. When treating patients with DKA, the following points must be considered and closely monitored: Correction of electrolyte disturbances, particularly potassium loss. It is essential to maintain extreme vigilance for any concomitant ...
When to use sodium bicarbonate?
If sodium bicarbonate is indicated, 100-150 mL of 1.4% concentration is infused initially. This may be repeated every half hour if necessary.
Can insulin be used for DKA?
When insulin treatment is started in patients with DKA, several points must be considered. A low-dose insulin regimen has the advantage of not inducing the severe hypoglycemia or hypokalemia that may be observed with a high-dose insulin regimen. Only short-acting insulin is used for correction of hyperglycemia.
Is insulin used for hyperglycemia?
Only short-acting insulin is used for correction of hyperglycemia. Subcutaneous absorption of insulin is reduced in DKA because of dehydration; therefore, using intravenous routes is preferable. SC use of the fast-acting insulin analog (lispro) has been tried in pediatric DKA (0.15 U/kg q2h).
What are the therapeutic goals of diabetic ketoacidosis?
The therapeutic goals for diabetic ketoacidosis consist of improving circulatory volume and tissue perfusion, reducing blood glucose and serum osmolality toward normal levels, clearing ketones from serum and urine at a steady rate, correcting electrolyte imbalances and identifying precipitating factors. A suggested flow sheet for monitoring therapeutic response is provided in Figure 3. 6
How long does subcutaneous insulin last?
When diabetic ketoacidosis has been controlled, subcutaneous insulin therapy can be started. The half-life of regular insulin is less than 10 minutes. Therefore, to avoid relapse of diabetic ketoacidosis, the first subcutaneous dose of regular insulin should be given at least one hour before intravenous insulin is discontinued. 1, 22 A protocol for the administration of subcutaneous insulin is included in Figure 2.
Is ketoacidosis a life threatening condition?
Diabetic ketoacidosis is an emergency medical condition that can be life-threatening if not treated properly. The incidence of this condition may be increasing, and a 1 to 2 percent mortality rate has stubbornly persisted since the 1970s. Diabetic ketoacidosis occurs most often in patients with type 1 diabetes ...
Is a physical exam necessary for a diabetic?
The history and physical examination continue to be important aspects of management. Even in comatose patients, information documenting a history of diabetes or insulin therapy may be available. The physical examination can provide supportive evidence for the diagnosis of diabetic ketoacidosis and can point to precipitating factors ( Table 2). 3, 4
Can you take bicarbonate with insulin?
In general, supplemental bicarbonate therapy is no longer recommended for patients with diabetic ketoacidosis, because the plasma bicarbonate concentration increases with insulin therapy. 1, 4, 8, 16, 17 Insulin administration inhibits ongoing lipolysis and ketone production and also promotes the regeneration of bicarbonate.
Is there a randomized prospective study for diabetic ketoacidosis?
No randomized prospective studies have evaluated the optimal site of care for patients with diabetic ketoacidosis. The response to initial therapy in the emergency department can be used as a guideline for choosing the most appropriate hospital site (i.e., intensive care unit, step-down unit, general medical ward) for further care.
What should be included in a sick day management program?
An educational program should include sick-day management instructions (i.e., for any illness that alters routine care), including the use of short-acting insulin, blood glucose and urinary ketone monitoring, and the use of a liquid diet containing carbohydrates and salt. Patients should not discontinue insulin therapy when they are ill, and they should contact their physician early in the course of illness. Indications for hospitalization include greater than 5 percent loss of body weight, respiration rate of greater than 35 per minute, intractable elevation of blood glucose concentrations, change in mental status, uncontrolled fever and unresolved nausea and vomiting.
