Medication
Feb 15, 2017 · a nonenteric coated aspirin (162 to 325 mg) at first rec- ognition of ACS symptoms, unless they have a history of severe aspirin sensitivity. 4 At the community level,
Procedures
Nov 29, 2016 · Current guidelines for the treatment of ACS recommend that all patients routinely receive a loading dose of aspirin, followed by maintenance therapy unless contraindicated.[3,4] There is a wide range of maintenance dosages of aspirin that are prescribed in this context, ranging from 75 to 325 mg daily in different countries.
Self-care
Mar 06, 2014 · Desired Outcome All patients exhibiting signs of Acute Coronary Syndrome receive Aspirin before arrival at the hospital. Standard 100% of patients with no contraindications. ... Berger JS, et al, “Initial Aspirin Dose and Outcome Among ST-Elevation Myocardial Infarction Patients Treated With Fibrinolytic Therapy.” Circulation (2008) 117:192 ...
Nutrition
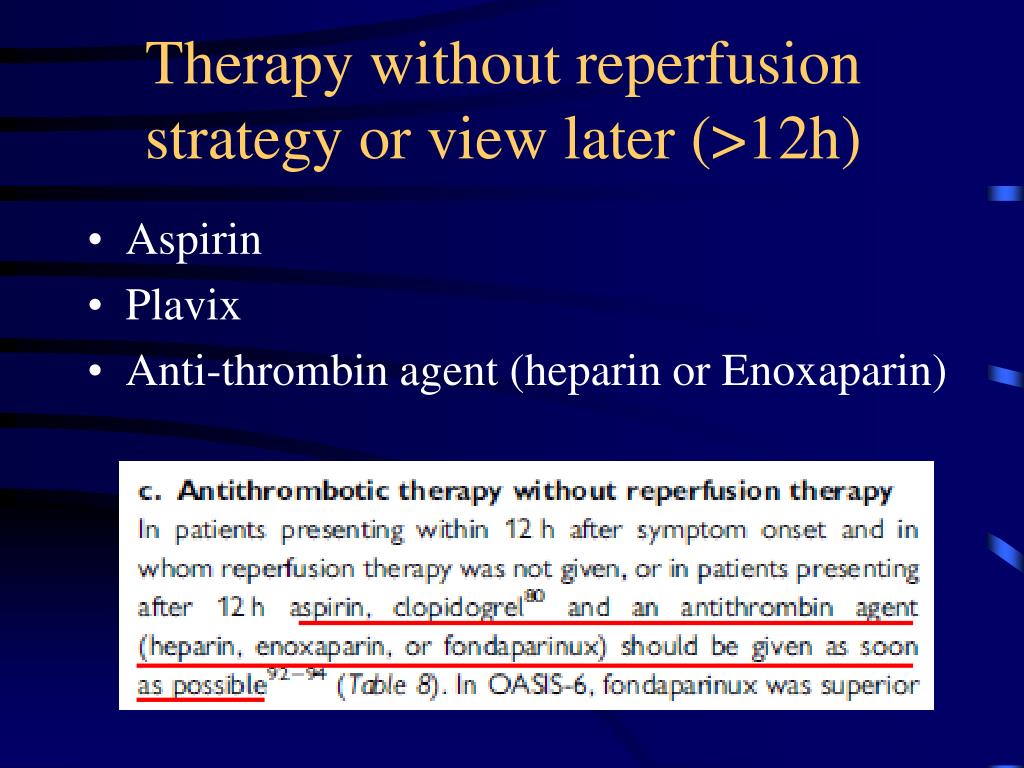
Jul 27, 2017 · Due to its efficacy and safety profile, the ESC recommends the use of subcutaneous fondaparinux at a dose of 2.5 mg once daily in patients presenting with NSTE-ACS regardless of the planned management strategy unless coronary angiography is imminent.[4,48] In patients managed for NSTE-ACS with fondaparinux a bolus of UFH is recommended at the …
What are the ACS Guidelines for aspirin?
Aug 02, 2021 · Version 2021.01.c. In the presence of ACS, EMS or the Emergency Department will start with care and focus on obtaining a 12-lead ECG, aspirin administration, oxygen therapy if oxygen saturation is <90% or if the patient is short of breath, administering nitroglycerin if not contraindicated and/or morphine for discomfort if no relief with nitroglycerin, and most …
How many patients are given 162 mg of aspirin?
Dec 17, 2007 · A wide range of aspirin doses have been evaluated to determine the best way to achieve maximal antiplatelet activity in the acute setting. 24–26 In a study that evaluated the acute effect of 40-, 100-, 300-, and 500-mg doses of aspirin, the 100-, 300-, and 500-mg doses were found to inhibit platelet aggregation at 2 hours, with no difference observed between the …
Are there recommended aspirin doses for patients with coronary artery disease?
Mar 29, 2016 · LD: 81-325 mg if already taking aspirin or 325 mg non-enteric aspirin if not taking aspirin; MD: 75-100 mg daily with a P2Y12 inhibitor as part of DAPT. 2011 ACCF/AHA PCI. 2016 ACCF/AHA DAPT. CABG. Pre-op dose: 100-325 mg; Post-op …
When should aspirin be added to anticoagulation in patients with A4 syndrome?
17 1.1.5 Offer people with acute STEMI a single loading dose of 300 mg aspirin as 18 soon as possible unless there is clear evidence that they are allergic to it. 19 [2010] DRAFT FOR CONSULTATION Acute coronary syndromes (update): NICE guideline DRAFT (February 2020) 5 …

What are the primary prevention factors for ACS?
The ACC/AHA guidelines continue to emphasize the importance of primary prevention of ACS by decreasing coronary artery disease risk factors, including hypertension, hypercholesterolemia, diabetes mellitus, and smoking. 1 Family history of coronary artery disease is also a risk factor.
Who should be educated about ACS?
Family physicians should continue to educate patients about the risk factors, clinical presentation, and symptoms of ACS. Older persons, persons with diabetes, women, and postoperative patients should be aware that they may have atypical symptoms and presentation for ACS.
How many patients received 162 mg of aspirin?
Information on immediate aspirin dose and short-term outcomes was available for 48 422 patients (86%). An immediate aspirin dose of 162 mg was given to 36 594 patients (75.6%). Patients from GUSTO I were more likely to receive 162 mg, whereas patients from GUSTO III were more likely to receive 325 mg. Baseline characteristics according to aspirin dose are presented in Table 1. It is evident that there were some imbalances between the groups. Patients receiving 162 mg were more frequently enrolled from North America, more likely to be current smokers and diabetic, less likely to have a family history of cardiac disease or history of MI, and more likely to have an inferior MI than those receiving 325 mg. Treatment and procedural characteristics are depicted in Table 2. Patients who received 162 mg were more likely to receive streptokinase; were less likely to receive tenectaplase and reteplase; had significantly higher measured activated partial thromboplastin times at 6, 12, and 24 hours; and were more likely to undergo invasive procedures. In-hospital medications also were significantly different between the groups ( Table 2 ).
Is 325 mg aspirin safe?
Although these data are nonrandomized, they suggest that for the first dose of aspirin, 162 mg may be as effective as and safer than 325 mg for the acute treatment of STEMI.
Is aspirin randomized?
There are several limitations to our study. First, our study was a post hoc analysis of prospectively collected data within the context of 2 clinical trials. As such , the dose of aspirin was not prescribed by the study protocol, nor was it randomized. In general, treatment effects cannot be reliably estimated by observational studies, even when good adjustment models are available. However, the data with respect to both efficacy and safety are mechanistically consistent. Second, we could not explore the indications for a specific aspirin dose. Nevertheless, the main determinant of the dose used in patients in GUSTO I and GUSTO III was the routine approach of centers and specific countries ( Table 1 ). This argues against the possibility that the selection of dose may be related to the risk profile of patients, thus confounding the differences in efficacy or safety between dose groups. Third, trial differences and regional differences in patient populations and practice patterns are reflected by significant differences in the baseline characteristics of the patients ( Table 1) and in additional treatments. However, after adjustment for these differences, including the use of fibrinolytics and other antithrombotics, and stratification by clinical trial and region, a dose response between aspirin and bleeding complications is still observed. Fourth, it was unknown whether the patient was on aspirin before the infarction. Finally, GUSTO I and III were performed 10 to 15 years ago, before clopidogrel and glycoprotein IIb/IIIa use, which may limit the generalizability of the results. Nevertheless, with the current use of dual and triple antiplatelet therapy in STEMI, great focus remains on minimizing bleeding risk.
Does aspirin cause bleeding?
The major risk of aspirin therapy is the risk of bleeding, and there is considerable evidence that the side effects of aspirin are dose dependent. 3,8,38,39 A UK study group found that patients with higher aspirin dose were more likely to have both gastrointestinal tract symptoms and gastrointestinal hemorrhage. 28 In the Dutch TIA trial, 27 risk of bleeding was higher in patients receiving 283 mg compared with those receiving 30 mg. Observational data from the Clopidogrel in Unstable Angina to Prevent Recurrent Events (CURE) investigators 40 noted increased bleeding risks with increasing aspirin dose (<100 mg, 1.9%; 101 to 199 mg, 2.8%; >200 mg, 3.7%; P =0.0001). In a recent analysis of 31 randomized controlled trials, major, minor, gastrointestinal, and fatal bleeding all increased with increased aspirin dose. 41
Does aspirin inhibit platelet cyclooxygenase 1?
Aspirin irreversibly inhibits platelet cyclooxygenase-1, thereby preventing the conversion of arach idonic acid to pro staglandin H 2, which, under normal circumstances, is then converted to thromboxane (TX) A 2 and other bioactive prostanoids. 21 TXA 2 is synthesized and released by platelets and acts as a platelet aggregator and vasoconstrictor. 22 By preventing TXA 2 formation, aspirin irreversibly blocks platelet function. At higher doses, aspirin suppresses vascular endothelial cell production of prostacyclin, 23 which, if unopposed, results in inhibition of platelet aggregation and induces vasodilation.
Expert Analysis
Aspirin is indicated for prevention and/or treatment of a wide variety of cardiovascular conditions, including primary and secondary prevention, percutaneous coronary intervention (PCI), coronary artery bypass graft (CABG) surgery, peripheral arterial disease (PAD), extra-cranial arterial disease, mechanical heart valve replacement and pericarditis.
Recommended Aspirin Doses in Patients with Coronary Artery Disease
Aspirin is indicated for prevention and/or treatment of a wide variety of cardiovascular conditions, including primary and secondary prevention, percutaneous coronary intervention (PCI), coronary artery bypass graft (CABG) surgery, peripheral arterial disease (PAD), extra-cranial arterial disease, mechanical heart valve replacement and pericarditis.