
What is the life expectancy of someone with gastroparesis?
Management of gastroparesis should include assessment and correction of nutritional state, relief of symptoms, improvement of gastric emptying and, in diabetics, glycemic control. Patient nutritional state should be managed by oral dietary modifications.
How to manage diabetic gastroparesis?
Prior to any intervention, the underlying mechanism that may exacerbate an already existing gastroparesis should be managed, and clinicians should be aware that certain medications might exacerbate gastric emptying abnormalities, including H 2 receptor antagonists, proton pump inhibitors, antihistamines, opioids, tricyclic antidepressants, benzodiazepines, and calcium …
How does gastroparesis affect people with diabetes?
Mar 28, 2018 · Management of gastroparesis should include assessment and correction of nutritional state, relief of symptoms, improvement of gastric emptying and, in diabetics, glycemic control. Patient nutritional state should be managed by oral dietary modifications.
Can you gain weight if you have gastroparesis?
Jun 22, 2018 · The American College of Gastroenterology (ACG) guidelines for the diagnosis and management of DGp state that a combination of appropriate symptoms and signs, along with delayed gastric emptying in the absence of gastric outlet obstruction or ulceration, is required to establish the diagnosis of DGp [ 4 ].
What is the best treatment for diabetic gastroparesis?
Medications to treat gastroparesis may include:Medications to stimulate the stomach muscles. These medications include metoclopramide (Reglan) and erythromycin. ... Medications to control nausea and vomiting. Drugs that help ease nausea and vomiting include diphenhydramine (Benadryl, others) and ondansetron (Zofran).Oct 10, 2020
What are the treatment options for gastroparesis?
Treatment for GastroparesisChanging eating habits. ... Controlling blood glucose levels. ... Medicines. ... Oral or nasal tube feeding. ... Jejunostomy tube feeding. ... Parenteral nutrition. ... Venting gastrostomy. ... Gastric electrical stimulation.
What is the latest treatment for gastroparesis?
Prokinetic agents increase the rate of gastric emptying and decrease symptoms in patients with gastroparesis. Metoclopramide, a dopamine-2 receptor antagonist, is approved by the US Food and Drug Administration (FDA) for the treatment of gastroparesis.
Which medication is approved for gastroparesis and usually used first when a medication is required?
Prokinetics are drugs that increase the strength or frequency of smooth muscle contractions. Metoclopramide is the first-line drug prescribed for gastroparesis and is given as an injection, tablet, or liquid. It has potentially severe side effects, so drugs such as domperidone or tegaserod may be prescribed instead.Nov 17, 2021
What medications make gastroparesis worse?
Medicines that may delay gastric emptying or make symptoms worse include the following: narcotic pain medicines, such as codeine link , hydrocodone link , morphine link , oxycodone link , and tapentadol link. some antidepressants link , such as amitriptyline link , nortriptyline link , and venlafaxine link.
Do antibiotics help gastroparesis?
Gastroparesis can also happen in people who have had surgery on their stomach. Erythromycin is an antibiotic that is licensed to treat various infections of the chest, digestive system, ear, eye, mouth and skin. Erythromycin is usually taken by mouth as tablets, capsules or as a liquid every 6 to 12 hours.Jun 18, 2013
How do you treat gastroparesis naturally?
Steps to take can include:small, frequent meals.avoiding raw or uncooked fruits and vegetables.avoiding fibrous fruits and vegetables.eating liquid foods such as soups or pureed foods.eating foods low in fat.drinking water during meals.gentle exercise following meals, such as walking.More items...•7 days ago
How do you improve gastroparesis?
Although there is no cure for gastroparesis, changes to the diet, along with medication, can offer some relief. Certain medications, such as some antidepressants, opioid pain relievers, and high blood pressure and allergy medications, can lead to slow gastric emptying and cause similar symptoms.Feb 15, 2019
Why do diabetics get gastroparesis?
Extended periods of high glucose in the blood cause nerve damage throughout the body. Chronically high blood sugar levels also damage the blood vessels that supply the body's nerves and organs with nutrition and oxygen. This includes the vagus nerve and digestive tract, both of which ultimately lead to gastroparesis.
Is bethanechol used for gastroparesis?
Prokinetic agents for gastroparesis It enhances amplitude of contractions throughout the GI tract [113]. Bethanechol increases phasic antral motor activity, however the elicited contractions are not peristaltic and do not facilitate gastric emptying [114,115].
What does erythromycin do for gastroparesis?
Erythromycin increases the number of gastric contractions and the force of contractions. Because of these potent gastrokinetic properties, it's used to facilitate gastric emptying in patients with gastroparesis.
Is erythromycin effective for gastroparesis?
These results suggest that for most patients with diabetic gastroparesis, a single 250-mg dose of erythromycin will significantly improve gastric emptying. It is possible that a dose-dependent relationship will be demonstrated with doses of erythromycin less than 250 mg.
What are the symptoms of gastroparesis?
Symptoms from gastroparesis include nausea, vomiting, early satiety, postprandial fullness, bloating, and upper abdominal pain. Management of gastroparesis should include assessment and correction ...
Is enteral nutrition necessary for a jejunostomy tube?
Patient nutritional state should be managed by oral dietary modifications. If oral intake is not adequate, then enteral nutrition via jejunostomy tube needs to be considered. Parenteral nutrition is rarely required when hydration and nutritional state cannot be maintained.
What is the first line of treatment for DGP?
The first-line medical therapy for patients with DGP is generally a combination of an antiemetic agent and a promotility drug (Table 1). Unfortunately, data from adequately powered clinical trials in patients with gastroparesis are limited, and no study has adequately stratified patients by etiologic subtypes.
Why are the 3 scales used in the GCSI?
These 3 scales were selected as part of the GCSI because they assess common symptoms related to gastroparesis—nausea/vomiting, postprandial fullness/early satiety, and bloating. The GCSI is used to rate symptom change by either the physician or the patient over a 2-week recall period.
What is the best phenothiazine for DGP?
The most commonly prescribed phenothiazine agent for DGP is prochlorperazine, a neuroleptic with a potency 10 to 20 times that of chlorpromazine.7Adverse effects include drowsiness, dry mouth, constipation, skin rashes, and tardive dyskinesia.
How often is 13CO2 measured?
Breath 13CO2was measured every 15 minutes for 3 hours, and scintigraphy was performed every 15 to 30 minutes for 5 hours. Researchers found that the breath test detected abnormal gastric emptying with a sensitivity of 86% and specificity of 80%.
What is used to exclude a stricture, mass, or ulcer?
Abdominal radiography, computed tomography, and magnetic resonance imaging can be used to exclude gastric and intestinal obstruction, and an upper endoscopy is needed to exclude a stricture, mass, or ulcer. Laboratory testing can be used to rule out infectious, metabolic, and immunologic causes of upper GI symptoms.
Is gastric emptying a sign of diabetes?
Conclusion. Gastroparesis is characterized by delayed gastric emptying in the absence of mechanical obstruction. Diabetes is a common cause of gastroparesis. Diabetic gastroparesis has been associated with symptoms such as nausea, vomiting, early satiety, bloating, postprandial fullness, abdominal pain, and weight changes.
What is gastroparesis in diabetes?
Gastroparesis is a disorder characterized by a delay in gastric emptying after a meal in the absence of a mechanical gastric outlet obstruction.
What are the symptoms of gastroparesis?
Symptoms from gastroparesis include nausea, vomiting, early satiety, postprandial fullness, bloating, and upper abdominal pain.
How long does it take for a diabetic to have a gastric emptying?
The cardinal symptoms of diabetic gastroparesis are nausea and vomiting. Gastroesophageal scintiscanning at 15-minute intervals for 4 hours after food intake is considered the gold standard for measuring gastric emptying.
How long does metoclopramide last?
Treatment with metoclopramide for longer than 12 weeks should be avoided in all but rare cases where therapeutic benefit is thought to outweigh the risk of developing tardive dyskinesia.
What are the complications of a gastric gastrectomy?
Complications from gastric electrical stimulation (GES) such as local infection or lead migration, as well as complications related to the surgery may occur in up to 10% of patients implanted. The risk of malnutrition and weight loss following gastrectomy has to be weighed relative to the symptom relief.
What causes gastric surgery?
Diabetes is the most common cause. Other causes include some disorders of the nervous system, such as Parkinson's disease and stroke, and some medicines, such as tricyclic antidepressants, calcium channel blockers, and opiate pain relievers. This condition can also be a complication of gastric surgery.
How do you know if you have gastroparesis?
Food coming back up your throat, without nausea or vomiting. Gastroparesis may be suspected in a person with diabetes who has upper digestive tract symptoms or has blood sugar levels that are hard to control.
What is the first line of management for gastroparesis patients?
The first line of management for gastroparesis patients should include restoration of fluids and electrolytes, nutritional support and in diabetics, optimization of glycemic control. (Strong recommendation, moderate level of evidence.) Oral intake is preferable for nutrition and hydration.
What are the symptoms of gastroparesis?
Symptoms from gastroparesis include nausea, vomiting, early satiety, postprandial fullness, bloating, and upper abdominal pain.
What is the best treatment for nausea and vomiting?
Among alternative medicine therapies, acupuncture is the method most studied in treatment of nausea and vomiting; one study reported impressive relief in 94 % of patients (115) (see section on alternative medicine). TCA can be considered for refractory nausea and vomiting in gastroparesis (116,117).
What are the side effects of metoclopramide?
The most common adverse extrapyramidal side effects of metoclopramide are acute dystonias (incidence of 0.2% (81)). The incidence of acute dystonias in a UK series was higher in females, patients receiving higher doses, in children, and young adults. Whereas prolonged reactions were more common in elderly patients.
Can botulinum toxin be used for gastroparesis?
Thus, botulinum toxin injection into the pylorus is not recommended as a treatment for gastroparesis (134), although there is a need for further study in patients with documented “pylorospasm.”. Table 6. Systematic review of studies on botulinum toxin injection into the pylori sphincter for treatment of gastroparesis.
Does GES improve oral tolerance?
Most subsequent reports have been open-label studies, including long-term efficacy reports of several hundred patients, suggesting that GES enhances symptom control and quality of life and improves oral tolerance of feeding (155).
Can gastroparesis cause GERD?
Gastroparesis can be associated with and may aggravate gastroesophageal reflux disease (GERD). Evaluation for the presence of gastroparesis should be considered in patients with GERD that is refractory to acid-suppressive treatment. (Conditional recommendation, moderate level of evidence) Recommendations.
DEFINITION OF GASTROPARESIS SYNDROME AND GASTROPARESIS SYMPTOMS
The diagnosis of gastroparesis is based on the combination of symptoms of gastroparesis, absence of gastric outlet obstruction or ulceration, and delay in gastric emptying. (Strong “We recommend”, High)
IDENTIFYING THE CAUSE OF GASTROPARESIS
Patients with gastroparesis should be screened for the presence of diabetes mellitus, thyroid dysfunction, neurological disease prior gastric or bariatric surgery, and autoimmune disorders. Patients should undergo biochemical screen for diabetes and hypothyroidism; other tests are as indicated clinically. (Strong “We recommend”, High)
DIAGNOSIS OF GASTROPARESIS
Documented delay in gastric emptying is required for the diagnosis of gastroparesis. Scintigraphic gastric emptying of solids is the standard for the evaluation of gastric emptying and the diagnosis of gastroparesis. The most reliable method and parameter for diagnosis of gastroparesis is gastric retention of solids at 4 h measured by scintigraphy.
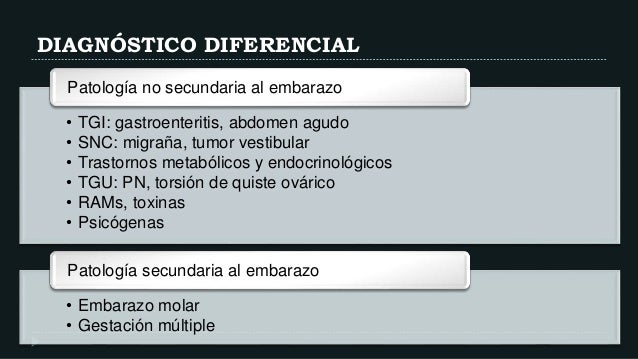
EXCLUSION CRITERIA AND DIFFERENTIAL DIAGNOSIS
The presence of rumination syndrome and/or eating disorders (including anorexia nervosa and bulimia) should be considered when evaluating a patient for gastroparesis. These disorders may be associated with delayed gastric emptying, and identification of these disorders may alter management. (Strong “We recommend”, Moderate)
MANAGEMENT OF GASTROPARESIS
The first line of management for gastroparesis patients should include restoration of fluids and electrolytes, nutritional support and in diabetics, optimization of glycemic control. (Conditional (weak) “We suggest”, Low)
GLYCEMIC CONTROL IN DG
Good glycemic control should be the goal. Since acute hyperglycemia inhibits gastric emptying, it is assumed that improved glycemic control may improve gastric emptying and reduce symptoms. (Conditional (weak) “We suggest”, Moderate)
PHARMACOLOGIC THERAPY
In addition to dietary therapy, prokinetic therapy should be considered to improve gastric emptying and gastroparesis symptoms, taking into account benefits and risks of treatment. (Strong “We recommend”, Moderate)
