
Medication
· Although the guidelines recommend either 14 days of TMP-SMX or 7 days of ciprofloxacin for the treatment of pyelonephritis, a study in 272 women with susceptible E coli pyelonephritis reported...
Nutrition
Outpatient oral antibiotic therapy with a fluoroquinolone is successful in most patients with mild uncomplicated pyelonephritis. Other effective alternatives include extended-spectrum penicillins, amoxicillin-clavulanate potassium, cephalosporins, and trimethoprim-sulfamethoxazole.
What is the best treatment for pyelonephritis?
Table 4, Treatment of Pyelonephritis - Urinary Tract Infection - NCBI Bookshelf. NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health. Bettcher CM, Campbell E, Petty LA, et al. Urinary Tract Infection [Internet]. Ann Arbor (MI): Michigan Medicine University of Michigan; 2021 May.
What are the IDSA guidelines on the treatment of pyelonephritis?
· Outpatient oral antibiotic therapy with a fluoroquinolone is successful in most patients with mild uncomplicated pyelonephritis. Other effective alternatives include extended-spectrum penicillins,...
What is the treatment for xanthogranulomatous pyelonephritis (kidney infection)?
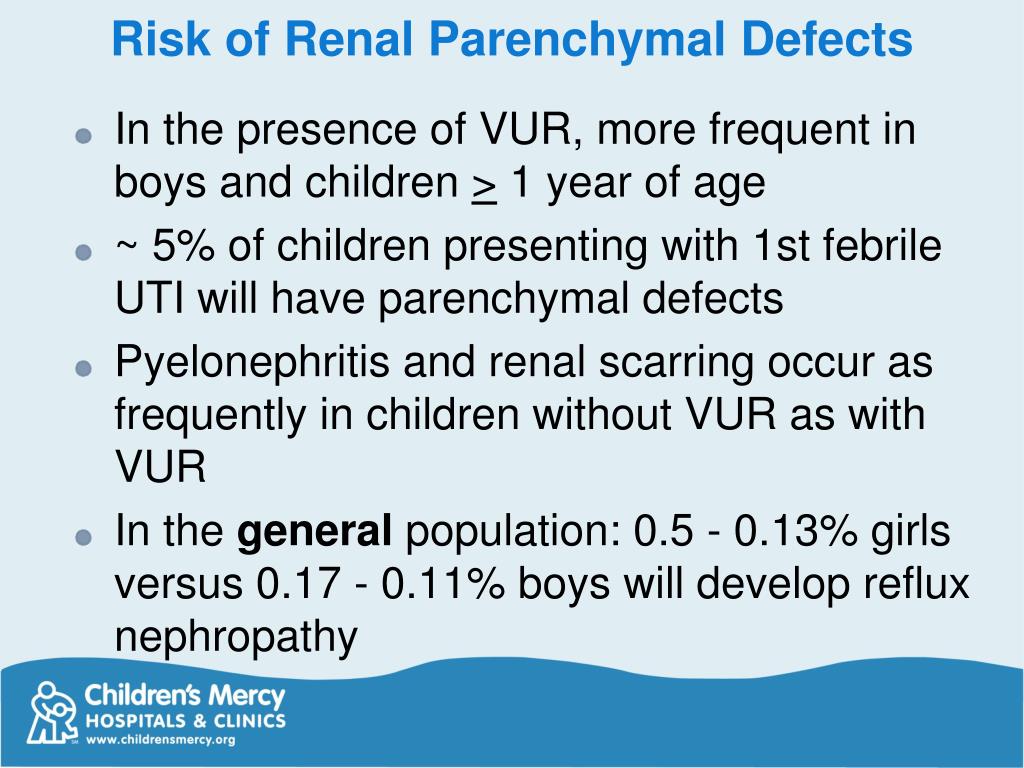
Sensitivities for acute pyelonephritis are difficult to determine because Tc-99m DMSA is considered the gold standard. Most frequently, cortical scanning is done in children with acute pyelonephritis, but it also may be performed as part of the workup in patients with vesicoureteral reflux who have no evidence of active pyelonephritis.
When is outpatient therapy indicated for acute pyelonephritis (kidney infection)?
· Timely initiation of suitable antibiotics and percutaneous catheter drainage (PCD) are of utmost importance as treatment. 5,6 To maximize nephron sparing, PCD has been widely adopted and in conjunction with medical treatment has succeeded in lowering the mortality rate to 13.5%. 4 Any empiric antimicrobial regimen should primarily target gram-negative bacteria.

What is the best treatment for pyelonephritis?
Outpatient oral antibiotic therapy with a fluoroquinolone is successful in most patients with mild uncomplicated pyelonephritis. Other effective alternatives include extended-spectrum penicillins, amoxicillin-clavulanate potassium, cephalosporins, and trimethoprim-sulfamethoxazole.
What is the first line treatment for pyelonephritis?
Fluoroquinolones (FQ) are the first line empiric treatment for acute pyelonephritis. Fluoroquinolones (FQ) are the first line empiric treatment for acute pyelonephritis.
What is the drug of choice for pyelonephritis?
The penicillins (amoxicillin) and first-generation cephalosporins are the drugs of choice for chronic pyelonephritis because of good activity against gram-negative rods and good oral bioavailability.
Is percutaneous drainage the new gold standard in the management of emphysematous pyelonephritis?
Conclusions: Percutaneous drainage should be part of the initial management strategy for emphysematous pyelonephritis. This strategy is associated with a lower mortality than medical management or emergency nephrectomy. Delayed elective nephrectomy may be required in some patients.
What is the safest antibiotic for kidney infection?
Commonly used antibiotics for kidney infections include ciprofloxacin, cefalexin, co-amoxiclav or trimethoprim. Painkillers such as paracetamol can ease pain and reduce a high temperature (fever). Stronger painkillers may be needed if the pain is more severe.
How is pyelonephritis diagnosed and treated?
To diagnose the problem, your health care provider may use the following tests:A medical history. ... Physical exam. ... Urinalysis. ... Urine culture. ... Blood cultures. ... Computed tomography (CT scan). ... Kidney ultrasound.More items...
Is ceftriaxone good for pyelonephritis?
The results demonstrate that ceftriaxone is an effective drug when given once a day intramuscularly to out-patients with acute pyelonephritis. in a dose of 1 g every 24 h is an effective and safe antibiotic in the treatment of adult women with acute bacterial pyelonephritis.
Does doxycycline treat pyelonephritis?
Eleven patients with refractory chronic pyelonephritis were given 14 courses of long-term therapy with doxycycline. Good results were obtained in 7 instances, while the results were poor in 3 instances and inde- terminate in 4.
How long is treatment for pyelonephritis?
In the current International Clinical Practice Guidelines for the treatment of acute pyelonephritis, the recommended duration of treatment for pyelonephritis is 7 days for fluoroquinolones, 10–14 days for β-lactams and 14 days for trimethoprim/sulfamethoxazole.
How long does it take for pyelonephritis to be adjusted?
People with pyelonephritis may have bacteria in their blood as well as their urine. Antibiotics are started prior to the culture results and will be adjusted once the bacterial species is identified in 24 to 48 hours.
What are the causes of pyelonephritis?
A man is more likely to develop the problem if his prostate is enlarged, a common condition after age 50. Both men and women are more likely to develop pyelonephritis if they have any of the following conditions: 1 An untreated urinary tract infection 2 Diabetes 3 Nerve problems that affect the bladder 4 Kidney stones 5 A bladder tumor 6 Abnormal backflow of urine from the bladder to the kidneys, called vesicoureteral reflux 7 An obstruction related to an abnormal development of the urinary tract
What age do men develop pyelonephritis?
A man is more likely to develop the problem if his prostate is enlarged, a common condition after age 50. Both men and women are more likely to develop pyelonephritis if they have any of the following conditions: Abnormal backflow of urine from the bladder to the kidneys, called vesicoureteral reflux.
How do you know if you have pyelonephritis?
The two primary symptoms of pyelonephritis are pain in one flank, the area just beneath the lower ribs in the back, and fever. The pain can travel around the side toward the lower abdomen. There also can be shaking chills and nausea and vomiting. The urine may be cloudy, tinged with blood or unusually strong or foul-smelling.
Does a test in the bladder increase the risk of pyelonephritis?
Tests or procedures that involve the insertion of an instrument into the bladder also increase the risk of urinary tract infections and pyelonephritis.
Can pyelonephritis cause kidney damage?
A single episode of uncomplicated pyelonephritis rarely causes permanent kidney damage in an otherwise healthy adult. However, repeated episodes of pyelonephritis can cause chronic (long-lasting) kidney disease in children, people with diabetes, and adults who have structural abnormalities of the urinary tract, or nerve diseases that disrupt bladder function. Pyelonephritis can become chronic if an infection cannot be cleared easily, as in a person with a kidney stone or a developmental abnormality of the urinary system.
What is the treatment for pyelonephritis?
Outpatient treatment is appropriate for patients who have an uncomplicated infection that does not warrant hospitalization. Oral antibiotics are used to treat patients with mild to moderate illness. (See Table 2, below, for a description of outpatient treatments for pyelonephritis.)
How long does it take to get rid of pyelonephritis?
For uncomplicated pyelonephritis, the American College of Physicians (ACP) recommends administering a short course of fluoroquinolones (5 to 7 days) or trimethoprim-sulfamethoxazole (TMP-SMX; 14 days), based on antibiotic susceptibility. [ 26]
How long does it take to get ciprofloxacin for pyelonephriti
Although the guidelines recommend either 14 days of TMP-SMX or 7 days of ciprofloxacin for the treatment of pyelonephritis, a study in 272 women with susceptible E coli pyelonephritis reported similar clinical outcomes with 7 days of TMP-SMX therapy compared with 7 days of ciprofloxacin.
What should be considered when choosing an empirical antibiotic regimen?
In choosing an empirical antibiotic regimen, consideration should include the local antibiogram and drug-resistance rates. For example, in a community with growing fluoroquinolone resistance, agents in that class may not be an ideal first-line choice. In light of increasing resistance, short courses of treatment are preferred. In one clinical trial, a 7-day course of oral ciprofloxacin was shown to be a safe and successful treatment for acute pyelonephritis in women, including older women and those with more severe infection. [ 25]
What are the host factors for acute pyelonephritis?
The decision regarding admission of a patient with acute pyelonephritis depends on age; host factors, such as immunocompromising chemotherapy or chronic diseases, known urinary tract structural abnormalities, renal calculi, recent hospitalization, or urinary tract instrumentation; and the patient's response to ED therapy.
Can pyelonephritis be treated in the ED?
They must be otherwise healthy and must not be pregnant. In addition, they must be treated initially in the emergency department (ED) with vigorous oral or intravenous (IV) fluids, antipyretic pain medication, and a dose of parenteral antibiotics. Studies have shown that outpatient therapy for selected patients is as safe as inpatient therapy for a comparable group of patients and is much less expensive.
Can a female patient have pyelonephritis?
For female patients suspected of having acute pyelonephritis, the IDSA guidelines recommend sending urine for culture and susceptibility testing and then starting empirical antibiotic therapy. [ 3]
What is the most common etiologic cause of pyelonephritis?
The most common etiologic cause is infection with Escherichia coli. The combination of the leukocyte esterase test and the nitrite test (with either test proving positive) has a …. There are approximately 250,000 cases of acute pyelonephritis each year, resulting in more than 100,000 hospitalizations. The most common etiologic cause is infection ...
How long after antibiotics should you repeat a urine culture?
Urine culture should be repeated one to two weeks after completion of antibiotic therapy. Treatment failure may be caused by resistant organisms, underlying anatomic/functional abnormalities, or immunosuppressed states. Lack of response should prompt repeat blood and urine cultures and, possibly, imaging studies.
Is fluoroquinolone effective for pyelonephritis?
Outpatient oral antibiotic therapy with a fluoroquinolone is successful in most patients with mild uncomplicated pyelonephritis. Other effective alternatives include extended-spectrum penicillins, amoxicillin-clavulanate potassium, cephalosporins, and trimethoprim-sulfamethoxazole. Indications for inpatient treatment include complicated infections, ...
What is the best treatment for acute pyelonephritis?
Patients hospitalized with acute pyelonephritis should be treated with one of three initial intravenous therapies: a fluoroquinolone; an aminoglycoside with or without ampicillin; or an extended-spectrum cephalosporin with or without an aminoglycoside. B. 29.
When should blood cultures be obtained for pyelonephritis?
Blood cultures should be obtained in patients with acute pyelonephritis only if there is diagnostic uncertainty, the patient is immunosuppressed, or a hematogenous source is suspected.
How long does it take to treat UTI in men?
Differences between UTI in men and women support the classification of male acute pyelonephritis as complicated. Men younger than 60 years without obstruction, renal abnormalities, or prostatitis respond well to 14 days of antibiotic therapy. 2 Men who have recurrent UTIs require a six-week regimen. Men with acute prostatitis require four weeks of treatment with an antibiotic that has high penetration into prostatic tissue, such as doxycycline (Vibramycin), TMP-SMX, or a fluoroquinolone; men with chronic prostatitis require six to 12 weeks of such therapy. 2, 38 The optimal duration of treatment for hospitalized patients is 14 days.
What is pyelonephritis in the urinary tract?
Acute pyelonephritis is an infection of the upper urinary tract, specifically the renal parenchyma and renal pelvis ( Figure 1). Acute pyelonephritis is considered uncomplicated if the infection is caused by a typical pathogen in an immunocompetent patient who has normal urinary tract anatomy and renal function. Misdiagnosis can lead to sepsis, renal abscesses, and chronic pyelonephritis that may cause secondary hypertension and renal failure. Risk factors for complicated acute pyelonephritis are those that increase susceptibility or reduce host response to infections ( Table 1). 1, 2
How many cases of pyelonephritis are there in the US each year?
Approximately 250,000 cases of acute pyelonephritis occur each year, resulting in more than 100,000 hospitalizations. 3 Women are approximately five times more likely than men to be hospitalized with this condition (11.7 versus 2.4 hospitalizations per 10,000 cases, respectively); however, women have a lower mortality rate than men (7.3 versus 16.5 deaths per 1,000 cases, respectively). 4 Acute pyelonephritis occurs in 1 to 2 percent of pregnant women, increasing the risk for premature labor and low-birth-weight infants. 5
Why is pyelonephritis considered a complicated disease?
2 Acute pyelonephritis is considered complicated in men because they have a higher probability of urinary tract abnormalities, prostatic enlargement causing urethral obstruction with incomplete voiding, or an age-related decrease of antibacterial activity in prostatic secretions.
How long does it take to get antibiotics for pyelonephritis?
A seven- to 14-day course of antibiotics is effective in women who are immunocompetent and do not have underlying illness. 1, 27, 30 Studies 29, 33, 34 suggest that therapy lasting only five to seven days is comparable to seven to 14 days in terms of clinical and bacteriologic outcome in patients with mild pyelonephritis and in those having a dramatic initial response to therapy. Acute pyelonephritis associated with immunosuppressive states responds well to a 14- to 21-day course of a fluoroquinolone or TMP-SMX. 2 Post-treatment urine cultures are recommended in all patients at the follow-up visit, one to two weeks after completion of antibiotic therapy. 35
What is the best treatment for pyelonephritis?
Acute pyelonephritis may be accompanied by septicaemia and is usually marked by fever and loin pain. In such patients it is advisable to start with co-amoxiclav i.v. or alternatively gentamicin (perhaps plus amoxicillin) i.v. If oral therapy is considered suitable, co-amoxiclav or ciprofloxacin is recommended for 2 weeks. This is an infection of the kidney substance and so needs adequate blood as well as urine concentrations, although a switch to an oral agent (guided by the results of susceptibility testing) to complete the course is recommended after the patient has clinically improved.
What is the cause of pyelonephritis?
Acute pyelonephritis occurs as a result of infection of the kidney, usually from bacteria.74,77 Most pediatric cases occur in boys, and most adult cases occur in women. Infections can be ascending, from lower urinary tract infection, or hematogenous, from sepsis or endocarditis. 74,77,92,93
What are the symptoms of pyelonephritis in cows?
First signs may be blood-tinged urine in a seemingly normal cow. Untreated infections usually become chronic with discomfort, frequent urination, weight loss, anorexia, hematuria or pyuria and loss of production in dairy animals. Chronic cases are characterized by diarrhea, polyuria, polydipsia, stranguria, and anemia. Relapses are common, and some infections are severe and fatal. Diagnosis of pyelonephritis is based on clinical signs and urinalysis (proteinuria and hematuria) and rectal or vaginal palpation (assessing ureteral enlargement).
What is pyelonephritis on a CT?
Acute pyelonephritis is infection of the kidney ; patients often present with fever, chills, and flank pain and tenderness. It is most often due to ascending retrograde infection via the bladder, ureter, and collecting system with subsequent infection of the renal parenchyma. CT findings include a normal-appearing kidney; focal areas of striated or wedge-shaped hypoattenuation in the kidney, resulting in a heterogeneous nephrogram (Fig. 20-7); a “striated nephrogram” on delayed postcontrast images because of stasis of contrast material within edematous tubules; enlargement of the kidney; perinephric fat stranding; and renal pelvic and ureteral thickening with hyperenhancement. Sometimes, associated hydroureteronephrosis (dilation of the collecting system and ureter), renal infarction, or renal or perinephric abscess formation may be seen.
What is the renal size of a dog with pyelonephritis?
Typically, there is mild to moderate pyelectasia.72 The mean diameter of the renal pelvis with pyelonephritis was 3.6 mm in dogs and 4.0 mm in cats.31 However, this range is quite wide, with overlap with other nonobstructive or obstructive renal diseases, and even with normal animals. 31 More important, the shape of the renal pelvis is usually distorted with infection, resulting in blunted and asymmetric pelvic diverticula, seen both on excretory urography and ultrasound ( Figs. 41.24 and 41.25). Additionally, on ultrasound imaging, echogenic debris may be observed in the renal pelvis and proximal ureter rather than anechoic urine, and the renal pelvis may be surrounded by an echogenic rim caused by fibrotic change.72-74 The echogenicity of the renal cortex may be uniformly or heterogeneously increased. In severe acute pyelonephritis, regional inflammation of the perirenal fat results in a hyperechoic rim around the kidney and proximal ureter (see Fig. 41.25 ), often with a small amount of retroperitoneal effusion. Thickening of the proximal ureteral wall and mild ureteral dilation without evidence of intraluminal obstruction are observed commonly. Chronic pyelonephritis is difficult to distinguish from other chronic renal diseases, because it is characterized by small, irregularly shaped kidneys with mild pyelectasia. 72
Can pyelonephritis cause scarring?
Therefore recurrent infections often occur and lead to significant damage and scarring. This process is a significant cause of long-term morbidity, causing hypertension and chronic renal failure.
What Is Pyelonephritis?
Symptoms
Diagnosis
Expected Duration
Specialist to consult
Prevention
Treatment
When to Call A Professional
- If your doctor is concerned that you have a kidney infection, he or she will ask you about other medical problems, any past infections and your recent symptoms. He or she will check your vital signs (temperature, heart rate, blood pressure), and will press on your abdomen and flanks to see if there is tenderness near the kidney. In women, the symptoms of pyelonephritis may be similar …
Prognosis
- Most patients with uncomplicated cases of pyelonephritis find that their symptoms begin to improve after one to two days of treatment with antibiotics. However, even after symptoms improve, antibiotics are usually prescribed to complete a 10 to 14 day course.
Further Information
- To help prevent pyelonephritis if you have had a previous episode or are at risk: 1. Drink several glasses of water each day. Water discourages the growth of infection-causing bacteria by flushing out your urinary tract. This flushing also helps to prevent kidney stones, which can increase the risk of pyelonephritis. 2. If you are a woman, wipe from front to back. To prevent the spread of in…