How do you treat V tach with a pulse?
Sep 02, 2021 · POT syndrome (POTS, postrual orthostatic tachycardia syndrome) is a nervous system disorder that causes lightheadedness and fainting when a person stands up. Treatment may include increasing blood volume and regulating circulatory problems that …
How to fix Vtach?
Jun 06, 2018 · The PROCAMIO trial was the first randomized trial to compare the use of procainamide and amiodarone in stable, sustained, monomorphic wide complex tachycardia (most likely ventricular). 9 This was a multicenter, prospective trial that included 74 patients with regular WCT who presented to the ED and met the inclusion criteria: HR > 120/min
What to do for V tach?
May 03, 2019 · Stable V-tach should certainly be addressed to prevent the rhythm from becoming more erratic and to prevent the patient from becoming symptomatic. Anti-arhythmic medications, such as adenosine, are usually given. Synchronized cardioversion is typically recommended as well for patients who have either narrow or regular QRS complexes.
Is V tach regular or irregular?
Ablation of ventricular tachycardia has a long history of safety and success. For some patients, ablation completely cures the abnormal rhythm, and no other treatment is needed. Ablation can also improve treatment with an implantable cardioverter defibrillator. Implantable Cardioverter Defibrillator. An ICD is a device that is implanted under the skin.
What is the first thing to do for V tach?
What MED do you give for V tach?
What is the first line antiarrhythmic for V tach with a pulse?
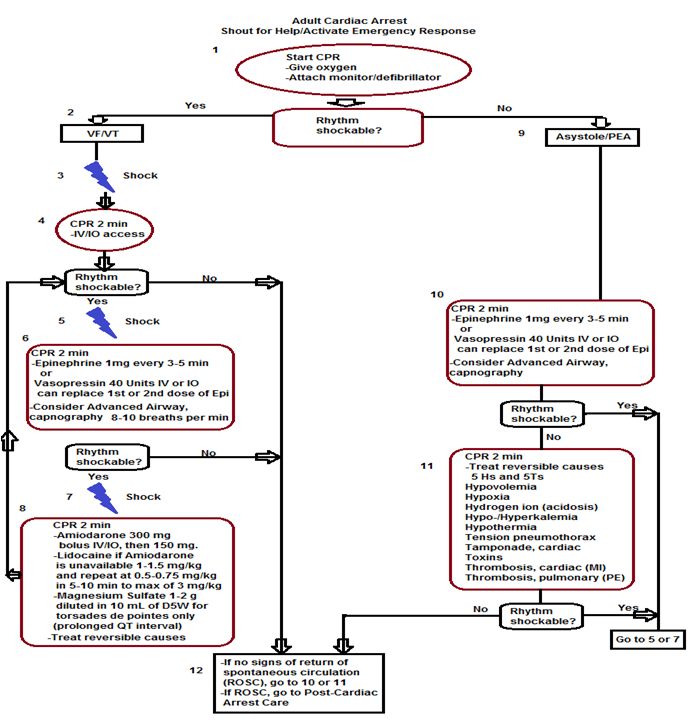
How is Vtach ACLS treated?
How is asystole treated?
Which drug is considered first-line treatment for asystole or PEA?
What causes ventricular tachycardia?
Your heart rate is regulated by electrical signals sent to your heart muscle. Certain conditions can interfere with normal electrical signals and cause ventricular tachycardia:
What are the signs and symptoms of ventricular tachycardia?
Ventricular tachycardia goes away on its own in 30 seconds. However, sustained ventricular tachycardia can last more than 30 seconds and requires emergency treatment.
How is ventricular tachycardia diagnosed?
Your doctor will ask you about your symptoms and take a complete medical history. They may order tests that include:
What can you do to prevent ventricular tachycardia?
Following your doctor’s treatment recommendations can help you prevent or manage episodes of the disease. In some cases, the causative factor (cardiovascular disorder, tumor, drugs, electrolyte imbalance, etc.) may need to be addressed and treated. It is also advised to adopt a healthy lifestyle that includes:
Top Best Treatment of Ventricular Tachycardia Related Articles
This procedure is used to treat abnormal heart rhythms. Depending on the type of arrhythmia and the presence of other heart disease, a nonsurgical ablation or a surgical ablation, may be performed. During a catheter ablation, catheters are advanced to the heart via blood vessels in the groin, neck, and arm.
Why do you need stable V-tach?
Stable V-tach should certainly be addressed to prevent the rhythm from becoming more erratic and to prevent the patient from becoming symptomatic. Anti-arhythmic medications, such as adenosine, are usually given.
Is V-tach stable?
When V-tach is described as being stable, it occurs with very few if any symptoms. The patient will still be able to talk and generally function and may even have mostly normal vital signs other than heart rate.
What is the rate of heartbeat in a patient with ventricular tachycardia?
Tachycardia usually refers to any heart rhythm over 120 beats per minute, but emergency treatments are usually considered when the heart rate gets to 150 beats per minute or more.
How to manage tachycardia?
Prior to this point, the tachycardia can usually be managed by attending physicians or by family physicians through medication changes. If you’re caring for a patient in your hospital or clinic who has a fast heart rhythm, you must first determine what the EKG is showing and whether your patient is stable or unstable.
Can ventricular tachycardia be caused by medication?
Many conditions, diseases and even medications can cause ventricular tachycardia, but not all episodes of tachycardia may be immediately serious. For example, a certain medication may simply need to be stopped, or the root cause of a disease may need to be addressed to get the heart back to functioning correctly.
What are the symptoms of unstable V-tach?
In unstable V-tach, the patient will present with symptoms. Mental symptoms, such as confusion or loss of consciousness, may be the first changes noted. Without quick treatment, complete hemodynamic collapse is possible, which could lead to the need for CPR and emergency treatments.
How many beats per minute is tachycardia?
Tachycardia usually refers to any heart rhythm over 120 beats per minute, but emergency treatments are usually considered when the heart rate gets to 150 beats per minute or more. Prior to this point, the tachycardia can usually be managed by attending physicians or by family physicians through medication changes.
Does ablation help with ventricular tachycardia?
Ablation of ventricular tachycardia has a long history of safety and success. For some patients, ablation completely cures the abnormal rhythm, and no other treatment is needed. Ablation can also improve treatment with an implantable cardioverter defibrillator.
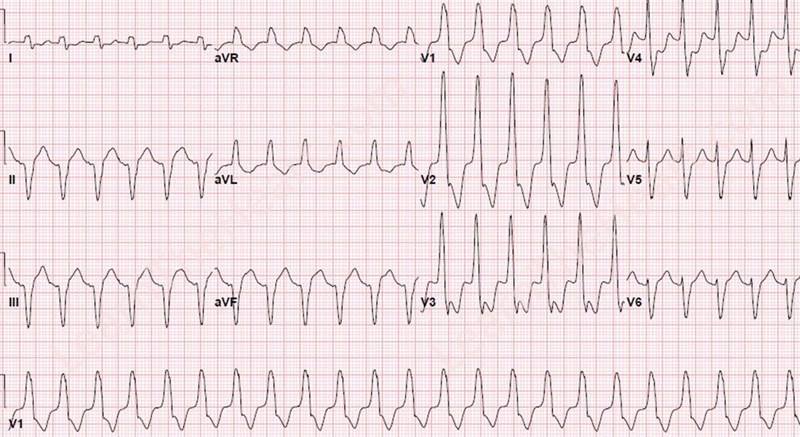
Can tachycardia be recorded on EKG?
Ventricular Tachycardia recorded on EKG. Your doctor may refer you to a specialist to electrophysiology testing. During the test, catheters (long, thin tubes) with electrodes are inserted through the veins at the groin and placed directly in the heart.
What is the heart rate of ventricular tachycardia?
Ventricular tachycardia starts in the heart’s lower chambers. Most patients who have ventricular tachycardia have a heart rate that is 170 beats per minute or more. Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission.
What causes tachycardia in the heart?
When something goes wrong and signals are sent too quickly, it can cause tachycardia. Most patients with ventricular tachycardia have another heart problem, such as coronary artery disease, high blood pressure, an enlarged heart (cardiomyopathy) or heart valve disease.
What is the second step of a cardiac ablation procedure?
In the second step, the doctor uses a catheter with a special tip that emits a high-frequency form of electrical current. The current is used to destroy a tiny amount of tissue in the area of the ventricle where the abnormal rhythm begins. This is called an ablation procedure.
What is the procedure called when you have a V-tach?
Since long-term medication use can have side effects, many patients opt for a minimally invasive procedure called cardiac ablation. In this procedure, physicians use catheters to find and trigger V-tach episodes. This helps them locate the “spot” in the ventricle where they’re originating.
What is the first step in ventricular tachycardia treatment?
“The first step in ventricular tachycardia treatment is to figure out why someone has VT in the first place, ” says Gregory E. Supple, MD, an electrophysiologist at Penn Medicine. “It’s a spectrum of diseases.”
What are the symptoms of V-tach?
V-tach occurs when your pulse rate is more than 100 beats per minute, and you have at least three irregular heartbeats, or arrhythmias, in a row. Besides palpitations, V-tach can cause symptoms like: 1 Chest pain 2 Lightheadedness 3 Fainting
What does V-tach mean?
V-tach occurs when your pulse rate is more than 100 beats per minute, and you have at least three irregular heartbeats, or arrhythmias, in a row. Besides palpitations, V-tach can cause symptoms like: Chest pain. Lightheadedness. Fainting. Untreated V-tach can be dangerous: It’s a major cause of sudden cardiac death.
Is V-tach idiopathic?
While rare, V-tach can be idiopathic, meaning there is nothing else wrong with the heart. But most of the time, V-tach is a result of other heart problems, such as: Dr. Supple also sees many cases of V-tach that have developed as a result of scar tissue on the heart from a heart attack or heart surgery.
Is V-tach a heart disease?
While rare, V-tach can be idiopathic, meaning there is nothing else wrong with the heart. But most of the time, V-tach is a result of other heart problems, such as: An enlarged heart. Valve disease. Coronary artery disease.
What causes V-tach in heart?
But most of the time, V-tach is a result of other heart problems, such as: An enlarged heart. Valve disease. Coronary artery disease. High blood pressure. Dr. Supple also sees many cases of V-tach that have developed as a result of scar tissue on the heart from a heart attack or heart surgery.
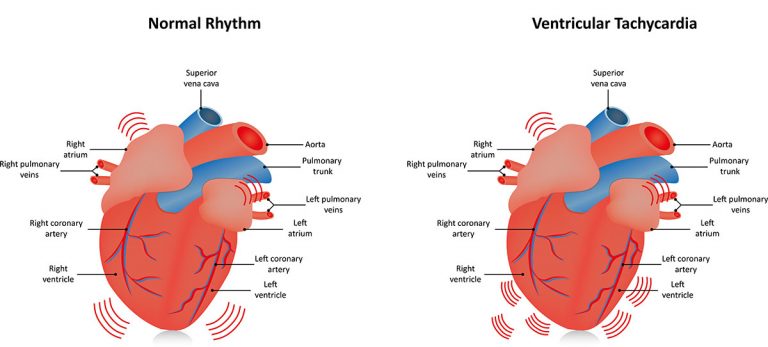
Where does ventricular tachycardia start?
Ventricular tachycardia begins in the lower chambers (ventricles) and is quite fast. When it lasts only a few seconds, ventricular tachycardia may cause no problems.
What is a CPVT?
Catecholaminergic polymorphic ventricular tachycardia (CPVT) is a genetic condition that can cause a fast abnormal heart beat from the ventricles. CPVT may cause a loss of consciousness or sudden death due to the lack of blood pumped to the body.
What causes tachycardia in the heart?
Ventricular tachycardia most often occurs when the heart muscle has been damaged and scar tissue creates abnormal electrical pathways in the ventricles. Causes include: 1 Heart attack 2 Cardiomyopathy or heart failure 3 Myocarditis 4 Heart valve disease
Can ventricular tachycardia cause syncope?
When it lasts only a few seconds, ventricular tachycardia may cause no problems. But when sustained, vent ricular tachycardia can lower the blood pressure, resulting in syncope (fainting) or lightheadedness. Ventricular tachycardia can also lead to ventricular ...
Can a person with no heart disease have ventricular tachycardia?
Sometimes, people with no known heart disease can develop ventricular tachycardia, often due to an irritable focus — when cells outside the sinus node start generating an electrical impulse automatically on their own. This form of ventricular tachycardia is easier to address and is usually not life threatening.
Can tachycardia cause lightheadedness?
When it lasts only a few seconds, ventricular tachycardia may cause no problems. But when sustained, ventricular tachycardia can lower the blood pressure, resulting in syncope (fainting) or lightheadedness. Ventricular tachycardia can also lead to ventricular fibrillation (a life-threatening arrhythmia) and cardiac arrest.
Where does V-Tach originate?
V-Tach signals originate from the ventricles rather than the SA or AV node and creates a contraction that occurs before the SA node has a chance to send out a signal…. AKA a Premature Ventricular Contraction (PVC). A PVC can be harmless but multiple PVCs in a row can cause issues. More than 3 PVCs in a row is labeled V-Tach.
What are the symptoms of a V-tach?
Signs and symptoms of Ventricular Tachycardia (V-Tach) The most common sign or symptom of V-Tach is palpitations, but can also be chest pain, dizziness, lightheadedness, dyspnea, nausea diaphoresis, and/or loss of consciousness. If a patient is not in sustained V-Tach, they may not have any signs or symptoms, making it hard to recognize this ...
Is ventricular tachycardia POLYmorphic or MONOmorphic?
Note: The waves are the same height and width thus MONOmorphic. Note: The waves vary in height and width thus POLYmorphic. In Ventricular Tachycardia, there aren’t any P waves… because the atria aren’t sending signals or contracting properly!
Why are there no P waves in ventricular tachycardia?
In Ventricular Tachycardia, there aren’t any P waves… because the atria aren’t sending signals or contracting properly! The T waves are lost in the QRS so you can’t measure things like the QT interval. The rate is regular and faster than 100 beats per minute.
What is VT on EKG?
Ventricular Tachycardia can be a life-threatening arrhythmia. Usually referred to as V-Tach or VT, this arrhythmia is easy to recognize on an EKG/ECG. It is defined as a heart rate faster than 100 bpm, with re-entry electrical impulses in the ventricles causing them to contract giving the EKG/ECG a slinky-like wide complex QRS.
How long can a V-Fib last?
This can cause hypotension and decreased myocardial perfusion which can lead to Ventricular Fibrillation (V-Fib). The body can only sustain V-Fib for 6 minutes after which death occurs. So it is safe to say that this is a scary rhythm that as a nurse, you need to know about. (GIPHY)
Can you recognize a V-tach without an EKG?
If a patient is not in sustained V-Tach, they may not have any signs or symptoms, making it hard to recognize this arrhythmia without an EKG/ECG. Then again if it is not sustained and is asymptomatic it probably won’t need any intervention anyway.
Can antiarrhythmics be used for VT?
Combinations of these therapies are often used when structural heart disease is present. Antiarrhythmic drugs have traditionally been the mainstays of treatment for clinically stable patients with VT. However, some patients experience unacceptable side effects or frequent recurrence of VT with drug therapy.
Does polymorphic VT recur?
Polymorphic VT in stable patients typically terminates on its own. However, it tends to recur. After sinus rhythm returns, the ECG should be analyzed to determine whether the QT interval is normal or prolonged. Polymorphic VT in patients with a normal QT interval is treated in the same manner as monomorphic VT.
What are the symptoms of tachycardia?
Unstable patients have signs or symptoms of insufficient oxygen delivery to vital organs as a result of the tachycardia. Such manifestations may include the following: 1 Dyspnea 2 Hypotension 3 Altered level of consciousness
Can VT cause hemodynamic collapse?
Sustained ventricular tachycardia (VT) may lead to hemodynamic collapse. Consequently, these patients require urgent conversion to sinus rhythm. The strategy for conversion depends on whether the patient is hemodynamically stable or unstable.
Can a catheter ablation be used for cardiomyopathy?
In patients with structurally normal hearts, catheter ablation can eliminate symptomatic VT arising from the right or left ventricle. Catheter ablation may also be used in patients with cardiomyopathy. The goal in these cases is to reduce the arrhythmia burden and thereby minimize the number of ICD shocks.
Can tachycardia cause cardiomyopathy?
Prolonged exposure to this (or any other) tachycardia may cause a tachycardia-induced cardiomyopathy, which typically improves with medical or ablative treatment of the VT. [ 19] Pulseless VT. Pulseless VT, in contrast to other unstable VT rhythms, is treated with immediate defibrillation.
What is a Ventricular Arrhythmia (VTACH or VFIB)?
Ventricular arrhythmias are those originating from the ventricles. Since the ventricles are responsible for pumping blood to the lungs and throughout the body, ventricular arrhythmias are often deadly.
What Causes Ventricular Arrhythmias?
Ventricular arrhythmias are usually caused by coronary artery disease (CAD). Any lack of blood flow (i.e. a heart attack) will cause ventricular cells to be deprived of oxygen. When the cardiac myocytes become hypoxic, they become irritable and prone to firing when they shouldn’t, which leads to PVCs, VTACH, and even VFIB.
IDENTIFYING VTACH
VTACH is a tachycardic rhythm originating within the ventricles. This produces very fast heart rates which may or may not be perfusing.
MONOMORPHIC VTACH
Monomorphic VTACH originates from the same ventricular focus. This means that the same ventricular cells or region of cells are functioning as the pacemaker for this rhythm.
POLYMORPHIC VTACH
Polymorphic VTACH originates from multiple different ventricular foci.
QT Prolongation
QT prolongation is the main cause of Torsades and is defined when the QT interval is >440ms in men and >460ms in women.
IDENTIFYING VFIB
VFIB is similar to polymorphic VTACH, but on a much wider scale. Essentially, all of the ventricular cells are irritable and it produces a disorganized chaotic arrhythmia that does not perfuse the body and is a CODE BLUE.