- Catheter ablation. This procedure is often used when an extra electrical pathway is responsible for an increased heart rate.
- Medications. Anti-arrhythmic medications taken by mouth may prevent a fast heart rate when taken regularly. ...
- Pacemaker. Some types of tachycardias may be treated with a pacemaker. ...
- Implantable cardioverter. ...
- Surgery. ...
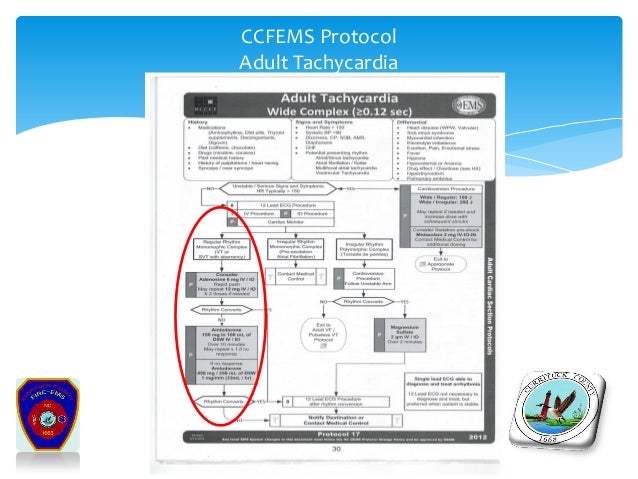
What is the first step in managing unstable tachycardia?
Jul 17, 2017 · The first step in managing unstable tachycardia is determining whether or not the patient has a pulse. In situations where the patient both has a pulse and is unstable, prompt synchronized cardioversion should be performed. For a more detailed, step-by-step description of the Unstable Tachycardia Algorithm, see below:
How is tachycardia treated in cardiogenic shock?
May 16, 2021 · For the purposes of emergency treatment of a hemodynamically unstable patient in the field, professionals consider all instances of wide-complex tachycardia as VT. If a patient shows signs of immediate danger (systolic blood pressure below 90 mm/Hg, loss of consciousness, confusion, or only able to find a carotid pulse), synchronized cardioversion is …
What are the treatment options for adult tachycardia?
Jun 06, 2018 · The current literature and guidelines both support Procainamide as a first-line agent. The PROCAMIO trial was the first randomized trial to compare the use of procainamide and amiodarone in stable, sustained, monomorphic wide complex tachycardia (most likely ventricular). 9 This was a multicenter, prospective trial that included 74 patients with regular …
Can tachycardia be prevented?
Regularity: R-R intervals are regular, overall rhythm is regular. Rate: The rate is over 100 bpm but usually less than 150 bpm. P Wave: There is one P wave in front of every QRS.

What is the first line treatment for tachycardia?
Calcium channel blockers are typically used as the first line of treatment. However, some authors consider magnesium sulfate to be the drug of choice. Most patients with MAT require hospital admission to further manage their underlying cardiopulmonary diseases.Nov 16, 2019
What drugs treat stable tachycardia?
Adenosine is the primary drug used in the treatment of stable narrow-complex SVT (Supraventricular Tachycardia). Now, adenosine can also be used for regular monomorphic wide-complex tachycardia. When given as a rapid IV bolus, adenosine slows cardiac conduction particularly affecting conduction through the AV node.
When do you give adenosine vs amiodarone?
Note that amiodarone becomes the antiarrhythmic of choice (after failure of adenosine) if the patient's cardiac function is impaired and the ejection fraction is <40% or there are signs of congestive heart failure.Aug 22, 2000
What is the initial step in treating stable sinus tachycardia?
Initial management of stable wide-complex tachycardia Attach defibrillator pads to the patient. Ensure that the rhythm is stable. If any sign of hemodynamic instability: Deliver unsynchronized electrical cardioversion (at 200 J for biphasic defibrillators).Nov 10, 2021
How is unstable tachycardia treated?
Patients with unstable tachycardia should be treated immediately with synchronized cardioversion. If a pulseless tachycardia is present patients should be treated using the cardiac arrest algorithm. The AHA no longer provides specific shock dose recommendations for synchronized cardioversion.
What is a first line treatment for a patient with unstable bradycardia?
The American Heart Association recommends atropine sulfate as the first line of treatment for symptomatic bradycardia, regardless of whether it is due to AVB or not.Nov 23, 2019
Are adenosine and amiodarone the same?
Adenosine and amiodarone are antiarrhythmic agents that slow conduction, suppress premature heart beats, are used for the emergency treatment of supraventricular tachycardia [1–3], and are used for long-term treatment of atrioventricular tachycardia [4].Jun 14, 2017
What is amiodarone prescribed for?
Amiodarone is used to treat life-threatening heart rhythm problems called ventricular arrhythmias. This medicine is used in patients who have already been treated with other medicines that did not work well.Feb 1, 2022
Which drug is considered first-line treatment for asystole or PEA?
When treating asystole, epinephrine can be given as soon as possible but its administration should not delay initiation or continuation of CPR. After the initial dose, epinephrine is given every 3-5 minutes.
What is the correct treatment protocol for asystole?
Asystole is treated by cardiopulmonary resuscitation (CPR) combined with an intravenous vasopressor such as epinephrine (a.k.a. adrenaline). Sometimes an underlying reversible cause can be detected and treated (the so-called "Hs and Ts", an example of which is hypokalaemia).
What is the initial drug of choice for SVT treatment?
Adenosine (Adenocard) Adenosine is the first-line medical treatment for the termination of paroxysmal SVT.Apr 5, 2017
What is the treatment for wide complex tachycardia?
SVT will typically be managed with adenosine, Afib with WPWS will be treated with amiodarone, and Afib with aberrancy with either diltiazem or a beta-blocker. Typically, amiodarone will be the first-line drug of choice for all ventricular arrhythmias (VT, polymorphic VT, Vfib, etc.)Jul 1, 2021
What is the procedure to treat tachycardia?
Open-heart surgery may be needed in some cases to destroy an extra electrical pathway causing tachycardia. Tachycardia may also be treated with a maze procedure. During this procedure, a surgeon makes small incisions in heart tissue to create a pattern or maze of scar tissue.
How to diagnose tachycardia?
A thorough physical exam, medical history and testing is required to diagnose tachycardia. To diagnose your condition and determine the specific type of tachycardia, your doctor will evaluate your symptoms, perform a physical examination, and ask you about your health habits and medical history. Several heart tests also may be necessary ...
What is the most common test for tachycardia?
An electrocardiogram, also called an ECG or EKG, is the most common tool used to diagnose tachycardia. It's a painless test that detects and records your heart's electrical activity using small sensors (electrodes) attached to your chest and arms. An ECG records the timing and strength of electrical signals as they travel through your heart.
Why do doctors do stress tests?
Your doctor may recommend a stress test to see how your heart functions while it is working hard during exercise or when medication is given to make it beat fast.
What is an EKG?
An electrocardiogram (ECG or EKG) records the electrical signal from your heart to check for different heart conditions. Electrodes are placed on your chest to record your heart's electrical signals, which cause your heart to beat. The signals are shown as waves on an attached computer monitor or printer. An electrocardiogram, also called an ECG ...
How long does a Holter monitor monitor last?
Holter monitor. A Holter monitor uses electrodes and a recording device to track your heart's rhythm for 24 to 72 hours. Your doctor can print an electrocardiogram strip using the data on the recording device to see your heart's rhythm during the period you wore the monitor. Cardiac event monitor.
What is an ECG device?
Portable, or remote, ECG devices include: Holter monitor. This portable ECG device is carried in your pocket or worn on a belt or shoulder strap. It records your heart's activity for an entire 24-hour period, which provides your doctor with a prolonged look at your heart rhythms.
