Medication
Aug 14, 2018 · For late-onset and/or MDR factor patients, appropriate antibiotic options would include one or more of the following 37: • Antipseudomonal cephalosporins (eg, Cefepime, ceftazidime) • Antipseudomonal carbapenems (imipenem or meropenem) • Beta-lactam/beta-lactamase inhibitors ...
Therapy
The First-Line Treatment Of Community Acquired Pneumonia should be Penicillin. Eitan Kerem Department of Pediatrics and CF Center, Hadassah University Hospital, Jerusalem, Israel Community-acquired pneumonia (CAP) is a significant cause of childhood morbidity and mortality worldwide. Viral etiology is most common in young children and
Self-care
Community-Acquired Pneumonia. Diagnosis and Treatment of Adults with Community-acquired Pneumonia. An Official Clinical Practice Guideline. external icon The Infectious Diseases Society of America and American Thoracic Society developed these consensus guidelines. The Management of Community-Acquired Pneumonia in Infants and Children Older Than 3 Months …
Nutrition
Aug 01, 2021 · What is the first line treatment for hospital-acquired pneumonia? In general, for both hospital-acquired pneumonia (HAP) and VAP, 7 days of treatment with appropriate antibiotics/antibiotics is recommended. This duration may be shortened or lengthened depending on the clinical response of the individual.
What antibiotic is best for pneumonia?
Feb 01, 2006 · Consensus guidelines from ATS, 8 Infectious Diseases Society of America, 9 and Canadian Guidelines for the Initial Management of Community-Acquired Pneumonia 28 ( Figure 1 6) recommend initial...
What are the best treatments for pneumonia?
Aug 25, 2019 · Pneumonia should be treated with antibiotics. The antibiotic of choice for first line treatment is amoxicillin dispersible tablets. Most cases of pneumonia require oral antibiotics, which are often prescribed at a health centre.. Is ceftriaxone good for pneumonia?
Can pneumonia go away on its own?
Sep 30, 2021 · First-line antibiotics that might be selected include the macrolide antibiotics azithromycin ( Zithromax) or clarithromycin ( Biaxin XL ); or the tetracycline known as doxycycline. Other appropriate antibiotics may include the fluoroquinolone antibiotics such as levofloxacin ( Levaquin ); or combined therapy of a beta-lactam such as amoxicillin or …
How do you cure pneumonia?
Jun 16, 2020 · the most frequent treatments that qualify a patient as being immunocompromised include glucocorticoids, therapies that suppress b-cell or t-cell responses, chemotherapy for malignancy that causes neutropenia, conventional disease-modifying antirheumatic drugs, and biological agents used to treat a broad range of rheumatologic, dermatologic, gi, …

What is the first line drug of choice for pneumonia?
In otherwise uncomplicated pneumonia, azithromycin is the initial drug of choice, as it covers most of the potential etiologic agents, including Mycoplasma species. Compared with other drugs, this agent also causes less GI upset, and it has the potential for good compliance because of its reduced dosing frequency.
What is the best antibiotic to treat pneumonia?
The first-line treatment for pneumonia in adults is macrolide antibiotics, like azithromycin or erythromycin. In children, the first-line treatment for bacterial pneumonia is typically amoxicillin.Dec 9, 2021
What is the most common treatment for pneumonia?
Mild pneumonia can usually be treated at home with rest, antibiotics (if it's likely be caused by a bacterial infection) and by drinking plenty of fluids. More severe cases may need hospital treatment.
What is the 2nd line antibiotic for pneumonia?
For the second agent, an alternative to azithromycin is a respiratory fluoroquinolone (levofloxacin [750 mg daily] or moxifloxacin [400 mg daily]).Sep 3, 2021
What is the treatment for viral pneumonia?
There are no treatments for most viral causes of pneumonia. However, if the flu virus is thought to be the cause, antiviral drugs might be prescribed, such as oseltamivir (Tamiflu®), zanamivir (Relenza®), or peramivir (Rapivab®), to decrease the length and severity of the illness.Jun 15, 2020
Which is better doxycycline or azithromycin?
The beneficial effect continued until 2 months after treatment. In the azithromycin group three patients had diarrohea, while photosensitivity was seen in two patients using doxycycline. This study indicates that azithromycin is at least as effective as doxycycline in the treatment of acne.
What is the treatment for Covid pneumonia?
Are There Treatments for COVID-19 Pneumonia? Pneumonia may need treatment in a hospital with oxygen, a ventilator to help you breathe, and intravenous (IV) fluids to prevent dehydration.Jan 25, 2022
What are the 3 stages of pneumonia?
Stages of PneumoniaStage 1: Congestion. During the congestion phase, the lungs become very heavy and congested due to infectious fluid that has accumulated in the air sacs. ... Stage 2: Red hepatization. ... Stage 3: Gray hepatization. ... Stage 4: Resolution.
What is the treatment for pneumonia in the elderly?
If you are elderly, it is best to treat your pneumonia as early as possible. Your doctor will likely prescribe you antibiotics or over-the-counter medicines, or they may even suggest a hospital visit depending on how sick you are. Some of these medicines can be: Antibiotics for bacterial pneumonia.Mar 16, 2021
What IV antibiotics are used to treat pneumonia?
Cefuroxime and levofloxacin were the most commonly used IV agents, while orally-treated subjects primarily received a macrolide or levofloxacin.
Will Zithromax treat pneumonia?
Zithromax (azithromycin), also known as Z-Pak, is an antibiotic used to treat bacterial infections by inhibiting the growth of bacteria in the body. A Z-Pak is typically taken over a five-day course to treat infections such as bronchitis, pneumonia, and infections of the ears, lungs and other organs.
Is azithromycin used for pneumonia?
Azithromycin is used to treat certain bacterial infections (including sinusitis, pneumonia). It is a macrolide-type antibiotic. It works by stopping the growth of bacteria. This medication will not work for viral infections (such as common cold, flu).
What is the best medicine for pneumonia?
It may take time to identify the type of bacteria causing your pneumonia and to choose the best antibiotic to treat it. If your symptoms don't improve, your doctor may recommend a different antibiotic. Cough medicine.
How to get rid of pneumonia?
Get plenty of rest. Don't go back to school or work until after your temperature returns to normal and you stop coughing up mucus. Even when you start to feel better, be careful not to overdo it. Because pneumonia can recur, it's better not to jump back into your routine until you are fully recovered.
How long does it take for a person to feel tired after pneumonia?
Although most symptoms ease in a few days or weeks, the feeling of tiredness can persist for a month or more. Specific treatments depend on the type and severity of your pneumonia, your age and your overall health. The options include: Antibiotics. These medicines are used to treat bacterial pneumonia.
What tests are done to determine if you have pneumonia?
If pneumonia is suspected, your doctor may recommend the following tests: Blood tests . Blood tests are used to confirm an infection and to try to identify the type of organism causing the infection. However, precise identification isn't always possible. Chest X-ray.
What to do if pneumonia isn't clearing?
If your pneumonia isn't clearing as quickly as expected, your doctor may recommend a chest CT scan to obtain a more detailed image of your lungs. Pleural fluid culture. A fluid sample is taken by putting a needle between your ribs from the pleural area and analyzed to help determine the type of infection.
What is a sputum sample?
A sample of fluid from your lungs (sputum) is taken after a deep cough and analyzed to help pinpoint the cause of the infection. Your doctor might order additional tests if you're older than age 65, are in the hospital, or have serious symptoms or health conditions. These may include: CT scan.
How fast can you breathe in a minute?
Your breathing is rapid (30 breaths or more a minute) You need breathing assistance. Your temperature is below normal. Your heart rate is below 50 or above 100. You may be admitted to the intensive care unit if you need to be placed on a breathing machine (ventilator) or if your symptoms are severe.
What are the tests for pneumonia?
Historically, common laboratory tests for pneumonia have included leukocyte count, sputum Gram stain, two sets of blood cultures, and urine antigens. However, the validity of these tests has recently been questioned after low positive culture rates were found (e.g., culture isolates of S. pneumoniae were present in only 40 to 50 percent of cases). 9 Such low positive culture rates are likely due to problems with retrieving samples from the lower respiratory tract, previous administration of antibiotics, contamination from the upper airways, faulty separation of sputum from saliva when streaking slides or plates, 9 or viral etiology. Furthermore, sputum samples are adequate in only 52.3 percent of patients with CAP, and only 44 percent of those samples contain pathogens. 10 Nonetheless, initial therapy often is guided by the assumption that the presenting disease is caused by a common bacterial pathogen.
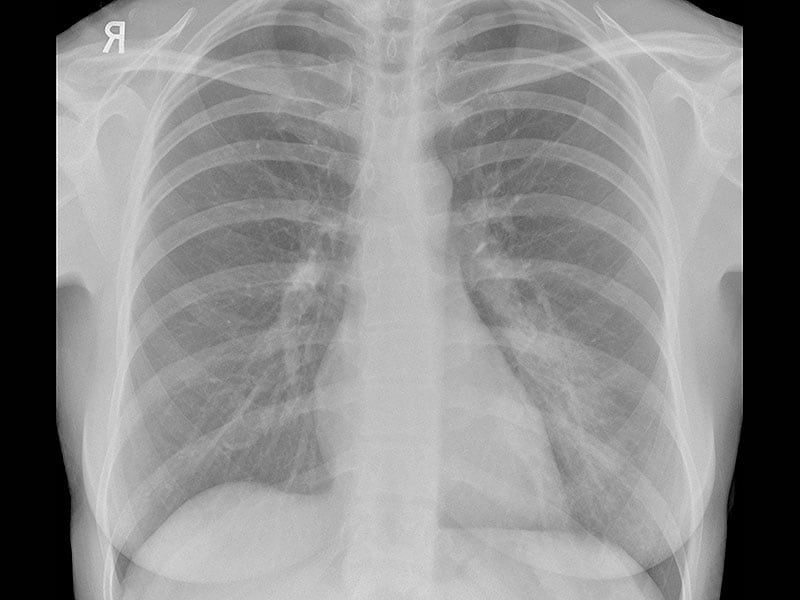
What is a chest radiograph for pneumonia?
Chest radiography (posteroanterior and lateral views) has been shown to be a critical component in diagnosing pneumonia. 8 According to the latest American Thoracic Society (ATS) guidelines for the diagnosis and treatment of adults with CAP, “all patients with suspected CAP should have a chest radiograph to establish the diagnosis and identify complications (pleural effusion, multilobar disease).” 8 Chest radiography may reveal a lobar consolidation, which is common in typical pneumonia; or it could show bilateral, more diffuse infiltrates than those commonly seen in atypical pneumonia. However, chest radiography performed early in the course of the disease could be negative.
What is CAP in healthcare?
Community-acquired pneumonia (CAP) is defined as pneumonia not acquired in a hospital or a long-term care facility.
What is pneumonia in lungs?
Pneumonia is an inflammation or infection of the lungs that causes them to function abnormally. Pneumonia can be classified as typical or atypical, although the clinical presentations are often similar. Several symptoms commonly present in patients with pneumonia.
When should fluoroquinolones be used?
Respiratory fluoroquinolones should be used when patients have failed first-line regimens, have significant comorbidities, have had recent antibiotic therapy, are allergic to alternative agents, or have a documented infection with highly drug-resistant pneumococci. C. 8, 9, 28, 29.
What are the goals of pharmacotherapy for CAP?
The primary goals of pharmacotherapy for patients with CAP include eradicating the causative pathogens, resolving the clinical signs and symptoms, minimizing hospitalization, and preventing reinfection. 23 – 27 Physicians should choose a medication based on the pharmacokinetic profile, adverse reactions, drug interactions, and cost-effectiveness. 23 – 27 Further, patient evaluation should focus on severity of illness, patient age, comorbidities, clinical presentation, epidemiologic setting, and previous exposure. 9 The majority of patients with CAP are treated empirically based on the most common pathogen (s) associated with the condition. 23 – 27
What percent of CAP cases are fatal?
S. pneumoniae, which accounts for 60 to 70 percent of all bacterial CAP cases, can affect all patient groups and can cause a fatal form of CAP. The alarming rate of resistance to many commonly used antibiotics raises great concern. Penicillin-resistant S. pneumoniae was uncommon in the early 1990s but has since become increasingly prevalent. 29, 31
What is CAP in medical terms?
Guidelines for the treatment of patients with community-acquired pneumonia (CAP) have been published by medical societies from several countries. These guidelines have improved the treatment and outcomes of patients with CAP, primarily by standardization of initial empirical therapy. But current society-published CAP guidelines exclude immunocompromised patients.
Why do we need a CT scan of the chest?
A CT scan of the chest will allow better definition of the extent of pulmonary infiltrate as well as better recognition of complications of pneumonia such as abscesses or pleural effusions. This information, gained by CT imaging of the chest, may help in the decision regarding hospitalization.
How many physicians are involved in the consensus document?
This consensus document was created by a multidisciplinary panel of 45 physicians with experience in the treatment of CAP in immunocompromised patients. The Delphi survey methodology was used to reach consensus.
Why is deescalation important?
Deescalation of therapy is important because continuing broad-spectrum therapy for the full duration of therapy is associated with selection of multidrug-resistant organisms, increased risk of toxicity, drug-drug interactions, and impaired antimicrobial stewardship for the entire community.
Is the ATS/IDSA CAP a generalization?
Therefore, this project aimed to give a perspective on the ATS/IDSA CAP recommendations related to the management of CAP outside the United States.
Is empirical therapy necessary for respiratory pathogens?
Initial empirical therapy active against these respiratory pathogens may be necessary only in selected patients presenting with specific epidemiologic, clinical, or immunologic risk factors for infection due to a particular pathogen. These risk factors and the specific pathogens that are involved are discussed below.
Diagnosis
Treatment
Clinical Trials
Lifestyle and Home Remedies
Specialist to consult
Preparing For Your Appointment