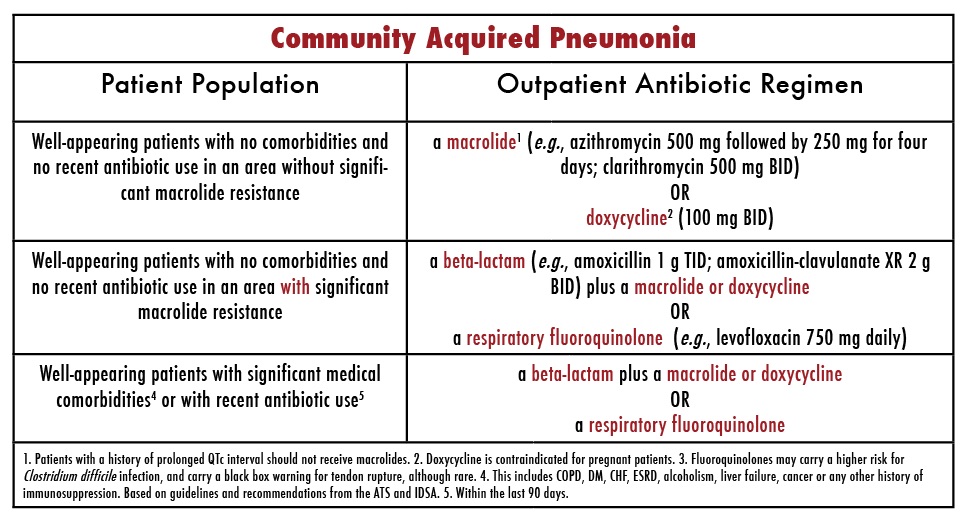
- Community Acquired Pneumonia. Doxycycline, dose: 200mg on the first day then 100mg per day. ...
- Hospital-Acquired Pneumonia. If pneumonia is hospital acquired, then following antibiotics are given as empirical therapy. ...
- Atypical pneumonia. If Chlammydophila species is suspected then give tetracycline.
- Aspiration pneumonia. ...
What are the most common causes of community acquired pneumonia?
Pneumonia is a common illness that affects millions of people each year in the United States. Germs called bacteria, viruses, and fungi may cause pneumonia. In adults, bacteria are the most common cause of pneumonia. Ways you can get pneumonia include: Bacteria and viruses living in your nose, sinuses, or mouth may spread to your lungs.
What is the first line treatment for pneumonia?
• Nonresolving pneumonia may be because of less common pathogens, or feature other conditions, and requires more detailed investigation. • Pediatric pneumonia is also common, and first-line treatment is still amoxicillin, followed closely by cephalosporins or macrolides.
What is the treatment for community acquired pneumonia?
Updated Clinical Practice Guidelines for Community-Acquired Pneumonia
- Etiology and Diagnosis. The most common bacterial causes of CAP are Streptococcus pneumoniae, Haemophilus influenzae, Mycoplasma pneumoniae, Staphylococcus aureus, Legionella species, Chlamydia pneumoniae, and Moraxella catarrhalis.
- Empirical Antibiotic Treatment. ...
- Directed Treatment. ...
- Duration of Therapy. ...
- The Pharmacist’s Role. ...
How effective is amoxicillin for pneumonia?
Your doctor will select the right antibiotic for you based on multiple factors, including: 6
- Your age: People 65 and older have a greater risk of serious complications from pneumonia infections.
- Your health history: A history of smoking, lung diseases, or other conditions may influence a person's ability to fight off infections.
- The exact infection you have: Your doctor may take a sample and test it for bacteria. ...
What is empiric treatment for community-acquired pneumonia?
Consensus guidelines from several organizations recommend empiric therapy with macrolides, fluoroquinolones, or doxycycline. Patients who are hospitalized should be switched from parenteral antibiotics to oral antibiotics after their symptoms improve, they are afebrile, and they are able to tolerate oral medications.
What antibiotic is preferred as empirical for treatment of community-acquired pneumonia in children?
For children aged <5 years, oral amoxicillin for a standard course of 5 days is the first-choice antibiotic. Macrolides are recommended if either M. pneumoniae or Chlamydia pneumoniae is suspected.
What antibiotic is primarily used for the treatment of bacterial community-acquired pneumonia?
The first-line treatment for pneumonia in adults is macrolide antibiotics, like azithromycin or erythromycin. In children, the first-line treatment for bacterial pneumonia is typically amoxicillin.
What is the treatment protocol for pneumonia?
TreatmentAntibiotics. These medicines are used to treat bacterial pneumonia. ... Cough medicine. This medicine may be used to calm your cough so that you can rest. ... Fever reducers/pain relievers. You may take these as needed for fever and discomfort.
What is empiric antibiotic therapy for pneumonia?
Consensus guidelines from several organizations recommend empiric therapy with macrolides, fluoroquinolones, or doxycycline. Patients who are hospitalized should be switched from parenteral antibiotics to oral antibiotics after their symptoms improve, they are afebrile, and they are able to tolerate oral medications.
When should antibiotics be initiated for the empiric treatment of CAP?
Timing of antibiotics — We generally start antibiotic therapy as soon as we are confident that CAP is the appropriate working diagnosis and, ideally, within four hours of presentation for patients being admitted to the general medical ward [28,29].
What is meant by empirical treatment?
Empiric therapy or empirical therapy is medical treatment or therapy based on experience and, more specifically, therapy begun on the basis of a clinical "educated guess" in the absence of complete or perfect information.
Which antibiotic is the means of choice in the empirical therapy of acquired communal pneumonia before the verification of the pathogen?
< 5 years: Amoxicillin or amoxicillin/clavulanate is usually the drug of choice. If epidemiology suggests an atypical pathogen as the cause and clinical findings are compatible, a macrolide (eg, azithromycin, clarithromycin) can be used instead.
What is the first line treatment for hospital acquired pneumonia?
In general, for both hospital-acquired pneumonia (HAP) and VAP, 7 days of treatment with appropriate antibiotics/antibiotics is recommended. This duration may be shortened or lengthened depending on the clinical response of the individual.
Which regimen is the preferred treatment for community-acquired pneumonia according to the 2019 IDSA guidelines?
a beta-lactam plus a respiratory fluoroquinolone (strong recommendation, low quality of evidence).
What is the most common treatment for pneumonia?
Mild pneumonia can usually be treated at home with rest, antibiotics (if it's likely be caused by a bacterial infection) and by drinking plenty of fluids. More severe cases may need hospital treatment.
What two antibiotics treat pneumonia?
Types of Antibiotics for Pneumonia Healthy adults under 65 years with pneumonia are typically treated with a combination of amoxicillin plus a macrolide like Zithromax (azithromycin) or sometimes a tetracycline like Vibramycin (doxycycline).
Which antibiotics are not associated with S pneumoniae?
Some antibiotics that have been used for the treatment of CAP have not been associated with widespread S pneumoniae penicillin resistance, including β-lactams, doxycycline, telithromycin, and respiratory quinolones ( eg, levofloxacin, gatifloxacin, or moxifloxacin). 26.
What antibiotics are used for CAP?
The first consideration in selecting an antibiotic for the treatment of CAP is the antibiotic spectrum. The antibiotic selected for CAP should have a high degree of activity against the usual typical pathogens responsible for CAP ( ie, Streptococcus pneumoniae, Haemophilus influenzae, or Moraxella catarrhalis and Legionella species, Mycoplasma pneumoniae, or Chlamydia pneumoniae among the nonzoonotic atypical pathogens). Pneumococci are the single most common bacterial pathogen causing CAP in hospitalized adults with CAP. H influenzae and M catarrhalis are more common in elderly patients with COPD. Aspirated oral pharyngeal anaerobes are the pathogens in aspiration CAP, which is most common in elderly patients who are in long-term care facilities or hospitals. Legionella is more common in elderly patients and compromised hosts with impaired cellular immunity. Legionella is relatively uncommon in young adults as a cause of ambulatory CAP. M pneumoniae and C pneumoniae along with respiratory viruses are the most common causes of CAP in ambulatory young adults. There are also important geographic differences. Legionella is apparently more common in the North American experience than in the European experience, and there are regional differences. Legionella is relatively common in some centers, and others have few or no cases, which should be taken into account in using or modifying CAP guidelines to reflect local patterns of pathogen distribution.
How long does CAP treatment last?
The single most important advance in the treatment of CAP has been in the area of pharmacokinetics. Traditionally, the duration of treatment for CAP has been 2 weeks. Treatment has been shortened in healthy individuals and has been extended in those with serious systemic disorders. Patients with severe CAP who are admitted to ICUs traditionally have been treated IV for the duration of their hospitalization. Also, hospitalized patients not requiring intensive care were treated entirely with 2 weeks of IV therapy. Siegel et al
What are antibiotic guidelines?
Antibiotic guidelines are supposed to emphasize commonality in therapeutic approach. While guidelines have common features, they vary in antibiotic choice, route of antibiotic administration, resistance potential, inclusion/exclusion of the pulmonary severity index, and antibiotic cost.
Is a quinolone good for CAP?
Respiratory quinolones are ideal agents for the treatment of CAP because they are highly active against penicillin-resistant strains of S pneumoniae, are active against all of the other common respiratory pathogens, are active against Legionella and the other atypical pulmonary pathogens, have a minimal resistance potential, have a good safety profile, and have the great advantage of favorable pharmacokinetic profiles, such that blood/lung levels are the same whether the drug is administered orally or IV in areas in which combination therapy offers no advantage and has several disadvantages, as explained.
Is comorbidity a therapeutic modifier?
Comorbidities are another cause of confusion. Comorbidities in some guidelines are a therapeutic modifier. Additional therapy is sometimes added to some guidelines. Severe systemic disorders have prognostic significance and can predict complications/ICU admission, but should have no effect on antibiotic selection. The following analogy emphasizes the point. Patients with asplenia with overwhelming, often fatal, S pneumoniae bacteremia are treated with penicillin or a β-lactam. Patients with intact B-cell immunity and non–life-threatening S pneumoniae bacteremia are treated the same way ( ie, with the same drug, dose, route of administration, and duration of therapy). Adding another drug because the patient has advanced lung, heart, liver, or renal disease makes little sense since the target of therapy is the pathogen, which is unaffected by morbidities. As with comorbidities, the severity of infection is not a reason to increase the spectrum morbidities or to add another antibiotic. Severity is primarily dependent on the underlying functional capacity of the lung, heart, and immune system. If the patient with severe CAP is treated initially with appropriate empiric monotherapy ( eg, a respiratory quinolone), what is the rationale for expanded coverage? In a patient with severe chronic bronchitis, pulmonary function may be so compromised by CAP that even a relatively avirulent pathogen ( eg, M catarrhalis) may present clinically as severe CAP requiring ICU admission. Coverage already includes penicillin-resistant S pneumoniae, all common bacterial pathogens, and Legionella. There is no reason for adding P aeruginosa coverage in non-cystic fibrosis/chronic bronchiectasis patients. Therapeutic choice is determined by the probable pathogen and should not be based on the severity of illness. Severity determines ICU admission and the initial mode of antibiotic administration, not the choice of antibiotics.
Is oral therapy good for CAP?
If IV-to-oral switch therapy was good, then oral therapy for hospitalized patients with moderate to moderately severe CAP is very good indeed. The pharmacoeconomic implications for oral therapy for non-critically ill hospitalized patients with CAP are important. This means that IV antibiotic therapy for CAP should be largely relegated to patients with severe CAP in the ICU setting. Oral therapy, which has traditionally been used for the treatment of mild-to-moderate CAP in the outpatient setting, can now be extended to include non-ICU patients hospitalized with moderate to moderately severe CAP. This principle will simplify the therapeutic approach ( ie, guidelines for CAP in ambulatory and hospitalized patients). At least, it will emphasize that the route of administration is less important than the spectrum and resistance potential of the antibiotic selected.
What is the FDA approved antimicrobial?
Since the publication of the 2007 IDSA/American Thoracic Society (ATS) guidelines for the management of CAP in adults, 2 intravenous antimicrobials have been approved by the US Food and Drug Administration (FDA) for the treatment of CAP: tigecycline and ceftaroline fosamil.
When was tigecycline approved?
Tigecycline was approved by the FDA in 2009 for adults with CAP caused by S pneumoniae (penicillin-susceptible isolates), including cases with concurrent bacteremia, H influenza (beta-lactamase-negative isolates), and Legionella pneumophila.
What is CAP in a hospital?
Empiric Therapy Regimens. Community-acquired pneumonia ( CAP) is one the most common infectious diseases addressed by clinicians. It is a major health problem in the United States and is an important cause of mortality and morbidity worldwide. It is the second most common reason for admission to the hospital and the most common infectious cause ...
What causes CAP in bronchiectasis?
Staphylococcalaureus may cause CAP in patients with influenza. Pseudomonas aeruginosa is a cause of CAP in patients with bronchiectasis or cystic fibrosis. [ 1] Atypical pathogen CAP manifests a variety of pulmonary and extrapulmonary findings (eg, CAP plus diarrhea).
How long does it take for a CAP to be diagnosed?
CAP is defined as pneumonia acquired outside a hospital or long-term care facility. It may be diagnosed within 48 hours of hospital admission. The designation "healthcare-associated pneumonia" (HCAP) is no longer included in the pneumonia guidelines. [ 1, 2, 3]
References
Bradley, JS, et al. The management of community-acquired pneumonia in infants and children older than 3 months of age: clinical practice guidelines by the Pediatric Infectious Diseases Society and the Infectious Diseases Society of America. Clin Infect Dis 2011;53:e25-e76.
Pediatric Empiric Antimicrobial Therapy Guidelines
This is a subsection of the UCSF Benioff Children’s Hospitals Empiric Antimicrobial Therapy Guidelines, developed by the Pediatric Antimicrobial Stewardship Programs at each campus to inform initial selection of empiric antimicrobial therapy for children at the UCSF Benioff Children’s Hospitals and affiliated outpatient sites.
