What is the CPT code for a nebulizer?
Code E0467 combines the function of a ventilator with all of the following: Oxygen equipment. Nebulizer and compressor.
Does CPT 94640 include medication?
CPT code 94640 describes treatment of acute airway obstruction with inhaled medication and/or the use of an inhalation treatment to induce sputum for diagnostic purposes.
Can CPT code 94664 and 94640 be billed together?
To bill both 94640 and 94664 on the same date of service, there must be documentation supporting that the procedures were separate and distinct from one another. The medical record should include a request for each procedure, and therapist documentation should support that procedures occurred at separate times.
What is the ICD 10 code for nebulizer treatment?
Long term (current) use of inhaled steroids Z79. 51 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM Z79. 51 became effective on October 1, 2021.
How do you bill for a nebulizer treatment?
If the treatment is less than 1 hour, you would bill Current Procedural Terminology (CPT) code 94640, “Pressurized or non-pressurized inhalation treatment for acute airway obstruction for therapeutic purposes and/or for diagnostic purposes such as sputum induction with an aerosol generator, nebulizer, metered dose ...Oct 2, 2017
What is included in CPT code 94010?
CPT code 94010, “Spirometry, including graphic record, total and timed vital capacity, expiratory flow rate measurement(s), with or without maximal voluntary ventilation,” may be separately reported when performed and documented with a six-minute walk test.
How do I bill for albuterol treatment?
The code for the nebulizer treatment is, "94640 Pressurized or nonpressurized inhalation treatment for acute airway obstruction for therapeutic purposes and/or for diagnostic purposes such as sputum induction with an aerosol generator, nebulizer, metered dose inhaler or intermittent positive pressure breathing (IPPB) ...Jun 12, 2018
What is included in CPT code 94375?
Group 1CodeDescription94375Respiratory flow volume loop94450Hypoxia response curve94617Exercise tst brncspsm w/ecg94618Pulmonary stress testing19 more rows
What does CPT code 96372 mean?
CPT® code 96372: Injection of drug/substance under skin or into muscle | American Medical Association.
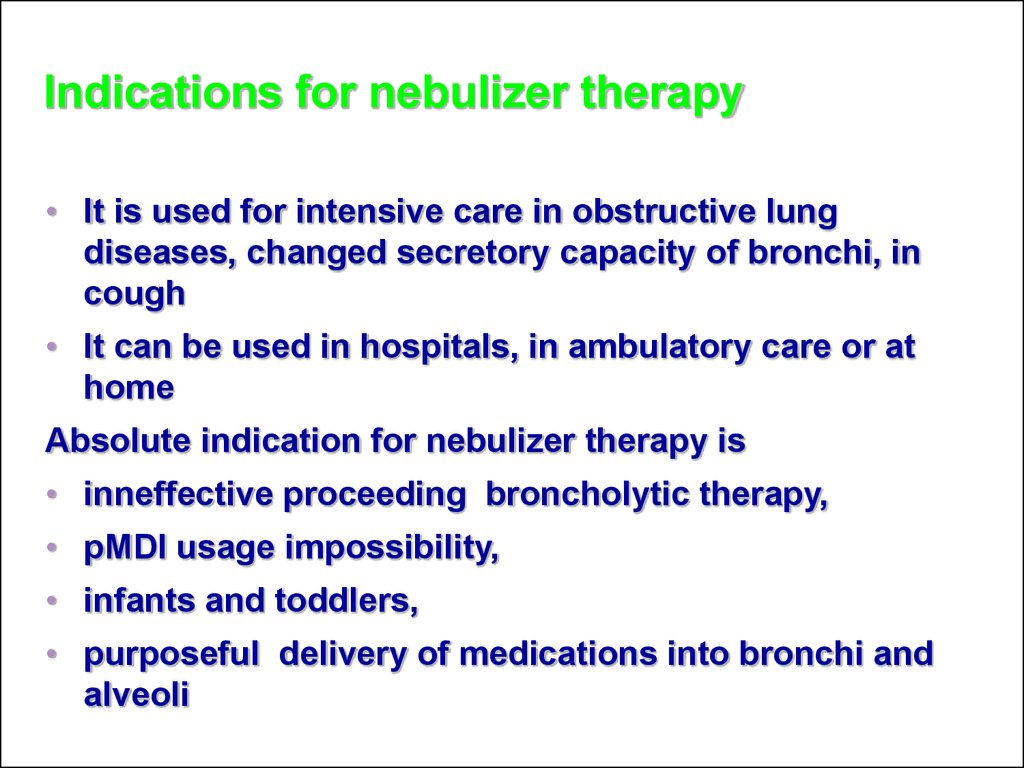
What diagnosis qualifies for a nebulizer?
To qualify for a nebulizer, you'll need a confirmed diagnosis to support a medical need for this device. You'll need to see a Medicare-approved provider and apply for the device within 6 months of an in-person visit. Some diagnoses that may be approved for coverage include COPD and cystic fibrosis.Aug 11, 2020
What diagnosis codes cover nebulizer?
A large volume nebulizer (A7007, A7017), related compressor (E0565 or E0572), and water or saline (A4217 or A7018) are covered when it is reasonable and necessary to deliver humidity to a patient with thick, tenacious secretions, who has cystic fibrosis (ICD-9 diagnosis code 277.02), bronchiectasis (ICD-9 diagnosis ...
What is CPT code A7003?
HCPCS code A7003 for Administration set, with small volume nonfiltered pneumatic nebulizer, disposable as maintained by CMS falls under Breathing Aids .
What is bronchodilator therapy?
Pharmacologic treatment with bronchodilators is used to prevent and/or control daily symptoms that may cause disability for persons with these diseases. These medications are intended to improve the movement of air into and from the lungs by relaxing and dilating the bronchial passageways.
What is CPT code 94640?
Time is a factor when billing the service. If the treatment is less than 1 hour, you would bill Current Procedural Terminology (CPT) code 94640, ‘Pressurized or non-pressurized inhalation treatment for acute airway obstruction for therapeutic purposes and/or for diagnostic purposes such as sputum induction with an aerosol generator, nebulizer, metered dose inhaler or intermittent positive pressure breathing (IPPB) device.’CMS policy states that an episode of care begins when a patient arrives at a facility for treatment and terminates when the patient leaves the facility. CPT code 94640 should be reported only once during an episode of care, regardless of the number of separate inhalation treatments that are administered. This means that if the patient requires two separate nebulizer treatments during the same visit, you would still only bill CPT code 94640 once.
Can a nebulizer be covered?
Nebulizers can be covered if the member’s ability to breathe is severely impaired. Lung diseases such as chronic obstructive pulmonary disease (COPD) and asthma are characterized by airflow limitation that may be partially or completely reversible. Pharmacologic treatment with bronchodilators is used to prevent and/or control daily symptoms ...
What does "appropriate" mean in medical terms?
Appropriate, including the duration and frequency that is considered appropriate for the service, in terms of whether it is: Furnished in accordance with accepted standards of medical practice for the diagnosis or treatment of the patient’s condition or to improve the function of a malformed body member.
Why do contractors specify bill types?
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service . Absence of a Bill Type does not guarantee that the policy does not apply to that Bill Type.
What are reasonable and necessary services?
Contractors shall consider a service to be reasonable and necessary if the contractor determines that the service is: 1 Safe and effective. 2 Not experimental or investigational (exception: routine costs of qualifying clinical trial services with dates of service on or after September 19, 2000, which meet the requirements of the clinical trials NCD are considered reasonable and necessary). 3 Appropriate, including the duration and frequency that is considered appropriate for the service, in terms of whether it is:#N#Furnished in accordance with accepted standards of medical practice for the diagnosis or treatment of the patient’s condition or to improve the function of a malformed body member.#N#Furnished in a setting appropriate to the patient’s medical needs and condition.#N#Ordered and furnished by qualified personnel.#N#One that meets, but does not exceed, the patient’s medical need.#N#At least as beneficial as an existing and available medically appropriate alternative.
What does "furnished" mean?
Furnished in a setting appropriate to the patient’s medical needs and condition. Ordered and furnished by qualified personnel. One that meets, but does not exceed, the patient’s medical need. At least as beneficial as an existing and available medically appropriate alternative.

CMS Need Nebulizer Necessity
Billing Scenarios and Correct Cpt Codes
- Time is a factor when billing the service. If the treatment is less than 1 hour, you would bill Current Procedural Terminology (CPT) code 94640, ‘Pressurized or non-pressurized inhalation treatment...
- However, if a patient receives ‘back-to-back’ nebulizer treatments exceeding 1 hour, (which rarely occurs in urgent care), bill CPT code 94644, ‘Continuous inhalation treatment with aero…
- Time is a factor when billing the service. If the treatment is less than 1 hour, you would bill Current Procedural Terminology (CPT) code 94640, ‘Pressurized or non-pressurized inhalation treatment...
- However, if a patient receives ‘back-to-back’ nebulizer treatments exceeding 1 hour, (which rarely occurs in urgent care), bill CPT code 94644, ‘Continuous inhalation treatment with aerosol medicat...
- If the patient receives a nebulizer treatment of less than 1 hour (CPT code 94640) during an episode of care and subsequently returns on the same date of service to the urgent care to receive anoth...
- The medications administered in the urgent care setting are most commonly a form of albut…
Documentations
- Appropriate documentation for Nebulizers must include the following items:
1. A recent order by the treating physician for refills, 2. A recent change in prescription, and 3. Beneficiary’s medical record within 12 months of the date of service showing usage of the item - When a shipping service makes a delivery, the following documentation elements must be prese…
1. Beneficiary’s name 2. Delivery address 3. Delivery service’s package identification number, supplier invoice number, or alternative method that links the supplier’s delivery documents with the delivery service’s records 4. A description of the items being delivered. The description can b…
Credentialing Services
- Simplifying Every Step of Credentialing Process, Most trusted and assured Credentialing servicesfor all you need, like Physician Credentialing Services, Group Credentialing Services, Re-Credentialing Services, Additionally We do provide: 1. General Surgery PracticeCredentialing 2. ChiropracticCredentialing Services 3. Credentialing for Optometry Practice 4. Credentialing for …