Mental Health Treatment CPT Codes & Unit Calculations CPT CODE DESCRIPTION DURATION 90791 Intake— Psychiatric diagnostic interview examination 1 to 2 units/hours 90792 Intake— Psychiatric diagnostic interview examination with med management 1 to 2 units/hours 90832
What are the billing codes for mental health?
Therapists say their professional codes of ethics already require disclosure to patients of per-visit costs.
What is the CPT code for Cognitive Therapy?
- Examine the patient with a focus on observing cognition
- Record and review the patient’s history, reports, and records
- Conduct a functional assessment of Basic and Instrumental Activities of Daily Living, including decision-making capacity
What is CPT code 96152?
96152 - CPT® Code in category: Health and behavior intervention – Deleted Codes. CPT Code information is available to subscribers and includes the CPT code number, short description, long description, guidelines and more. CPT code information is copyright by the AMA. Access to this feature is available in the following products:
What is the CPT code for OT treatment?
Content Menu
- Video Resources on YouTube
- Coding Overview
- CPT® Evaluation Codes
- Re-Evaluation
- ICD-10 Resources
- Diagnosis Code Selection
- CPT Coding Resources (Procedure Coding)
- Interventions
- Orthotics
- HCPCS Level II Coding (Coding for Orthotics, Prosthetics and Durable Medical Equipment)

What is a CPT code for mental health?
Common Behavioral Health Case Management CPT Codes 90832: 30 minutes of psychotherapy. 90834: 45 minutes of psychotherapy. 90837: 60 minutes of psychotherapy.
What is the difference between 90837 and 90838?
For 38 to 52 minutes of psychotherapy, you would use the 45-minute code, either 90834 or 90836; and for 53 minutes and beyond, you would use 90837 or 90838, the 60-minute codes.
What does CPT code 90833 mean?
Individual psychotherapy+90833 - Use add-on code for Individual psychotherapy, insight oriented, behavior modifying and/or supportive, 30 minutes with the patient and/or family member (time range 16-37 minutes), when performed with an evaluation and management service.
Who can use CPT code 90863?
The code 90863 was created to be used by providers who cannot report E/M services (such as psychologists or social workers). It is to be used to report pharmacologic management when it is provided with psychotherapy.
What is the difference between 90837 and 90847?
90847 involves family group therapy whereas 90837 is an individual session. The time frame is also different. 90837 sessions must be at least 53 minutes, and 90847 must be at least 26 minutes.
Can 99214 and 90837 be billed together?
The claim will be denied if box 24J or box 31 are filled out incorrectly. Medication management (evaluation and management) and psychotherapy Do not bill CPT codes 99201-99215 and 90832 or 90834 or 90837. It is acceptable to bill CPT codes 99201-99215 and 90833 or 90836 or 90838.
What is CPT code 90837 used for?
PsychotherapyCPT® code 90837: Psychotherapy, 1 | American Medical Association.
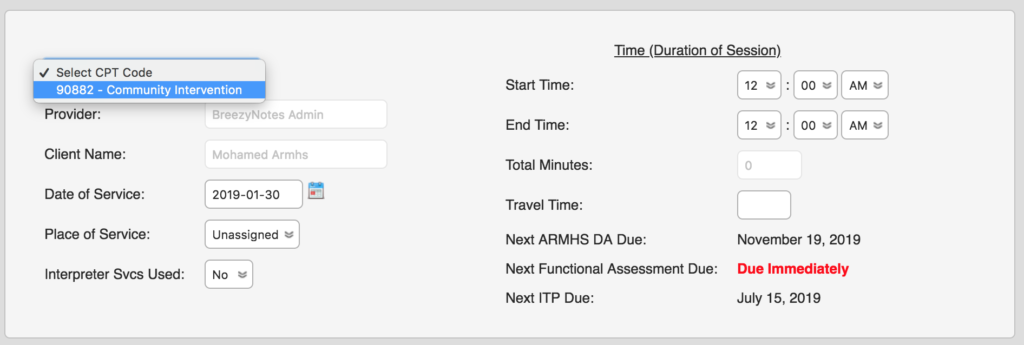
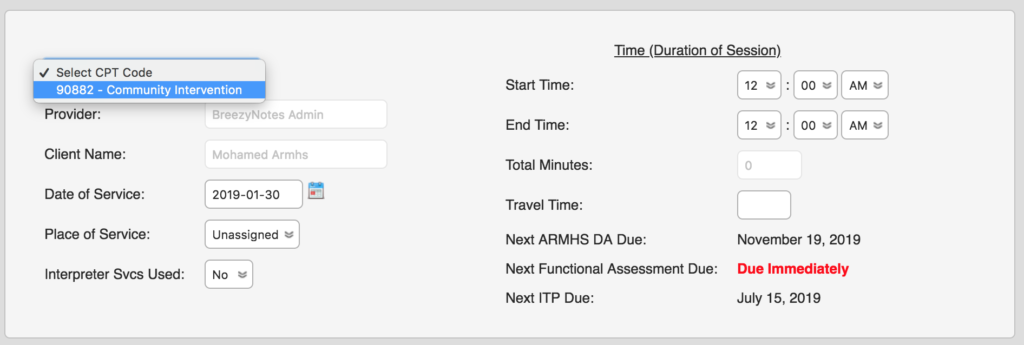
What does CPT code 90882 mean?
CPT® Code 90882 - Other Psychiatric Services or Procedures - Codify by AAPC.
What does CPT code 90899 mean?
Other Psychiatric Services or ProceduresCPT® Code 90899 - Other Psychiatric Services or Procedures - Codify by AAPC.
What are the new CPT codes for mental health 2021?
There are many CPT codes currently used by mental health professional that can be reported under the following categories:Health Behavior Assessment and Intervention (CPT codes 96156-96171)Psychotherapy Codes (CPT codes 90832-90863)Psychological and Neuropsychological Testing Codes (CPT codes 96105-96146)
What is the CPT code for counseling?
Key facts for utilizing psychotherapy codesPsychotherapy CodesCPT® CodeDescriptor90832Psychotherapy, 30 minutes with patient90834Psychotherapy, 45 minutes with patient90837Psychotherapy, 60 minutes with patient5 more rows
What is CPT code 90791 used for?
integrated biopsychosocial assessmentAccording to the CPT manual, 90791 is an “integrated biopsychosocial assessment, including history, mental status, and recommendations.” The manual goes on to say that the evaluation may include “communication with family or other sources and review and ordering of diagnostic studies.”
What are CPT Codes?
CPT is a uniform coding system developed by the American Medical Association (AMA). The AMA first established this system in 1966 to standardize terminology and simplify record-keeping for physicians and staff. Since its development, CPT has undergone several changes. The most recent edition focuses on using CPT codes to report physician services.
What is the CPT code for psychotherapy?
For example, therapists commonly use psychotherapy CPT codes falling in the range of 90832 to 90853 under Medicine’s psychiatry section. Psychiatrists, primary care physicians and other authorized prescribers might use evaluation and management codes for providing general medical services.
Why are CPT codes important?
CPT codes are essential parts of practice management for clinicians and health care staff because they determine compensation and the practice’s overall success.
What is CPT billing?
Current procedural terminology (CPT) codes are essential components of the health insurance billing process. It’s critical to use the appropriate procedure codes to receive reimbursement for your services and avoid an audit. However, using the correct CPT codes for medical billing involves understanding a complex system. There are thousands of codes to choose from and many different guidelines to follow. Nevertheless, it is possible to use medical codes properly and receive maximum reimbursement rates for your services.
How long is a CPT session?
Though CPT codes describe specific times, such as 30, 45, and 60 minutes, therapists have some flexibility, since sessions might go over or under that exact amount.
How many digits are in a CPT code?
The six sections of the CPT codebook are Evaluation and Management, Medicine, Surgery, Radiology, Anesthesiology and Pathology, and Laboratory. Each has a unique set of guidelines. The CPT codes under Category I are five digits long.
How to receive reimbursement for CPT?
To receive reimbursement, a clinician must complete accurate coding. Coding errors can lead to payment delays or rejected claims. Frequent or consistent errors could lead to an audit or charges of fraud. Strive for the highest accuracy, and cut down on simple errors like incorrect patient information or policy number mistakes. Always refer to the AMA’s most recent CPT manual to make sure you use the right codes in your practice.
What Are Add-ons, or Categories, of CPT Codes?
Add-on codes are codes that are always billed along with another code, called a primary code. The Centers for Medicare and Medicaid Services breaks these add-on codes into three categories:
What is the CPT type 3 code?
Type III codes are those for which a practitioner may bill along with an approved code listed in the CPT manual or if the provider offers medical justification for billing the add-on with another primary code. A common mental health add-on code is 90785, which denotes interactive complexity services.
What are add on codes?
Add-on codes are codes that are always billed along with another code, called a primary code. The Centers for Medicare and Medicaid Services breaks these add-on codes into three categories: 1 Type I codes are eligible for reimbursement only if submitted with an appropriate primary code for the same practitioner and client for services rendered on the same date. The only exception to this rule is if a client receives care from two practitioners in the same specialty, in the same practice, and on the same date. 2 Type II codes are not associated with a specific list of primary codes. Instead, these codes are eligible for reimbursement if a practitioner bills an acceptable primary code along with the add-on code for the same day of service. 3 Type III codes are those for which a practitioner may bill along with an approved code listed in the CPT manual or if the provider offers medical justification for billing the add-on with another primary code.
What is duplicate billing?
Duplicate billing, such as billing the same code twice or billing different codes for a single service. A basic familiarity with common billing codes can make it easier to quickly generate bills. Many psychotherapists only bill a few CPT codes.
How does the location of a service affect the reimbursement rate?
The location where you provide a service may affect the code you use. Facility-based reimbursement rates are lower than non-facility reimbursement rates , so using the right code may affect the amount of money you make.
What is the code for crisis psychotherapy?
Use 90839 for a 60-minute session. The actual time spent on treatment must be 30 to 74 minutes. Bill code 90840 for each additional 30 minutes beyond the initial 74 minutes.
When was CPT code developed?
The American Medical Association (AMA) developed the Current Procedural Terminology (CPT) code system in 1966. CPT codes standardize medical billing across disciplines and practice types, allowing a wide range of health care professionals, including mental health workers, to be reimbursed for their services.
What Are CPT Codes?
Current Procedural Terminology codes are used when billing a client’s insurance company in order to describe the treatment and assessment offered to the patient. The codes allow the mental health practitioner to be reimbursed for the care that they provided.
Why are CPT Codes Important?
Ultimately, if you want to get reimbursed fairly, then knowing how to correctly use CPT codes is paramount.
2020 Changes to CPT Billing Codes for Mental Health
Fortunately, there are only five changes that impact mental health. In one case, a single code replaced two existing codes, while in other cases, two codes replaced a single existing code. Most of the changes happened to the codes describing intervention services.
Impact of the Changes
Why were these changes made? A major change is that assessment services are no longer time-based. This frees providers to treat these services as they would other event-based services. Additionally, the new assessment code makes it possible to accommodate digitally-based services since the face-to-face requirement was eliminated.
90791: Psychiatric Diagnostic Evaluation (Initial Assessment)
A psychiatric diagnostic evaluation is an integrated biopsychosocial assessment, including client history, mental status, and treatment recommendations. It may include communication with family or other sources and review, and ordering of diagnostic studies.
90847: Family or Couples Therapy with the Patient Present
Used for face-to-face or telehealth couples and family psychotherapy sessions of 26 minutes or longer.
Common Add-On Codes
Add-on codes are CPT Codes that are listed separately for services that are performed in conjunction with a Primary Service. Add-on codes are only eligible for payment if it accompanies the appropriate Primary Service. If the Primary Service is denied for whatever reason, the add-on code will also be denied.