Other Treatments
- Transpupillary Thermotherapy – The temperature of the tumor is slowly raised, killing cancer cells and shrinking the tumor. ...
- Cryotherapy – The temperature of the tumor is lowered since melanocytes are susceptible to freezing. ...
- Gamma Knife – A focused, single dose of radiation is given to the tumor, sparing healthy tissue in and around the eye.
Full Answer
How are ocular metastases treated?
Treatment for ocular metastases requires a tight alliance between ocular and general oncologists. If a metastasis is the first indication of a systemic cancer—as it often is with lung cancer—the ocular oncologist may refer the patient to a general oncologist and advise the clinician about the type of tumor to look for.
What is the prognosis of ocular metastasis?
In general, prognosis is poor after an ocular tumor has metastasized. Without treatment, the median survival time is 2 to 8 months. We encourage you, though, to think of this as one data point, however. Many OM patients, even those with metastatic disease, have gone to live long, active lives.
When should you see an ophthalmologist for ocular metastases?
Detection of a suspected ocular metastasis should prompt an immediate referral to an ocular oncologist or, if that individual is not available, to a retinal specialist. “The referring ophthalmologist doesn’t even have to be right about the diagnosis,” Dr. Murray said. “If they even think it’s a cancer, we’ll see the patient right away.
What are the signs and symptoms of ocular metastases?
Not all ocular metastases fit the classic presentation of a creamy yellow mass deep to the retina. Less common presentations include a serous, nonrhegmatogenous retinal detachment with no apparent mass (flat metastasis), a swollen optic disc (optic nerve metastasis) or a hypopyon to the anterior chamber.

What is the life expectancy of someone with metastatic ocular melanoma?
The 5-year survival rate for eye melanoma is 82%. When melanoma does not spread outside the eye, the 5-year relative survival rate is about 85%. The 5-year survival rate for those with disease that has spread to surrounding tissues or organs and/or the regional lymph nodes is 71%.
Is ocular cancer treatable?
Eye cancer is most treatable when it is discovered early, says Renelle Lim, MD, a Yale Medicine ophthalmologist and specialist in ocular oncology and plastic surgery. “For that reason, we always advise everyone to have a dilated eye exam once a year with an eye doctor,” she says.
What is the best treatment for ocular melanoma?
Surgery. Surgery is the most common treatment for intraocular melanoma. The following types of surgery may be used: Resection: Surgery to remove the tumor and a small amount of healthy tissue around it.
What happens when ocular melanoma spreads to the liver?
Uveal melanoma, the most common primary intraocular tumor,1–4 has an associated approximate 40% risk of metastasizing to the liver within 10 years of diagnosis of the primary tumor. Hepatic metastases, which occur in 95% of patients with metastatic uveal melanoma,5 result in death in almost all cases.
Do you need chemo for eye cancer?
Doctors may treat some cancers on the surface of the eye (conjunctiva), such as melanoma and squamous cell cancer, with chemotherapy eye drops. This is called topical chemotherapy. Side effects include redness, a watery eye and inflammation.
Can eye cancer spread to the brain?
In addition to damaging vision, eye tumors can spread to the optic nerve, the brain and the rest of the body. Therefore, early diagnosis and treatment are extremely important.
Is ocular melanoma treatable?
These rare cancers can be treated with either surgical removal of the tumor, if it is small enough, or radiation therapy. In more advanced cases or if there is serious eye damage, enucleation (removal of the eyeball) may be needed.
How do you know if ocular melanoma has spread?
After intraocular melanoma has been diagnosed, tests are done to find out if cancer cells have spread to other parts of the body. The process used to find out if cancer has spread to other parts of the body is called staging. The information gathered from the staging process determines the stage of the disease.
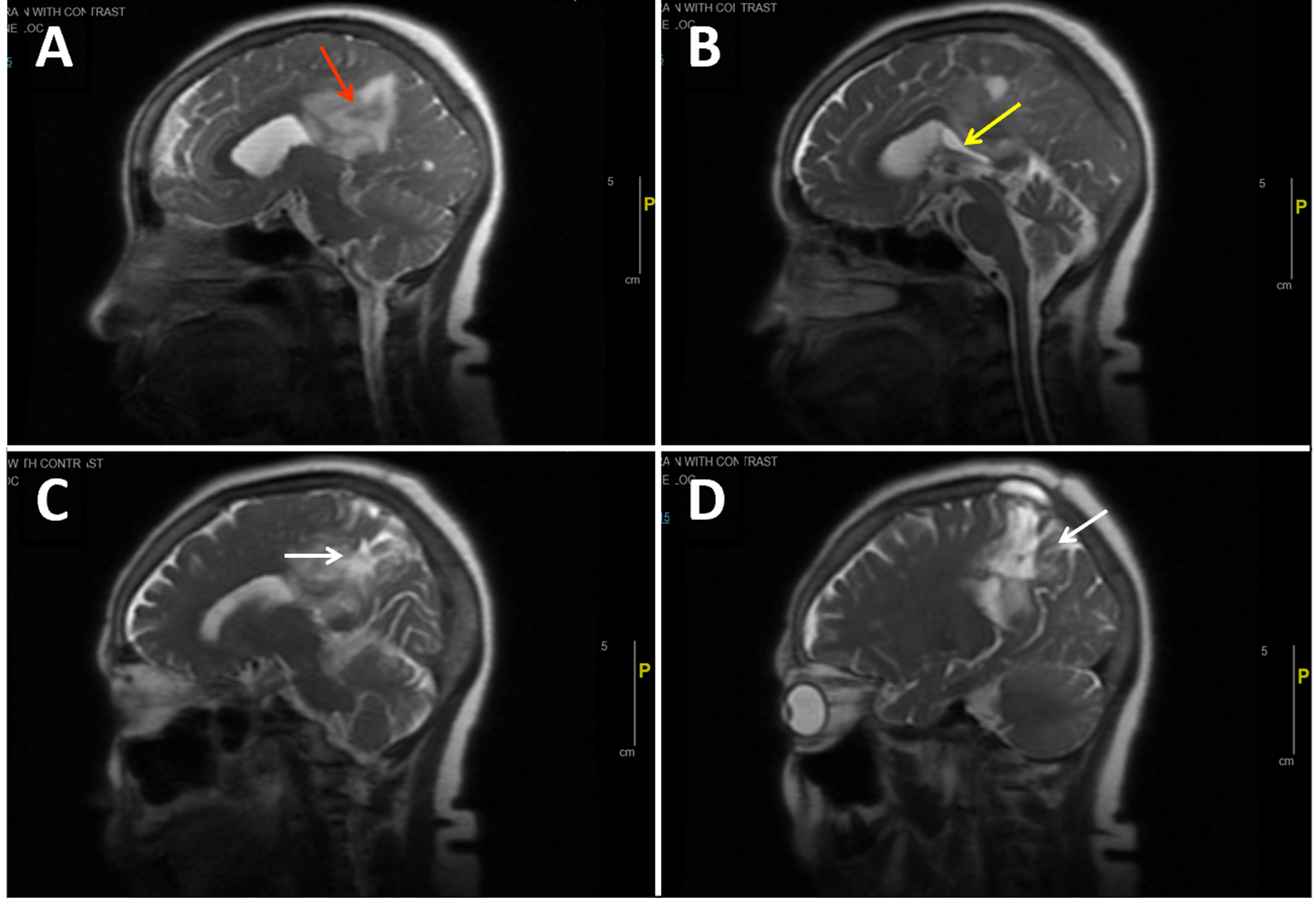
Can ocular melanoma spread brain?
Metastasis of the ocular malignant melanoma to the brain is extremely rare and most often occurs simultaneously with liver metastases. Lorigan et al., in clinical and radiological studies, found a total of five cases of brain metastases in 110 cases of metastatic choroidal melanoma [3].
What is Stage 4 ocular melanoma?
Stage 4. The cancer has spread to nearby lymph nodes or to other parts of the body (called distant metastasis), such as to the lungs, liver or bone. Cancer that has spread to a distant part of the body is also called metastatic eye cancer.
Where does ocular melanoma metastasize to?
An ocular melanoma has the potential to spread (metastasize) to other areas of the body. The liver is the most common organ in the body affected by metastasis of an ocular melanoma (80% of cases) but less often may involve the lungs, skin or soft tissue, and bone.
Can ocular melanoma spread to kidney?
Metastatic tumors are the most common malignancies of the kidney. We report a rare case of isolated metastatic ocular melanoma to the kidney occurring 20 years after diagnosis.
What is yttrium 90 used for?
RADIOEMBOLIZATION (administration of Yttrium-90 radioactive microspheres) is also being investigated in the treatment of uveal melanoma metastases to the liver. Tiny beads with an embedded radioactive material are injected directly into the arteries supplying the liver to kill the tumors. We are initiating a clinical trial to further study the effectiveness of this procedure for these tumors.
What is the most common malignant tumor in the eye?
Jefferson is a nationwide referral center for patients with uveal melanoma, the most common malignant tumor originating in the eye. At the time of diagnosis, more than 95% of patients have tumors limited to the eye, but at least 30% of these patients will subsequently develop metastases to other parts of the body, most commonly the liver and often several years after the diagnosis of the primary tumor. The clinical course of patients with uveal melanoma is generally determined by progression of the disease in the liver. Historically, median survival of patients with metastatic uveal melanoma to the liver has been up to 5 months. There are currently no effective systemic chemotherapy regimens for treatment of liver metastases from this tumor.
How long does a melanoma patient live?
Historically, median survival of patients with metastatic uveal melanoma to the liver has been up to 5 months. There are currently no effective systemic chemotherapy regimens for treatment of liver metastases from this tumor.
What is the treatment for cytokine in the liver?
Embolization involves blocking off the blood supply to the tumors by injecting an oily liquid (Ethiodol) and a temporary dissolvable agent (Gelfoam) into the arteries supplying the liver which helps to kill the tumors.
What is chemo injected into the liver?
CHEMOEMBOLIZATION is performed for patients with more extensive tumor involvement in the liver. BCNU (a chemotherapy drug) dissolved in an oily liquid (Ethiodol) is injected directly into the arteries supplying the liver, along with a temporary dissolvable agent (Gelfoam) to block off the blood supply to the tumors.
Does local stimulation of the immune system cause tumors?
This also presents tumor antigens to the immune system. Local stimulation of the immune system may result in development of a systemic immune response against tumor cells which could suppress the growth of additional tumors outside of the liver.
Why is fluorescein angiogram important?
A fluorescein angiogram also is useful because metastases tend to be hypofluorescent in the early angiogram and later show diffuse patchy fluorescence with multifocal leaks in the RPE. It’s those leaks that lead to retinal detachment.”.
What kind of oncologist treats ocular metastases?
Treatment for ocular metastases requires a tight alliance between ocular and general oncologists. If a metastasis is the first indication of a systemic cancer—as it often is with lung cancer—the ocular oncologist may refer the patient to a general oncologist and advise the clinician about the type of tumor to look for. For patients with previously treated cancers, the ocular oncologist may begin the restaging process and, if necessary, treat the ocular metastasis while referring the patient back to the general oncologist.
What to do if you suspect ocular metastasis?
Referral. Detection of a suspected ocular metastasis should prompt an immediate referral to an ocular oncologist or, if that individual is not available, to a retinal specialist. “The referring ophthalmologist doesn’t even have to be right about the diagnosis,” Dr. Murray said. “If they even think it’s a cancer, we’ll see the patient right away. We never say no to a patient.”
Why is ocular ultrasound important for metastases?
Dr. Shields agreed. “Ocular ultrasound is really important with metastases because they tend to be echogenic, whereas melanoma tends to be echolucent. A fluorescein angiogram also is useful because metastases tend to be hypofluorescent in the early angiogram and later show diffuse patchy fluorescence with multifocal leaks in the RPE. It’s those leaks that lead to retinal detachment.” Optical coherence tomography, she added, will help determine if subretinal fluid is present and is a good way to follow these lesions. Fine-needle aspiration biopsy is reserved for patients who have a negative preliminary workup and is necessary for only 1 to 2 percent of her patients.
What is the role of an ocular oncologist?
The ocular oncologist also may play a role in monitoring the patient’s systemic therapy. “General oncologists love to have us see their patients because the eye is one of the few sites where you can actually see a metastasis and watch it respond to therapy,” noted Dr. Shields. “If a patient has a choroidal metastasis, we measure it and document it with photography. The general oncologist then gives the chemotherapy or hormone therapy and sends the patient back to us two months later and say, 'How are we doing?'”
How thick is a breast metastasis?
According to Dr. Shields, breast cancer metastases tend not to be very thick, measuring about 2 to 3 millimeters, vs. an average thickness of 5.5 mm for melanoma. Metastases also tend to be yellow and very homogeneous in appearance, and the overlying retinal pigment epithelium is not as disturbed as it often is with a melanoma.
How many cases of eye cancer are there per year?
These are the most common ocular malignancies, with an estimated incidence of 30,000 cases per year (vs. about 2,500 cases of primary eye cancers). But many eye metastases go unrecognized.
How many cases of melanoma are there in MSK?
At MSK, we see more than 200 cases of benign eye lesions (choroidal nevi) each year and treat approximately 60 people with new eye melanomas (also called ocular melanoma) each year.
Where is the radiation placed in the eye?
In this type of radiation treatment, radioactive material is surgically placed on the outside wall of the eye, in the same spot that the tumor is on the inside of the eye. Our experts have decades of experience using brachytherapy for eye melanoma, and we treat many people with this approach.
Is MSK effective for a tumor?
Clinical trials sponsored by the National Institutes of Health, in which MSK played a leadership role, have proven that the removal of the eye and brachytherapy are equally effective for survival in people with medium-size tumors.
Who is David Abramson?
David Abramson cares for patients with melanoma of the eye; he’s also head of our ophthalmic oncology team, the only one of its kind in the United States .
Can you have an eye melanoma removed?
Depending on the size, location, and stage of the tumor, we may recommend that you have an operation to remove the eye. We often suggest this approach, called enucleation, if you have a relatively large eye melanoma. If the tumor is small, we may be able to treat it effectively with laser therapy.
Do you have to wear a mask at MSK?
Staff, patients, and visitors must continue to wear masks while at MSK, including people who are fully vaccinated. MSK is offering COVID-19 vaccines to all patients age 12 and over. To schedule or learn more, read this.
What is the best treatment for radiation blepharitis?
Radiation blepharitis (eyelid inflammation) can be treated with silvadine ointment, black tea soaks, or A&D ointment. If not already working with one, patients are strongly encouraged to consult with an oncologist to construct a proper surveillance schedule for ongoing observation and care.
What is the term for the removal of the eye?
Transretinal endoresection. Enucleation . Enucleation refers to full removal of the affected eye. After enucleation surgery, the patient is admitted to the hospital and the eye is removed under either local or general anesthesia. The enucleated eye cannot be treated or repaired and replaced in the eye socket.
How long after cataract surgery can you go home?
The patient usually leaves the hospital one or two days after surgery. In some cases, patients are permitted to go home the same day. Three to six weeks later, a specialist who makes artificial eyes (called an ocularist) fits the patient with a prosthesis.
What is a partial choroidectomy?
Transscleral partial choroidectomy (cyclochoroidectomy) – A viable therapeutic option for the subset of patients with choroidal or ciliochoroidal tumors who are poor candidates for radiotherapy but are highly motivated to avoid enucleation ( http://archopht.ama-assn.org/cgi/content/full/120/12/1659)
How long does it take for a plaque to be removed?
The plaque is left in place for a few days (6 days is not atypical) and then removed. Brachytherapy is commonly used to treat OM as well as localized prostate cancer, cervical cancer, and other cancers of the head and neck. Dr. Finger has a good overview of plaque therapy on his Eye Cancer Foundation site.
What is the most common form of radiation treatment?
Brachytherapy ("Plaque Therapy") Also known as sealed source radiotherapy or endocurietherapy, brachytherapy is the most common form of radiation treatment. With plaque therapy, a small disc-shaped shield known as a plaque encasing radioactive seeds (most often Iodine-125, though Ruthenium-106 and Palladium-103 can also be used) ...
Why is TTT used less frequently?
TTT is used less frequently in OM treatment due to issues with final control and recurrence.
Treatment Options
The liver is (initially) the exclusive site of choroidal melanoma metastasis in about 40% of patients. Of those patients, most have diffuse or multi-focal tumors which cannot be removed. Treatment options depend on the size, location and rate of tumor growth.
Observation
It is a patient’s right to choose or refuse treatment. Since many of the previously mentioned treatments can decrease a patient’s quality of life, each decision to treat must be weighed against potential side effects.
What is immunoembolization therapy?
Immunoembolization was developed at Jefferson as a novel therapy to improve survival in uveal (ocular) melanoma patients with liver metastases. This involves injecting cytokines (drugs which stimulate or modulate immune responses) directly into the arteries supplying the liver, combined with embolization of the hepatic artery.
What is the treatment for liver tumors?
Chemoembolization is performed in patients with more extensive tumor involvement in the liver. BCNU (a chemotherapy drug) dissolved in an oily liquid (Ethiodol) is injected directly into the arteries supplying the liver, along with a temporary dissolvable agent (Gelfoam) to block off the blood supply to the tumors.
How long does it take to recover from a liver metastasis?
This procedure improves survival for those with liver metastases from, at best, five months under conventional treatment to an average of 14.5 months. There are just a few other centers in the country that treat uveal (ocular) melanoma, and none through immunoembolization.
How many procedures are performed for metastatic melanoma?
We perform more than 350 procedures annually for patients with metastatic uveal (ocular) melanoma. The course of treatment for this disease is generally determined by progression of the disease in the liver. There are currently no effective systemic chemotherapy regimens for treatment of liver metastases from this tumor.
What is the best way to receive new treatments?
Clinical trials are the best way patients can receive new therapies and procedures. To find out if a clinical trial might be right for you, ask your health care provider or contact the Sidney Kimmel Cancer Center Clinical Research Management Office at 215-955-1661.
Is melanoma a low incidence?
The incidence of ocular, or uveal, melanoma is very low – about six cases per one million Americans – but the chances are good that patients with advanced stages of the disease will seek treatment at Jefferson. Jefferson has become a national referral center for patients whose uveal cancer has metastasized.
Abstract
AIMS Three issues were investigated in adult outpatients with orbital metastases. One, how accurate are current diagnostic methods? Two, what is the survival associated with orbital metastases? Three, did any clinical factors correlate with prognosis in this patient cohort?
Methods
We retrospectively reviewed the ocular oncology database at the University of California, San Francisco, for outpatients managed from 1976 to 1995 in whom the diagnosis of orbital metastases was established. Hospitalised patients with widespread disease, noted to have incidental orbital metastases, were excluded from this analysis.
Results
There were 15 males and 16 females, with a median age of 57 years (range 37 to 77 years). The racial distribution was five black, one Asian, and 25 white patients.
Discussion
Orbital metastases are relatively uncommon. In our experience 36 of 612 orbital biopsies for suspected neoplasm (6%) were metastatic in origin; this incidence is similar to that reported in other series.
Acknowledgments
This study was performed at the Department of Ophthalmology, University of California, San Francisco, USA. It was supported in part by That Man May See, San Francisco, California, USA.
Request Permissions
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.