
What you should know about thromboembolism?
Thromboembolism is the ungainly name given to the condition in which a blood clot that has formed inside a blood vessel (or inside the heart) subsequently breaks off, travels through the bloodstream, and plugs another blood vessel, causing organ damage. Science Photo Library - SCIEPRO / Getty Images.
How to treat thromboembolism?
Treatment
- Anticoagulants. Anticoagulants (commonly referred to as “blood thinners”) are the medications most commonly used to treat DVT or PE.
- Thrombolytics. Thrombolytics (commonly referred to as “clot busters”) work by dissolving the clot. ...
- Inferior vena cava filter. ...
How to prevent venous thromboembolism?
These include:
- Getting plenty of exercise: Lack of exercise is unhealthy for many reasons, and it is a major risk factor for DVT. ...
- Keep your weight where it should be: People who are overweight have an elevated risk for DVT, and maintaining a healthy weight can reduce your odds of having a DVT.
- Don’t smoke: Smoking can wreck your health in many ways. ...
Is thrombolytic therapy effective for pulmonary embolism?
Thrombolytic treatment accelerates the dissolution of thrombus in acute pulmonary thromboembolism (PTE) and is potentially a lifesaving treatment. High-risk PTE is the clearest indication for this therapy, and its use in intermediate-risk cases is still controversial.
How can thromboembolism be prevented?
Drink lots of fluids. Wear loose-fitting clothing. Walk and stretch at regular intervals (for example, when traveling by car, make frequent stops to allow you to get out and stretch your legs). Special stockings that compress the legs below the knee may help prevent blood clots from forming.
What techniques are the most effective in the prevention of venous thromboembolism?
Methods of DVT prophylaxis include general measures: the use of aspirin, mechanical prevention with graduated compression stockings, and intermittent pneumatic compression devices.
Is heparin VTE prophylaxis?
Pharmacologic prophylaxis is utilized in trauma patients to reduce their risk of a VTE event. The Eastern Association for the Surgery of Trauma guidelines recommend use of low-molecular-weight heparin (LMWH) as the preferred agent in these patients.
What drugs are used for VTE prophylaxis?
Apixaban, dabigatran, rivaroxaban, edoxaban, and betrixaban are alternatives to warfarin for prophylaxis or treatment of deep venous thrombosis (DVT) and pulmonary embolism (PE).
How do thrombolytics work?
Thrombolytics (commonly referred to as “clot busters”) work by dissolving the clot. They have a higher risk of causing bleeding compared to the anticoagulants, so they are reserved for severe cases.
What is the procedure to remove a clot in a patient with DVT?
In rare cases, a surgical procedure to remove the clot may be necessary. Thrombectomy involves removal of the clot in a patient with DVT. Embolectomy involves removal of the blockage in the lungs caused by the clot in a patient with PE.
What is a DVT test?
DVT. Duplex ultrasonography is an imaging test that uses sound waves to look at the flow of blood in the veins. It can detect blockages or blood clots in the deep veins. It is the standard imaging test to diagnose DVT. A D-dimer blood test measures a substance in the blood that is released when a clot breaks up.
What anticoagulants are used to prevent bleeding?
Fondaparinux (injected under the skin). Anticoagulants that are taken orally (swallowed) include. Warfarin, Dabigatran, Rivaroxaban, Apixaban, and. Edoxaban. All of the anticoagulants can cause bleeding, so people taking them have to be monitored to prevent unusual bleeding.
What is CTPA in pulmonary angiography?
Computed tomographic pulmonary angiography (CTPA) is a special type of X-ray test that includes injection of contrast material (dye) into a vein. This test can provide images of the blood vessels in the lungs. It is the standard imaging test to diagnose PE.
What are the symptoms of DVT?
There are other conditions with signs and symptoms similar to those of DVT and PE. For example, muscle injury, cellulitis (a bacterial skin infection), and inflammation (swelling) of veins that are just under the skin can mimic the signs and symptoms of DVT. It is important to know that heart attack and pneumonia can have signs ...
Do blood thinners thin blood?
Although called blood thinners, these medications do not actually thin the blood. They reduce the ability of the blood to clot, preventing the clot from becoming larger while the body slowly reabsorbs it, and reducing the risk of further clots developing. The most frequently used injectable anticoagulants are.
What is the broader term for venous thromboembolism?
The broader term venous thromboembolism generally refers to DVT, PE, or a combination of the two (DVT/PE). With that said, thromboembolism can involve other veins of the body, both deep and superficial. 2
Where does a thrombus travel?
That is, part of the thrombus that has formed in the leg veins breaks loose and travels through the venous system, through the right side of the heart, and into the pulmonary artery where it lodges, and cuts off blood flow to a portion of the lungs.
What is the term for a blood clot in the deep leg?
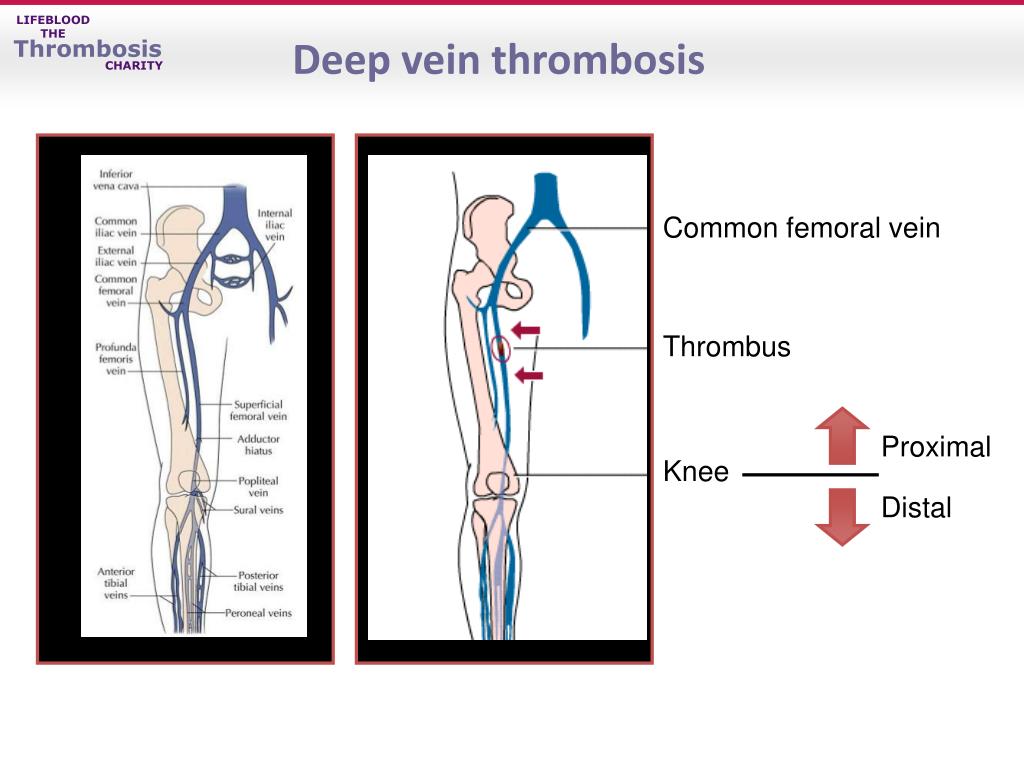
When doctors use the word thromboembolism, they are usually referring to the conditions deep venous thrombosis (DVT) and pulmonary embolus. The fact that these two conditions are so closely related accounts for the term “thromboembolism” being created in the first place. In DVT, blood clots develop in the deep leg veins.
What is the term for a blood clot that blocks blood flow?
Arterial thromboembolism occurs when a blood clot breaks off and blocks an artery, causing ischemia (the restrictions of blood flow and oxygen) and sometimes infarction (tissue death due to an inadequate blood supply). The majority of arterial embolisms involve a blood clot. 4
What is the term for a blood clot that forms in a blood vessel, breaks loose, and is?
Thromboembolism is a medical term used to describe a blood clot ( thrombus) that forms in a blood vessel, breaks loose, and is carried by the bloodstream to block another blood vessel. When an unattached mass of any sort (called an embolus) causes an obstruction, the blockage is referred to as an embolism. 1
What does DVT mean in medical terms?
Deep vein thrombosis (DVT): Throbbing, cramps, swelling, warmth, pain, hardened veins, and redness or darkened skin in one leg 5
What happens if a clot breaks off?
If the clot breaks off and lodges in a lung, it causes a serious condition known as pulmonary embolism (PE). 2 PE can be fatal depending on the location of the embolus and the degree of blood flow obstruction. 3
How to reduce the risk of VTE?
There are two major ways to reduce the risk of VTE. The first is to screen patients pre- and post-operatively with accurate diagnostic testing. By diagnosing VTE early, treatment could be provided to halt progression and avoid morbidity and mortality associated with acute VTE. Unfortunately, contrast venography is expensive, painful, and impractical to perform outside of clinical studies [ 26 ]. Less invasive studies, such as venous ultrasonography, are less sensitive in asymptomatic patients than in symptomatic patients [ 51, 52 ]. This is likely because most thrombi are small, non-occlusive calf vein thrombi, most of which may not extend and cause symptomatic DVT or PE and are of uncertain clinical significance. Screening “at-risk” patients is impractical and too expensive to be undertaken outside of clinical trials.
How to prevent VTE?
The second approach is to undertake measures to prevent VTE. General measures, such as encouraging early ambulation after surgery, can be adopted universally without harm. In addition, active prophylaxis with either mechanical or pharmacologic means has been proven to lower the risk of VTE. Mechanical prophylaxis refers to devices, such as graduated compression stockings and intermittent pneumatic compression devices, which decrease venous stasis in the lower extremities. Mechanical prophylaxis does not carry a risk of bleeding but can be uncomfortable, and prolonged use can lead to skin breakdown and other cutaneous complications. Recent American Society of Hematology (ASH) guidelines for prophylaxis in medical patients recommend mechanical prophylaxis when the bleeding risk is unacceptably high but suggest using pharmacologic prophylaxis in all patients without elevated risks for bleeding [ 9 ]. Given the relative paucity of evidence for mechanical prophylaxis, this review will focus on the use of pharmacologic prophylaxis. Low-dose anticoagulant medications reduce the risk of VTE by 50–80% across a variety of clinical circumstances at a cost of a modest increase in the risk of bleeding. Trials in VTE prevention attempt to identify large groups of patients who are at elevated risk, such as patients after hip surgeries, and administer low dose anticoagulants with the goal of reducing VTE.
What is the goal of pharmacologic VTE prophylaxis?
The primary goal of pharmacologic VTE prophylaxis is to prevent fatal PE , and in the intensive care unit (ICU) and surgical patients pharmacologic VTE prophylaxis is associated with a reduction in mortality [ 5, 6 ]. Early clinical studies in VTE prevention focused on the potential benefit of prophylactic anticoagulation in populations at high risk of VTE. This approach is easy to implement in patient care, and pharmacologic VTE prophylaxis for medical and surgical inpatients is frequently included in admission order sets for these patients. However, recent evidence suggests the risk of bleeding with anticoagulant thromboprophylaxis negated its benefit in some groups of patients [ 7, 8, 9 ]. Subsequent trials are examining whether it is possible to improve upon this approach by developing a risk prediction tool to identify individuals with high VTE risk who would benefit the most from thromboprophylaxis. In this review, we discuss how VTE epidemiology and the results of contemporary thromboprophylaxis trials have improved our understanding of risk factors and our ability to enhance the benefits of VTE prophylaxis. In particular, we will discuss modern thromboprophylaxis as it pertains to genetic risk factors, exogenous hormonal therapies, pregnancy, surgery, medical hospitalization, cancer, and what is known so far about VTE in COVID-19 infection.
What is VTE in medical terms?
Venous thromboembolism (VTE) is the third most common cause of vascular mortality worldwide and comprises deep-vein thrombosis (DVT) and pulmonary embolism (PE). In this review, we discuss how an understanding of VTE epidemiology and the results of thromboprophylaxis trials have shaped the current approach to VTE prevention. We will discuss modern thromboprophylaxis as it pertains to genetic risk factors, exogenous hormonal therapies, pregnancy, surgery, medical hospitalization, cancer, and what is known thus far about VTE in COVID-19 infection.
How are structured protocols used to predict VTE?
Over the past three decades, structured protocols have been developed and validated to reliably risk-stratify patients based upon clinical features and laboratory testing into risk groups for VTE. Protocols for estimating the VTE risk of individual patients admitted to hospital, after surgery, and outpatients with cancer are used in clinical practice today to aid in prescribing anticoagulant prophylaxis to those at greatest risk. By combining patient characteristics (e.g., personal history of VTE, BMI, genetic risk factors), context (e.g., hip arthroplasty, ambulatory pancreatic cancer, pregnancy), and predictive biomarkers (e.g., D-dimer) modern scoring systems aim to predict the risk of VTE in individual patients in an effort to target preventative measures to those who will benefit most.
What are the factors that determine the risk of VTE?
An individual patient’s risk of VTE depends on intrinsic, patient-specific factors (such as genetic risk factors, age, or body mass index) and acquired risk due to the unique context or situation (such as hospitalization, surgery, or cancer).
When does venous thrombosis occur in children?
Even in the presence of cancer, venous access devices, and medications that increase the risk of thrombosis, the incidence of venous thrombosis in children remains low until adulthood—late teens and early 20s.
What is the purpose of the review of thrombosis?
The purpose of this review is to provide an overview of the epidemiology of thrombosis in patients with cancer, to highlight evidence pertaining to its treatment and prevention in this population and to suggest how pharmacists may play a role in improving the care of patients with cancer and VTE.
What is the role of pharmacists in antithrombotic therapy?
Regardless of the selected antithrombotic therapy, pharmacists are in a position to educate patients about the risk of VTE, the risk of bleeding and directions for care if such an event occurs. They can also emphasize the importance of adherence with therapy. Pharmacists should also work with the patient and other caregivers to minimize the impact of drug interactions involving anticoagulant therapy.
What is the best treatment for cancer VTE?
Current clinical evidence and guidelines suggest that cancer patients receiving care in hospital with no contraindications should receive VTE prophylaxis with unfractionated heparin (UFH), a low-molecular-weight heparin (LMWH) or fondaparinux. Patients who require surgery for their cancer should receive prophylaxis with UFH, LMWH or fondaparinux. Cancer patients who have experienced a VTE event should receive prolonged anticoagulant therapy with LMWH (at least 3 months to 6 months). No routine prophylaxis is required for the majority of ambulatory patients with cancer who have not experienced a VTE event. Most publicly funded drug plans in Canada have developed criteria for funding of LMWH therapy for patients with cancer.
What should a pharmacist do for cancer patients?
Pharmacists should ensure that the therapeutic approach to anticoagulant therapy for cancer patients is evidence-based and consistent with the literature, published guidelines and patient preferences. As well, pharmacists should be vigilant in reviewing the patient's medication profile for agents such as hormone replacement therapy, oral contraceptives, tamoxifen, thalidomide, bevacizumab and erythropoietin-stimulating agents to ensure that consideration is given to prevention and treatment of thrombosis risk that may be increased by these agents. The authors of the Oncology Workforce Study in the United States recommended that oncology pharmacists can play an important role in preventing and managing thrombosis.33Given the impact that pharmacists have had in a wide variety of other disease states, it is only logical that they work to ensure optimal care of cancer patients who have experienced or are at risk of experiencing VTE. Through discussions with patients, pharmacists can better understand the options that have been offered and the choices that have already been made. For example, if the patient has active VTE and is being treated with warfarin, the pharmacist can determine if LMWH has been offered and, if not, can collaborate with the patient and the physician to determine if this might be a preferable treatment strategy, given currently available evidence and the limitations and challenges associated with warfarin anticoagulation. If warfarin is the preferred strategy, the pharmacist should work with the patient and the physician to optimize warfarin control. Bungard et al. recently published a practice tool and practical management tips that pharmacists may find helpful in ensuring best outcomes with warfarin therapy.34The Anticoagulation Forum has suggested that patients who are taking warfarin must receive information about the common signs and symptoms of thrombosis and bleeding and what to do if they occur. The common signs of thrombosis include shortness of breath and painful, swollen calves. Bleeding events that are commonly associated with anticoagulant therapy include bruising, minor bleeding, nosebleeds and more significant bleeding events, which may manifest as black stools, blood in the stool, rectal bleeding and vomiting of material with the appearance of coffee grounds. Patients should be advised that if any of these events occur (other than bruising, minor nosebleeds and other types of minor bleeding), they should seek medical attention.35
What is VTE in cancer?
Venous thromboembolism (VTE), including deep vein thrombosis (DVT) and pulmonary embolism, is a common complication of cancer and its treatment and occurs more frequently in patients with cancer than in patients without it. Patients with cancer have an annualized risk of VTE 6 to 12 times higher than those without cancer.1Among patients with cancer, VTE is strongly associated with reduced survival,2and thromboembolism is the second leading cause of death among outpatients who are receiving cancer therapy.1 Clinical trial data have demonstrated that anticoagulation therapy for prevention or treatment of VTE in patients with cancer, especially low-molecular-weight heparins (LMWHs), prevents morbidity and may decrease mortality.3However, despite evidence demonstrating the efficacy of anticoagulant therapy, VTE often goes unrecognized and may be treated suboptimally. Pharmacists are well positioned to aid in enhancing the management of cancer patients who have or are at risk of VTE.
How often do cancer patients get VTE?
The frequency of VTE in cancer patients being treated in hospital ranges from 0.6% to 5.4%.9Among medical inpatients with cancer, rates of VTE are lower with prophylaxis using LMWH, rather than unfractionated heparin (UFH) or placebo, without significantly higher rates of major bleeding.10Three large randomized controlled trials demonstrated the efficacy of enoxaparin, dalteparin and fondaparinux, respectively, in preventing VTE in medical patients being treated in hospital (Table 1).11–13In each of these trials, data were reported for nonrandomized cancer subgroups. Although these trials provided information about the efficacy of intervention, they had several limitations, including the limited number of cancer patients (5% to 15% of the patients in each trial) and the fact that bleeding events were not reported for the cancer subgroups.
Is prophylaxis warranted for multiple myeloma?
Preliminary data from randomized controlled trials involving ambulatory patients with cancer are conflicting. This, in combination with the known risk of bleeding in patients with cancer, suggests that prophylaxis is likely not warranted in the majority of ambulatory cancer patients given the benefit to risk ratio. Conversely, thromboprophylaxis with a fixed, low dose of warfarin (1–2 mg/day) or a LMWH may be warranted for patients with multiple myeloma who are receiving thalidomide-or lenalidomide-based combination therapy.17Further data are required for this population.
What is a deep vein thromboembolism?
Deep vein thrombosis (DVT) is a medical condition that occurs when a blood clot forms in a deep vein.
Why is it important to know about DVT?
It is important to know about DVT because it can happen to anybody and can cause serious illness, disability, and in some cases, death. The good news is that DVT is preventable and treatable if discovered early.
What is a VTE?
Venous thromboembolism (VTE), a term referring to blood clots in the veins, is an underdiagnosed and serious, yet preventable medical condition that can cause disability and death. The American Society of Hematology. external icon.
What happens if you have a DVT?
In addition, one-third to one-half of people who have a DVT will have long-term complications caused by the damage the clot does to the valves in the vein called post-thrombotic syndrome (PTS). People with PTS have symptoms such as swelling, pain, discoloration, and in severe cases, scaling or ulcers in the affected part of the body. In some cases, the symptoms can be so severe that a person becomes disabled.
How many people with DVT have no symptoms?
About half of people with DVT have no symptoms at all. The following are the most common symptoms of DVT that occur in the affected part of the body:
What is the most serious complication of DVT?
Complications of DVT. The most serious complication of DVT happens when a part of the clot breaks off and travels through the bloodstream to the lungs, causing a blockage called pulmonary embolism ( PE). If the clot is small, and with appropriate treatment, people can recover from PE.
What causes slow blood flow?
Major surgery (particularly involving the abdomen, pelvis, hip, or legs). Slow blood flow, often caused by: Confinement to bed. (e.g., due to a medical condition or after surgery); Limited movement (e.g., a cast on a leg to help heal an injured bone); Sitting for a long time, especially with crossed legs; or.
How to treat DVT?
DVT is most commonly treated with anticoagulants, also called blood thinners. These drugs don't break up existing blood clots, but they can prevent clots from getting bigger and reduce your risk of developing more clots. Blood thinners may be taken by mouth or given by IV or an injection under the skin.
What blood thinners are used for DVT?
The most commonly used injectable blood thinners for DVT are enoxaparin (Lovenox) and fondaparinux (Arixtra). After taking an injectable blood thinner for a few days, your doctor may switch you to a pill. Examples of blood thinners that you swallow include warfarin (Jantoven) and dabigatran (Pradaxa).
What is a clot buster?
Clot busters. Also called thrombolytics, these drugs might be prescribed if you have a more serious type of DVT or PE, or if other medications aren't working.
What blood test is used to diagnose a blood clot?
Tests used to diagnose or rule out a blood clot include: D-dimer blood test. D dimer is a type of protein produced by blood clots. Almost all people with severe DVT have increased blood levels of D dimer. A normal result on a D-dimer test often can help rule out PE. Duplex ultrasound.
How many goals are there for DVT?
There are three main goals to DVT treatment.
What to do if you can't take medicine to thin your blood?
If you can't take medicines to thin your blood, you might have a filter inserted into a large vein — the vena cava — in your abdomen. A vena cava filter prevents clots that break loose from lodging in your lungs. Compression stockings. These special knee socks reduce the chances that your blood will pool and clot.
How to prevent blood clots in knees?
Compression stockings. These special knee socks reduce the chances that your blood will pool and clot. To help prevent swelling associated with deep vein thrombosis, wear them on your legs from your feet to about the level of your knees. You should wear these stockings during the day for at least two years, if possible.
What is the treatment for pulmonary embolism?
Treatment of pulmonary embolism is aimed at keeping the blood clot from getting bigger and preventing new clots from forming. Prompt treatment is essential to prevent serious complications or death.
Where to get pulmonary embolism evaluated?
Preparing for your appointment. Pulmonary embolism is often initially evaluated in hospitals, emergency rooms or urgent care centers. If you think you might have a pulmonary embolism, seek immediate medical attention.
What is a blood clot tracer?
The tracer maps blood flow (perfusion) and compares it with the airflow to your lungs (ventilation) and can be used to determine whether blood clots are causing symptoms of pulmonary hypertension.
How accurate is a pulmonary embolism test?
This test provides a clear picture of the blood flow in the arteries of your lungs. It's the most accurate way to diagnose pulmonary embolism, but because it requires a high degree of skill to administer and has potentially serious risks, it's usually performed when other tests fail to provide a definitive diagnosis.
Why is it important to keep on blood thinners?
Because you may be at risk of another deep vein thrombosis or pulmonary embolism, it's important to continue treatment, such as remaining on blood thinners, and be monitored as often as suggested by your doctor. Also, keep regular doctor visits to prevent or treat complications.
What does a blood test for D dimer mean?
Your doctor may order a blood test for the clot-dissolving substance D dimer. High levels may suggest an increased likelihood of blood clots, although many other factors can also cause high D dimer levels. Blood tests also can measure the amount of oxygen and carbon dioxide in your blood.
Can a chest X-ray show pulmonary embolism?
Although X-rays can't diagnose pulmonary embolism and may even appear normal when pulmonary embolism exists , they can rule out conditions that mimic the disease.

Types of Blockages
Possible Symptoms
Causes
- Venous thromboembolism and arterial thromboembolism affect many of the same people and share several risk factors, but there are key distinctions between the two.
How Thromboembolism Is Diagnosed
- The diagnosis of thromboembolism largely involves imaging studies in combination with blood and lab tests. Some tests are organ-specific.
Treatment
- The treatment of venous or arterial thromboembolism can vary based on the location of the embolus and the extent of the blockage. Medications are central to any plan.
Summary
- Thromboembolism describes the obstruction of a blood vessel by a blood clot that has become dislodged from another site in the circulatory system. There is both venous thromboembolism (in which a vein is blocked) and arterial thromboembolism (in which an artery is blocked). Symptoms of thromboembolism vary by the location of the blockage. Venous thromboembolism often occu…
A Word from Verywell
- Thromboembolism is almost invariably serious, requiring immediate medical attention. Arguably, the biggest challenge is recognizing the signs and acting quickly. It helps to identify your risk factors for conditions like DVT, heart attack, and stroke, and do what you can to minimize the risks. For example, if you have heart disease and are on a long-distance flight, be sure to wear a …