Full Answer
Can hemorrhagic colitis be stopped?
There is no known method to stop Hemorrhagic colitis, but the essential part of its treatment is taking a lot of fluids, and in some cases, blood transfusion. This is because, during the ailment, the body loses so much fluid.
What are the treatment options for colitis?
For some conditions, certain types of surgery might also be used. For some of the causes of colitis, part of the treatment plan may include care that can be done at home. Changes to diet might also be used for some conditions, either long-term or for a short period of time.
What is haemorrhagic colitis?
Hemorrhagic colitis is an inflammation of the stomach and the large intestine. It is caused by a strain type of Escherichia coli, a gram-negative bacterium.
Why are antibiotics not used to treat E coli hemorrhagic colitis?
Antibiotics are not given for hemorrhagic colitis suspected to be caused by E. coli because they do not lessen symptoms, they do not prevent the spread of the infection, and they increase the risk of developing the hemolytic-uremic syndrome. The illness just goes away on its own.

How is hemorrhagic colitis treated?
Treatment for hemorrhagic colitis is supportive care; most illnesses are self-limited. At present, there is no evidence that antimicrobial therapy shortens the course of illness or prevents the development of sequelae.
What causes hemorrhagic colitis?
The most common causes of an acute ischemic/hemorrhagic colitis pattern of injury are ischemia, infections, radiation injury, certain drug reactions, and some phases of IBD (Fig. 13.29). Escherichia coli andClostridium difficile are two of the more common infections that cause acute hemorrhagic colitis.
What bacteria causes hemorrhagic colitis?
There are many strains of Escherichia coli (E. coli) that cause diarrhea or bloody diarrhea (hemorrhagic colitis). In North America, the most common strain that causes bloody diarrhea is E. coli O157:H7.
What is antibiotic associated hemorrhagic colitis?
Antibiotic-associated hemorrhagic colitis is a distinct form of antibiotic-associated diarrhea in which no C. difficile is detected. It is typically observed after a short course of therapy with penicillins and, to a lesser extent, after cephalosporins.
What does hemorrhagic colitis mean?
Hemorrhagic colitis is the name of the acute disease caused by Escherichia coli O157:H7. The illness is characterized by severe cramping (abdominal pain) and diarrhea which is initially watery but becomes grossly bloody. Occasionally, vomiting occurs.
What bacteria causes bloody diarrhea?
There are numerous organisms capable of producing acute, bloody diarrhea in the developed world. Most cases tend to be caused by Campylobacter jejuni, Escherichia coli O157:H7, other Shiga toxin-producing E coli, Salmonella species, Shigella species, and Yersinia species.
What causes hemorrhagic colitis symptoms diagnosis and prevention?
The most common causes of an acute ischemic/hemorrhagic colitis pattern of injury are ischemia, infections, radiation injury, certain drug reactions, and some phases of IBD (Fig. 13.29). Escherichia coli andClostridium difficile are two of the more common infections that cause acute hemorrhagic colitis.
What is the best antibiotic for bacterial gastroenteritis?
Ampicillin is recommended for drug-sensitive strains. Trimethoprim-sulfamethoxazole, fluoroquinolones,* or third-generation cephalosporins (fluoroquinolones are not recommended for use in children) are also acceptable alternatives.
How long does bloody stool last with E. coli?
The infection makes sores in your intestines, so the stools become bloody. The bloody diarrhea may last for 2 to 5 days. You might have 10 or more bowel movements a day. Some people say their stools are “all blood and no stool.” You may have a mild fever or no fever.
How do you get rid of gut Klebsiella?
coli and Klebsiella infections can usually be treated with normal antibiotics like penicillin and cephalosporin. But when these bacteria produce ESBLs, they can cause infections that can no longer be treated by these antibiotics.
Does Bactrim cover Klebsiella?
BACTRIM is indicated in the treatment of severe or complicated urinary tract infections in adults and pediatric patients two months of age and older due to susceptible strains of Escherichia coli, Klebsiella species, Enterobacter species, Morganella morganii, Proteus mirabilis and Proteus vulgaris when oral ...
What is the best antibiotic for Klebsiella oxytoca?
Aminoglycosides are an important treatment option for KPC-producing organisms. It has been found that the production of carbapenemases is the most important molecular mechanism of such resistance, both epidemiologically and clinically.
How long does it take for bloody diarrhea to go away?
One to 2 days later, grossly bloody diarrhea replaces the watery diarrhea. In almost all patients, the disease resolves spontaneously, usually within 8 days. Investigation of the epidemic outbreaks of E. coli O157:H7 infection revealed that not all patients acquire the full syndrome of hemorrhagic colitis.
Can E. coli be tested for sorbitol?
Specimens may be examined using sorbitol fermentation as a strain marker; unlike most E. coli organisms, E. coli O157:H7 strains test negative for sorbitol or have delayed positive results. 658 Colonies that test negative for sorbitol at 24 hours can be screened with commercial O157 antisera.
Can E. coli O157 H7 be detected in stool?
Because routine stool culture media do not distinguish E. coli O157 :H7 from other strains of E. coli normally present in the stool, physicians suspecting hemorrhagic colitis caused by enterohemorrhagic E. coli should specifically request that stools be screened for these organisms. View chapter Purchase book.
What is the management of a child with hus?
Thus, the management of HUS encompasses the usual management of children with acute renal failure with additional management issues specific to HUS. General management of acute renal failure includes appropriate fluid and electrolyte management, antihypertensive therapy if the child demonstrates hypertension, and the initiation of renal replacement therapy when appropriate.
Can E. coli cause hemorrhagic colitis?
Contamination of leafy green vegetables with harmful strains of Escherichia coli can cause hemorrhagic colitis when the vegetables are ingested. O157:H7 is a serotype of the bacterial species E. coli and one of the Shiga toxin-producing forms of E. coli. A Biacore 3000 instrument has been used to immobilize an antibody to E. coli strain O157:H7 on the gold surface of a dextran-modified CM5 SPR sensor chip ( Si et al., 2011 ). Samples of E. coli O157:H7 served as the analyte. The limit of detection was 3 × 10 5 colony-forming units/mL. Regeneration of the chip was achieved repeatedly with NaOH, allowing a single chip to be used more than 50 times and permitting detection of multiple samples.
What is hemorrhagic colitis?
Knowledge Article. Hemorrhagic colitis is the name of the acute disease caused by Escherichia coli O157:H7. The illness is characterized by severe cramping (abdominal pain) and diarrhea which is initially watery but becomes grossly bloody. Occasionally, vomiting occurs.
Is hemorrhagic colitis a low grade disease?
Occasionally, vomiting occurs. Fever is either low-grade or absent. The illness is usually self-limited and lasts for an average of 8 days. Some individuals exhibit watery diarrhea only. The infective dose is unknown, but from a compilation of outbreak data, the dose may be as few as 10 organisms.
There are various causes of colitis and each has different treatments
Amber J. Tresca is a freelance writer and speaker who covers digestive conditions, including IBD. She was diagnosed with ulcerative colitis at age 16.
Home Remedies and Lifestyle
For some of the causes of colitis, part of the treatment plan may include care that can be done at home. Changes to diet might also be used for some conditions, either long-term or for a short period of time.
Over-the-Counter (OTC) Therapies
There aren't many over-the-counter remedies that may be recommended to treat the cause of colitis. Vitamin and mineral supplements might be recommended in some cases.
Prescriptions
There are many prescription medications and therapies used to treat colitis. The treatments used will be different based on the cause of colitis. In most cases, therapies are aimed at treating the underlying cause of the inflammation.
Surgeries and Specialist-Driven Procedures
Surgery may be used to treat colitis that’s caused by IBD. This includes either the partial or the total removal of the colon. Surgery might be used when medications have failed to control the disease or there is a risk of colon cancer.
Summary
The treatments for colitis will depend on the underlying cause. For most types, medication and a change in diet are used. For some types, surgery may be needed.
A Word From Verywell
The reasons for the development of colitis are varied, as are the treatments. The key is to get the cause of colitis diagnosed so that it can be treated early and effectively. One of the most important things to know about the early diagnosis and treatment is that bleeding from the rectum is not normal.
How to treat colitis?
Treatment of colitis depends upon the cause and often is focused on symptom relief, supportive care, and maintaining adequate hydration and pain control. Antibiotics may be prescribed to treat infectious causes of colitis. Some bacterial infections that cause colitis resolve without any antibiotic treatment.
What are the symptoms of colitis?
Symptoms of colitis depend upon the cause and may include. abdominal pain, cramping, diarrhea, with or without blood in the stool (one of the hallmark symptoms of colitis). Associated symptoms depend upon the cause of colitis and may include. fever, chills, fatigue,
What is the name of the inflammation of the colon?
Colitis describes inflammation of the colon (col=colon + itis=inflammation). Examples of causes (types) of colitis include. infection, for example, caused by bacteria like C. difficile, viruses, and parasites; inflammatory bowel disease like Crohn's disease and ulcerative colitis,
What is the definition of colitis?
Colitis definition and facts. Colitis refers to inflammation of the inner lining of the colon. There are numerous causes of colitis including infection, inflammatory bowel disease (Crohn's disease and ulcerative colitis are two types of IBD ), ischemic colitis, allergic reactions, and microscopic colitis. Symptoms of colitis depend upon the cause ...
Why does my stool have blood in it?
Common causes of blood in the stool include hemorrhoids; however, other serious causes of bleeding need to be investigated. Colitis is not the only cause of rectal bleeding. Other causes include diverticular disease of the colon ( diverticulitis ), colon polyps, anal fissures, and cancer.
What is the inflammation of the inner lining of the colon?
Colitis describes inflammation of the inner lining of the colon and can be associated with diarrhea, abdominal pain, bloating, and blood in the stool. This inflammation may be due to a variety of reasons, including the following: An illustration of the colon anatomy.
What causes a person to have diarrhea and pain?
Ischemia or lack of blood supply causes inflammation of the colon leading to pain, fever, and diarrhea (bowel movements may contain blood). As a person ages, the arteries that supply blood to the colon gradually narrow and can cause ischemic colitis.
Causes
An overgrowth of C. difficile bacteria usually happens due to a disruption of typical intestinal bacteria following a course of antibiotics. Certain strains of C. difficile are resistant to some antibiotics, may be able to overgrow, and can cause inflammation and bleeding.
Treatment
A person with this condition will need to stop taking any drugs that are causing the issue. A doctor may prescribe medications such as vancomycin or fidaxomicin (Dificid).
Causes
It is not certain what causes microscopic colitis, but doctors believe a combination of genetics and atypical immune system responses may be the reason.
Treatment
Doctors may prescribe the following medications for microscopic colitis:
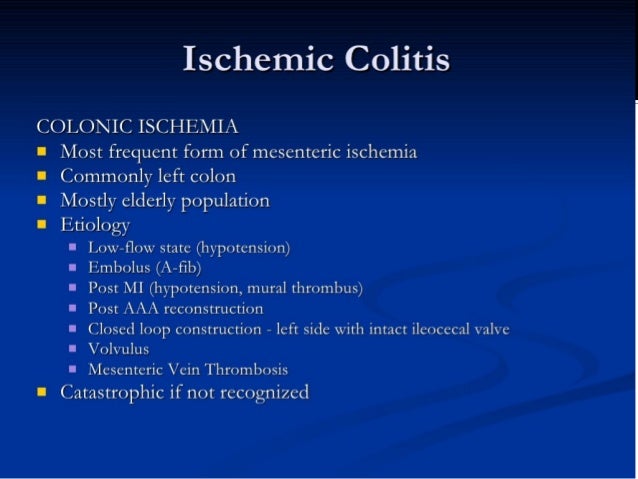
Causes
Ischemic colitis is caused by reduced blood flow to the colon. This can happen for various reasons, such as hardened arteries in people with peripheral vascular disease or coronary artery disease.
Treatment
Treatment for ischemic colitis depends on the severity of the condition. A doctor may treat mild cases with:
Symptoms
For some people, CMV colitis does not usually present any symptoms or it may be a self-limited disease, meaning it goes away on its own.
