Nutrition
5 rows · The 4-month TB treatment regimen (high-dose daily rifapentine with moxifloxacin, isoniazid, and ...
What is the best medicine for tuberculosis?
impurities in rifampin and rifapentine, two important anti-tuberculosis (TB) medications. People with TB disease or latent TB infection taking rifampin or rifapentine should continue taking their current medication, and should talk with their healthcare provider about any concerns. TB is a serious disease, and can be fatal if not treated properly.
Can You recover from tuberculosis without treatment?
Apr 08, 2020 · The most common treatment for active TB is isoniazid INH in combination with three other drugs—rifampin, pyrazinamide and ethambutol. You may begin to feel better only a few weeks after starting to take the drugs but treating TB …
What medications are used to treat tuberculosis?
Oct 11, 2003 · WHO recommends “standardised short-course chemotherapy... under proper case management conditions,” with the aim of adherence, completion of treatment, and therefore tuberculosis cure and prevention of drug resistance. These refer to a range of measures, including DOT, aimed at promoting treatment adherence and completion.
What should I do after the treatment of tuberculosis?
7 rows · Oct 05, 2020 · What is the best treatment for tuberculosis? Tuberculosis can only be treated effectively with ...
See more
8 rows · CDC and the National Tuberculosis Controllers Association (NTCA) preferentially recommend short-course, rifamycin-based, 3- or 4-month latent TB infection treatment regimens over 6- or 9-month isoniazid monotherapy. Short course regimens include: Three months of once-weekly isoniazid plus rifapentine (3HP) Four months of daily rifampin (4R) pdf icon

What is the best treatment for TB?
The usual treatment is: 2 antibiotics (isoniazid and rifampicin) for 6 months. 2 additional antibiotics (pyrazinamide and ethambutol) for the first 2 months of the 6-month treatment period.
How long does it take for tuberculosis to heal?
After taking TB medicine for several weeks, a doctor will be able to tell TB patients when they are no longer able to spread TB germs to others. Most people with TB disease will need to take TB medicine for at least 6 months to be cured.
Can you be completely cured of TB?
TB can usually be completely cured by the person with TB taking a combination of TB drugs. The only time that TB may not be curable is when the person has drug resistant TB.
What is first line treatment for TB?
Of the approved drugs, isoniazid (INH), rifampin (RIF), ethambutol (EMB), and pyrazinamide (PZA) are considered first-line anti-TB drugs and form the core of standard treatment regimens (Figure 6.4) (Table 6.2). Rifabutin (RBT) and rifapentine (RPT) may also be considered first- line drugs under certain circumstances.
Which food is not good for TB patients?
Foods To Avoid Limit intake of refined carbs such as maida and sugar-laden foods as they offer only empty calories devoid of nutrients. Deep-fried foods and junk foods packed with saturated fats and trans-fat would worsen symptoms associated with TB such as diarrhoea, abdominal cramps, and fatigue.Aug 11, 2021
Is there a vaccine for tuberculosis?
Bacille Calmette-Guérin (BCG) is a vaccine for tuberculosis (TB) disease. This vaccine is not widely used in the United States, but it is often given to infants and small children in other countries where TB is common. BCG does not always protect people from getting TB.
Can TB come back after 5 years?
The relapse rate differs by a country's incidence and control: 0–27% of TB relapses occur within 2 years after treatment completion and most relapses occur within 5 years; however, some relapses occur 15 years after treatment.
Can lungs heal after TB?
Researchers have found that more than one-third of patients who are successfully cured of TB with antibiotics developed permanent lung damage which, in the worst cases, results in large holes in the lungs called cavities and widening of the airways called bronchiectasis.Aug 11, 2019
Can TB come back after treatment?
Even with treatment, however, tuberculosis reinfection is becoming a problem. It's very common for people with tuberculosis to relapse during treatment. Treatment for tuberculosis symptoms can last anywhere from six months to a year, and sometimes more for drug-resistant tuberculosis.Dec 16, 2009
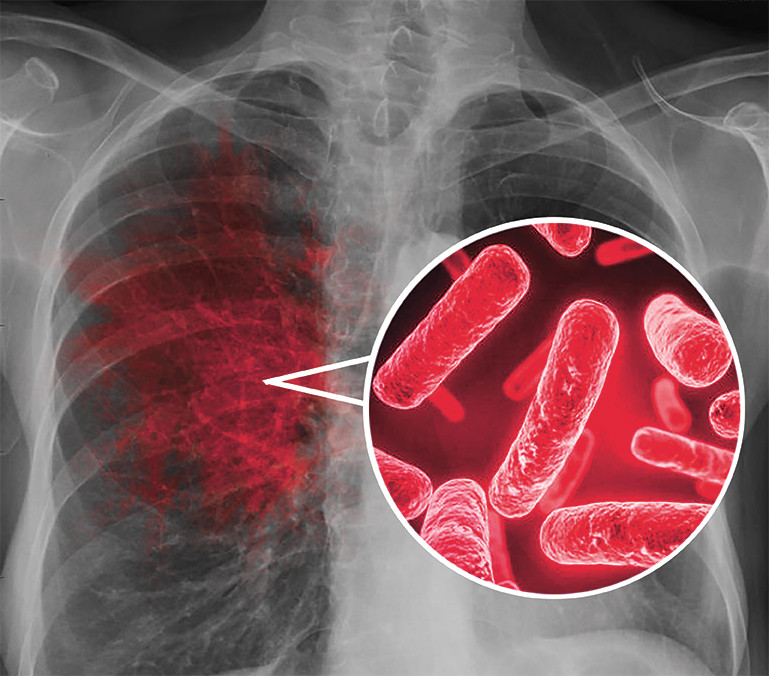
What are the 3 types of tuberculosis?
Tuberculosis is a bacterial infection that usually infects the lungs. It may also affect the kidneys, spine, and brain. Being infected with the TB bacterium is not the same as having active tuberculosis disease. There are 3 stages of TB—exposure, latent, and active disease.
Can TB be cured in 3 months?
ATLANTA - Health officials on Monday celebrated a faster treatment for people who have tuberculosis but aren't infectious, after investigators found a new combination of pills knocks out the disease in three months instead of nine.May 16, 2011
What is the name of TB medicine?
Rifampin, isoniazid, pyrazinamide, and ethambutol are first-line antitubercular medications, which are FDA-approved and indicated for the treatment of Mycobacterium tuberculosis infections.Nov 25, 2021
How long do you have to take antibiotics for tuberculosis?
For active tuberculosis, you must take antibiotics for at least six to nine months. The exact drugs and length of treatment depend on your age, overall health, possible drug resistance and where the infection is in your body.
What test is used to test for tuberculosis?
The most commonly used diagnostic tool for tuberculosis is a skin test, though blood tests are becoming more commonplace. A small amount of a substance called tuberculin is injected just ...
How long does ethambutol last?
If you have drug-resistant TB, a combination of antibiotics called fluoroquinolones and injectable medications, such as amikacin or capreomycin (Capastat), are generally used for 20 to 30 months. Some types of TB are developing resistance to these medications as well.
What is the test for TB?
Sputum tests. If your chest X-ray shows signs of tuberculosis, your doctor might take samples of your sputum — the mucus that comes up when you cough. The samples are tested for TB bacteria. Sputum samples can also be used to test for drug-resistant strains of TB.
What to do if you have a positive skin test?
If you've had a positive skin test, your doctor is likely to order a chest X-ray or a CT scan. This might show white spots in your lungs where your immune system has walled off TB bacteria, or it might reveal changes in your lungs caused by active tuberculosis.
Can a TB test be wrong?
Results can be wrong. The TB skin test isn't perfect. Sometimes, it suggests that people have TB when they don't. It can also indicate that people don't have TB when they do. You can have a false-positive result if you've been vaccinated recently with the bacille Calmette-Guerin (BCG) vaccine.
Can TB drugs cause liver damage?
Serious side effects of TB drugs aren't common but can be dangerous when they do occur. All tuberculosis medications can be toxic to your liver. When taking these medications, call your doctor immediately if you have any of the following:
Is TB a serious disease?
TB is a serious disease, and can be fatal if not treated properly. It is important to remember that all medications have risks and benefits. Learn more from CDC’s Dear Colleague letter. Not everyone infected with TB bacteria becomes sick. As a result, two TB-related conditions exist: latent TB infection and TB disease.
Can rifampin be used for TB?
Treatment. impurities in rifampin and rifapentine, two important anti-tuberculosis (TB) medications. People with TB disease or latent TB infection taking rifampin or rifapentine should continue taking their current medication, and should talk with their healthcare provider about any concerns.
What is the best treatment for TB?
The most common treatment for active TB is isoniazid INH in combination with three other drugs—rifampin, pyrazinamide and ethambutol. You may begin to feel better only a few weeks after starting to take the drugs but treating TB takes much longer than other bacterial infections.
How long does it take to treat TB?
The treatment for this type of TB takes much longer, 20 to 30 months to complete, and you may experience more side effects.
What are the side effects of TB?
While you are in treatment for active TB disease, you will need regular checkups to make sure your treatment is working. Everyone is different, but there are side effects associated with taking the medications, including: 1 Upset stomach, nausea and vomiting or loss of appetite 2 Tingling or numbness in the hands or feet 3 Itchy skin, rashes or bruising 4 Changes in your eyesight or blurred visions 5 Yellowish skin or eyes 6 Dark-colored urine 7 Weakness, fatigue or fever that for three or more days
What are the symptoms of TB?
Yellowish skin or eyes. Dark-colored urine. Weakness, fatigue or fever that for three or more days. It is important to tell your doctor or TB nurse immediately if you begin having any unusual symptoms while taking medicine for either preventive therapy or for active TB disease.
Can TB cause liver damage?
TB drugs can be toxic to your liver, and your side effects may be a warning sign of liver damage . If you are having trouble with tingling and numbness, your doctor may prescribe a vitamin B6 supplement while you are in treatment. It may also be possible to change TB medications if your side effects are serious.
Can you get TB from taking too much medicine?
You must finish your medicine and take the drugs exactly as prescribed. If you stop taking the drugs too soon you can become sick again and potentially spread the disease to others. Additionally, by taking the drugs incorrectly, TB germs that are still alive may become drug-resistant, making it harder for you to get better next time.
What is the most effective treatment for tuberculosis?
Isoniazid, which is also called INH, is the most widely used and effective drug against mycobacterium tuberculosis. However, it has several side effects. Most severely, isoniazid interferes with the body’s ability to make and use vitamin B12, or pyridoxine, which leads to nerve damage, called INH-induced neuropathy. Patients on isoniazid therapy will also be prescribed a pyridoxine supplement to prevent neuropathy.
What is the first line of treatment for TB?
The first-line treatment for active TB is a six-month antibiotic regimen consisting of a two-month intensive phase followed by a four-month continuation phase. In the intensive phase, patients will take four drugs that specifically target mycobacteria: isoniazid (INH), rifampin, ethambutol, pyrazinamide, and sometimes rifapentine. Only isoniazid and rifampin are used in the four-month continuation phase. Treatment may last as long as nine months.
What are the side effects of TB?
The most serious are liver problems and liver toxicity, so any course of treatment will involve regular blood tests to assess liver function. Isoniazid can also cause nerve damage and severe allergic reactions. Rifampin has a high incidence of hypersensitivity reactions. It also causes body excretions such as urine, sputum to turn reddish-brown/orange colored. Pyrazinamide causes pain in several joints. Ethambutol can cause painful swelling of the optic nerve that affects vision and could cause permanent blindness. A physician should be notified immediately if there is any vision change so ethambutol can be substituted with another antibiotic.
What is multidrug resistant tuberculosis?
Multidrug-resistant tuberculosis is defined as any strain that is resistant to both isoniazid and rifampin, making first-line antibiotic therapy useless. Other combinations of antibiotics are required for MDR-TB and XDR-TB, including second-line antibiotics (amikacin, kanamycin, streptomycin, capreomycin, viomycin, fluoroquinolones), and less-effective third-line antibiotics, such as linezolid, clarithromycin, and amoxicillin. It is extremely important to complete the full course of antibiotics as prescribed even though the symptoms improve within weeks. If antibiotics are stopped prematurely, a simple TB infection develops into an MDR-TB or XDR-TB infection.
How long has tuberculosis been around?
Tuberculosis has been around for thousands of years. In 2018, almost one-quarter of the human race was infected with tuberculosis. It has been 140 years since the tuberculosis bacterium was discovered, and medical science has created several antibiotics to help control this deadly illness.
How long does it take to get TB treatment?
TB treatment consists of a long treatment regimen of antibiotics. Typically lasting for six months, antibiotic treatment could take as long as 12 months. There are strict guidelines on antibiotics selection and duration. Side effects are common, often a source of discomfort, and can be severe. Because of drug resistance, healthcare providers follow a well-designed architecture of first-line, second-line, and third-line anti-tuberculosis drugs.
Is pulmonary TB contagious?
An active pulmonary TB infection is highly contagious, so patients will be asked to partially isolate themselves from family and other people they live with, wear a respirator mask at all times outside the house, and may even be hospitalized to prevent spreading the contagion.
What should a clinic decide on TB treatment?
Clinicians should choose the appropriate treatment regimen based on drug susceptibility results of the presumed source case (if known), coexisting medical conditions (e.g., HIV. ), and potential for drug-drug interactions. Consultation with a TB expert is advised if the known source of TB infection has drug-resistant TB.
What is the name of the drug that is used to treat TB?
Isoniazid (INH) Rifapentine (RPT) Rifampin (RIF) These medications are used on their own or in combination, as shown in the table below. CDC and the National Tuberculosis Controllers Association (NTCA) preferentially recommend short-course, rifamycin-based, 3- or 4-month latent TB infection treatment regimens over 6- or 9-month isoniazid ...
Is 6H or 9H better for TB?
Although effective, 6H and 9H have higher toxicity risk and lower treatment completion rates than most short-term treatment regimens. All treatment must be modified if the patient is a contact of an individual with drug-resistant TB disease.
How long does it take to treat TB in children?
Children over 2 years of age can be treated for latent TB infection with once-weekly isoniazid-rifapentine for 12 weeks. Alternative treatments for latent TB infection in children include 4 months of daily rifampin or 9 months of daily isoniazid.
Why is treatment recommended for children with latent TB?
Treatment is recommended for children with latent TB infection to prevent them from developing TB disease. Infants, young children, and immunocompromised children with latent TB infection or children in close contact with someone with infectious TB disease, require special consideration because they are at increased risk for getting TB disease.
How long does it take for TB to go away?
TB disease is treated by taking several anti-TB medicines for 6 to 9 months. It is important to note that if a child stops taking the drugs before completion, the child can become sick again. If drugs are not taken correctly, the bacteria that are still alive may become resistant to those drugs.
Why is TB so common in adults?
In comparison to children, TB disease in adults is usually due to past TB infection that becomes active years later, when a person’s immune system becomes weak for some reason (e.g., HIV infection, diabetes).
Can children take TB medicine?
It is very important that children or anyone being treated for latent TB infection or TB disease take the drugs exactly as instructed by the doctor and finish the medicine.
Where is TB common?
From countries where TB is common, including Mexico, the Philippines, Vietnam, India, China, Haiti, and Guatemala, or other countries with high rates of TB. (Of note, people born in Canada, Australia, New Zealand, or Western and Northern European countries are not considered at high risk for TB infection, unless they spent time in a country ...
Why is latent TB important?
Treatment of latent TB infection is essential to controlling TB in the United States because it substantially reduces the risk that latent TB infection will progress to TB disease.
How many people have latent TB?
In the United States, up to 13 million people may have latent TB infection. Without treatment, on average 1 in 10 people with latent TB infection will get sick with TB disease in the future. The risk is higher for people with HIV, diabetes, or other conditions that affect the immune system.
Can TB be treated with LTBI?
Persons with no known risk factors for TB may be considered for treatment of LTBI if they have either a positive IGRA result or if their reaction to the TST is 15 mm or larger. However, targeted TB testing programs should only be conducted among high-risk groups.
Can TB spread to others?
People with latent TB infection do not have symptoms, and they cannot spread TB bacteria to others. However, if latent TB bacteria become active in the body and multiply, the person will go from having latent TB infection to being sick with TB disease.
