Explore
Asystole is the most serious form of cardiac arrest and is usually irreversible. A cardiac flatline is the state of total cessation of electrical activity from the heart, which means no tissue contraction from the heart muscle and therefore no blood flow to the rest of the body.
Which intervention is most appropriate for the treatment of a patient in asystole?
If you can be treated, a doctor or paramedic may give you: Cardiopulmonary resuscitation ( CPR ). High-quality CPR acts like a heartbeat. This can keep blood flowing through your... Epinephrine. Also called adrenaline, this drug can boost blood flow. …
What is asystole and why should I worry about it?
For asystole, the standard medication to use is epinephrine. While treating asystole, epinephrine should be administered as soon as possible without delaying the start or continuation of CPR. Following the initial dose, epinephrine is given every 3-5 minutes as needed. During CPR, a rhythm check should be done every 2 minutes (5 cycles).
Can You shock a patient in asystole?
Mar 31, 2020 · The only two drugs recommended or acceptable by the American Heart Association (AHA) for adults in asystole are epinephrine and vasopressin. Atropine is no longer recommended for young children and...
Should we shock patients in asystole?
Jul 19, 2021 · Asystole should be treated following the current American Heart Association BLS and ACLS guidelines. High-quality CPR is the mainstay of treatment and the most important predictor of a favorable outcome. Asystole is a non-shockable rhythm. Therefore, if asystole is noted on the cardiac monitor, no attempt at defibrillation should be made.
:max_bytes(150000):strip_icc()/ankylosing-spondylitis-medications-5094631_final-2c4bf1e72033425fa000b34f2253e97f.jpg)
What to do if a patient is in asystole?
Asystole is treated by cardiopulmonary resuscitation (CPR) combined with an intravenous vasopressor such as epinephrine (a.k.a. adrenaline). Sometimes an underlying reversible cause can be detected and treated (the so-called "Hs and Ts", an example of which is hypokalaemia).
What is the first line drug of choice for asystole?
If the initial rhythm is pulseless electrical activity or asystole, an initial dose of epinephrine 1 mg IV/IO (intravenous/intraosseous) should be administered as soon as possible after recognition of cardiac arrest.
Do you shock a patient in asystole?
Asystole is a non-shockable rhythm. Therefore, if asystole is noted on the cardiac monitor, no attempt at defibrillation should be made. High-quality CPR should be continued with minimal (less than five seconds) interruption. CPR should not be stopped to allow for endotracheal intubation.Jul 19, 2021
What does epinephrine do in asystole?
Epinephrine is considered the single most useful drug in cardiac arrest; however, some authorities question its clinical effectiveness in humans This agent is used to increase coronary and cerebral blood flow during cardiopulmonary resuscitation (CPR) and may enhance automaticity during asystole.Mar 31, 2020
Do you give amiodarone for asystole?
The possible electrophysiologic mechanisms by which amiodarone might suppress both normal and abnormal pacemakers are discussed. The occurrence of asystole at therapeutic serum concentration of amiodarone suggests that this drug should be used with caution.
Do you give EPI for asystole?
When treating asystole, epinephrine can be given as soon as possible but its administration should not delay initiation or continuation of CPR. After the initial dose, epinephrine is given every 3-5 minutes.
What is the asystole protocol?
Asystole is not a shockable rhythm and treatment for Asystole involves high quality CPR, airway management, IV or IO therapy, and medication therapy which is 1mg epinephrine 1:10,000 every 3-5 minutes rapid IV or IO push. Remember, CPR should not be stopped for the delivery of medications.
What is asystole medical term?
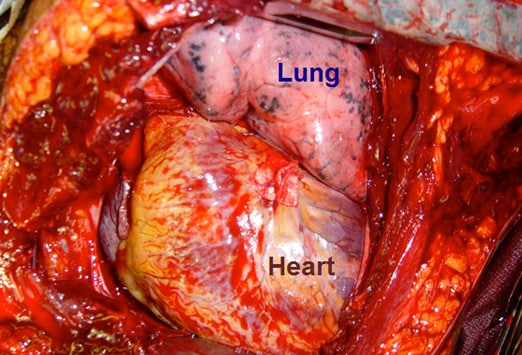
Asystole is also known as flatline. It is a state of cardiac standstill with no cardiac output and no ventricular depolarization, as shown in the image below; it eventually occurs in all dying patients.Mar 31, 2020
What is asystole in medical terms?
Medically Reviewed by James Beckerman, MD, FACC on February 11, 2020. Asystole (ay-sis-stuh-lee) is when there’s no electricity or movement in your heart. That means you don’t have a heartbeat. It’s also known as flatline.
What causes asystole in the heart?
One of them is certain types of arrhythmia, or irregular heartbeat. A heart injury or genetics -- something that runs in your family -- could also lead to asystole. If you’re worried about your heart, talk to your doctor. They’ll let you know if something’s going on and what you need to do.
What is the best medicine for asystole?
For asystole, the standard medication to use is epinephrine.
What is the term for a state of cardiac standstill in which all electrical activity has ceased?
Asystole, otherwise known as a flatline, is a state of cardiac standstill in which all electrical activity has ceased. It is diagnosed following a physical examination where no pulse is detected in conjunction with ECG monitoring.On an ECG tracing, asystole appears as a flatline:
Is vasopressin a good substitute for epinephrine?
Previous versions of the AHA guidelines have suggested that higher doses of epinephrine (greater than the standard 1mg dose), or an alternative vasopressor, called vasopressin, could be more effective alternatives to the standard dose of epinephrine.
What is the best medicine for asystole?
The only two drugs recommended or acceptable by the American Heart Association (AHA) for adults in asystole are epinephrine and vasopressin. Atropine is no longer recommended for young children and infants since 2005, and for adults since 2010 for pulseless electrical activity (PEA) and asystole.
Why is continuous cardiac monitoring important?
Continuous cardiac monitoring is useful during attempts at resuscitation to determine rhythm and effects of intervention. Endotracheal intubation is indicated during resuscitation. Central venous access or intraosseous access may be needed for vascular access.
What drugs cause pulseless arrest?
Street drugs and other chemicals can precipitate pulseless arrest. Cocaine is the most common street drug that increases incidence of pulseless arrest.
What are the H and T in ACLS?
The H’s and T’s of ACLS [1] is a mnemonic used to help recall the major contributing factors to a pulseless cardiac arrest including PEA , Asystole , Ventricular Fibrillation, and Ventricular Tachycardia .
What is a PEA?
Pulseless electrical activity (PEA) is a clinical condition characterized by unresponsiveness and no palpable pulse but with some organized cardiac electrical activity. Pulseless electrical activity has previously been referred to as electromechanical dissociation (EMD). With both asystole and PEA there is no blood flow to ...
What temperature should a hypothermic patient be?
The hypothermic patient may be unresponsive to drug therapy and electrical therapy (defibrillation or pacing). Core temperature should be raised above 86 F (30 C) as soon as possible.
What is a tamponade?
Tamponade. Cardiac tamponade is an emergency condition in which fluid accumulates in the pericardium (sac in which the heart is enclosed). The buildup of fluid results in ineffective pumping of the blood which can lead to pulseless arrest. ECG symptoms include narrow QRS complex and rapid heart rate.
What is the final differential diagnosis of the H and T?
The final differential diagnosis of the H’s and T’s is trauma. Trauma can be a cause of pulseless arrest, and a proper evaluation of the patients physical condition and history should reveal any traumatic injuries. Treat each traumatic injury as needed to correct any reversible cause or contributing factor to the pulseless arrest. Trauma was removed from the T’s but is still to be considered important during the assessment of any person in cardiac arrest.
Why do H's and T's need to be diagnosed?
Besides immediate CPR, the H’s and T’s need to be diagnosed and treated ASAP because there is so little time, a reason why even in a hospital survival chances are poor unless there immediate treatment available.
