Explore
Dec 18, 2017 · Status epilepticus (SE) is a very severe type of seizure. For someone who has seizures, they’re normally similar in length each time they occur and typically stop once that time period has passed....
What is status epilepticus (SE)?
How is status epilepticus treated? The healthcare provider will want to end the seizure as quickly as possible and treat any underlying problems that are causing it. You may receive oxygen, have blood tests, and an intravenous (IV) line. You may be given glucose (sugar) if low blood sugar may be causing the seizure.
What are the treatment options for status epilepticus?
Status epilepticus is a neurological emergency that is commonly encountered by the neurohospitalist. Successful treatment depends upon the recognition of prolonged seizure activity and the acute mobilization of available resources.
How long can a seizure last in status epilepticus?
Status epilepticus (SE) is a medical emergency that starts when a seizure that lasts longer than expected, usually considered around 5 minutes (or if there’s more than one seizure thta doesn't...
When should I worry about status epilepticus?
Status epilepticus (SE) is a medical emergency associated with significant morbidity and mortality. SE is defined as a continuous seizure lasting more than 30 min, or two or more seizures without full recovery of consciousness between any of them.

What is status epilepticus?
You may have status epilepticus if you have a seizure that lasts longer than 5 minutes, or if you have more than 1 seizure within a 5-minute period, without returning to a normal level of consciousness between episodes. This is a medical emergency. Call 911. It may lead to permanent brain damage or death.
What is the first line treatment for status epilepticus?
Early status epilepticus: first-line treatment The first-line treatment for early SE mainly comprises the administration of benzodiazepines, the most frequently used of which include diazepam, lorazepam, and midazolam.Nov 17, 2020
When do you treat status epilepticus?
Start first-line emergency treatment (i.e., benzodiazepine) in the first 5 to 20 minutes from presentation after excluding non-epileptic status (i.e., psychogenic non-epileptic seizures).Jul 13, 2020
What is the immediate IV treatment for status epilepticus?
Intravenous benzodiazepines-diazepam, midazolam or lorazepam and phenytoin are the first line drugs recommended for termination of seizures. Diazepam (or midazolam), thiopental and propofol infusion are useful for control of Refractory SE (RSE). Newer drugs are being investigated for use in SE.
How do you treat status?
How is status epilepticus treated? The healthcare provider will want to end the seizure as quickly as possible and treat any underlying problems that are causing it. You may receive oxygen, have blood tests, and an intravenous (IV) line. You may be given glucose (sugar) if low blood sugar may be causing the seizure.
What happens if epilepsy is not treated?
If epilepsy is not treated, seizures may occur throughout a person's life. Seizures can become more severe and happen more often over time. Epilepsy can be caused by tumors or improperly formed blood vessels.
Can you recover from status epilepticus?
Most seizures last less than 5 minutes. But sometimes they don't stop there – or they come one after the other, giving the person suffering from them no chance to recover.Mar 6, 2021
How do you break a status epilepticus?
Early status epilepticus It is usual to initiate treatment with a fast acting benzodiazepine, and intravenous lorazepam is the drug of choice. Alternatives include other intravenous benzodiazepines or intravenous lignocaine, the latter possibly being preferable in patients with respiratory disease.
What is the best treatment for a seizure?
Healthcare providers may use anti-seizure drugs to treat the problem, including: Diazepam. Lorazepam.
How long does an epilepsy seizure last?
Individuals who have epilepsy must take their medicine as directed. A seizure that lasts more than 5 minutes, or having more than 1 within a 5 minute period is an emergency that requires immediate medical care.
What causes seizures in the brain?
Many problems can cause you to have a seizure. These include high fever, brain infections, abnormal sodium or blood sugar levels, or head injuries. If you have epilepsy, you may have seizures repeatedly.
How long does it take for a seizure to go away?
If you have epilepsy, you may have seizures repeatedly. A seizure that lasts longer than 5 minutes, or having more than 1 seizure within a 5 minutes period, without returning to a normal level of consciousness between episodes is called status epilepticus. This is a medical emergency that may lead to permanent brain damage or death.
Can epilepsy cause death?
Complications depend on the underlying cause and can range from no complications to death. If the underlying cause, such as poor epilepsy control, can be fixed, there may no complications. If the underlying cause is a stroke or brain injury, complications may include physical disability from the cause or even death.
Can epilepsy cause permanent brain damage?
This is a medical emergency that may lead to permanent brain damage or death. Status epilepticus is very rare, most people with epilepsy will never have it. This condition is more common in young children and elderly adults. This condition can occur as:
How many people have status epilepticus?
Status epilepticus occurs in 50,000 to 150,000 people in the United States each year. It's more likely in children under 10, adults over 50, and those with febrile (fever-related) seizures. Studies note that between 30 percent and 44 percent of status epilepticus cases are in people previously diagnosed with epilepsy.
How common is epilepticus?
Death from status epilepticus is more common in men than in women, and it grows more common with age. Children under 10 have the best outcomes, with deaths in less than 3 percent of cases. That goes up to 30 percent for adults.
Why do we need an EEG?
EEG: Because the clinical symptoms of status epilepticus and several other conditions may be similar, an EEG is usually needed to distinguish between seizures and patterns that are consistent with conditions such as stroke and en cephalopathy. Brain imaging: A brain computed tomography (CT) or magnetic resonance imaging ...
What causes seizures in the brain?
Cerebral damage: People who have had extensive damage to the cerebral cortex, the region of the brain most likely to produce seizures, are more likely to experience status epilepticus than people who have small areas of limited brain damage. Hypoxia (low oxygen) prior to birth, cerebral palsy, head trauma, and severe blood loss can cause ...
How long does a seizure last?
In general, seizures tend to last from a few seconds to a few minutes, depending on the type of seizure. However, prolonged seizures can occur—and are always an emergency. The symptoms of status epilepticus may be easy to recognize in some situations, but not others.
Who is Sarah Rahal?
Sarah Rahal, MD, is a double board-certified adult and pediatric neurologist and headache medicine specialist. Status epilepticus is a dangerous situation historically defined as a seizure or a cluster of seizures lasting longer than 30 minutes without improvement in consciousness.
What is the medical term for a seizure that causes death?
Status epilepticus is a medical emergency. It can cause death due to physical injury, choking, or as a result of the seizure itself. The episode may cause lasting brain damage, which can result in worsening seizures, increased predisposition to status epilepticus, and cognitive decline.
What is status epilepticus?
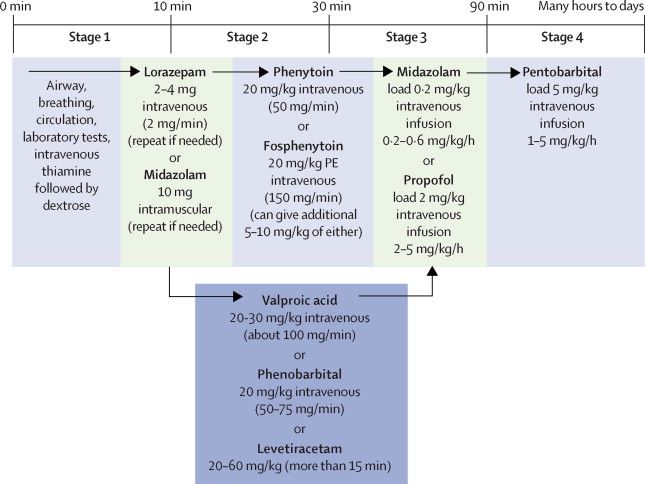
Abstract. Status epilepticus is a neurological emergency that is commonly encountered by the neurohospitalist. Successful treatment depends upon the recognition of prolonged seizure activity and the acute mobilization of available resources.
What is the most common form of SE?
SE can be categorized into convulsive and nonconvulsive status epilepticus (NCSE). Generalized convulsive status epilepticus (GCSE) is the most commonly encountered form of SE. Nonconvulsive SE can represent an evolved stage of previous GCSE or can occur in complex partial status epilepticus (CPSE).
Is midazolam a first line drug?
Midazolam is rarely used as a first-line drug for SE but is commonly used as a continuous intravenous infusion for RSE. It can be used acutely and is frequently used because of physician familiarity and its many routes of administration. These include the intramuscular, rectal, sublingual, and nasal routes.
Is lorazepam a benzodiazepine?
Lorazepam is considered the benzodiazepine of choice for the treatment of individual seizures and SE. It has a slightly longer onset of action, approximating 2 minutes; however, it is less lipid soluble than diazepam and has a duration of action greater than 12 hours.
Is diazepam a lipid soluble drug?
It is, however, highly lipid soluble, leading to rapid redistribution and decreases in brain concentrations. Clinical effectiveness is only about 20 minutes. Relapse rate is high and thus a second drug is required if diazepam is used as a first-line drug.27Diazepam can be given rectally in gel form and intramuscularly.
How long does a seizure last?
Most seizures last less than 5 minutes. But sometimes they don’t stop there – or they come one after the other, giving the person suffering from them no chance to recover. “Status epilepticus” literally means a continuous state of seizure.
How long does a tonic phase last?
To be safe, call 911 if the tonic phase – the first phase -- lasts for more than 5 minutes, or if another seizure seems to start right after one finishes.
What happens during the tonic phase?
In the tonic phase (which usually lasts less than 1 minute), your body becomes stiff and you lose consciousness. Your eyes roll back into your head, your muscles contract, your back arches, and you have trouble breathing. As the clonic phase starts, your body spasms and jerks.
What is status epilepticus?
Status epilepticus (SE) is a medical emergency associated with significant morbidity and mortality. SE is defined as a continuous seizure lasting more than 30 min, or two or more seizures without full recovery of consciousness between any of them. Based on recent understanding of the pathophysiology, it is now considered that any seizure that lasts more than 5 min probably needs to be treated as SE. GABAergic mechanisms play a crucial role in terminating seizures. When the seizure persists, GABA-mediated mechanisms become ineffective and several other putative mechanisms of seizure suppression have been recognized. Early treatment of SE with benzodiazepines, followed if necessary by fosphenytoin administration, is the most widely followed strategy. About a third of patients with SE may have persistent seizures refractory to the first-line medications. They require aggressive management with second-line medications such as barbiturates, propofol, or other agents. In developing countries where facilities for assisted ventilation are not readily available, it may be helpful to use nonsedating antiepileptic drugs (such as sodium valproate, levetiracetam, or topiramate) at this stage. It is important to recognize SE and institute treatment as early as possible in order to avoid a refractory state. It is equally important to attend to the general condition of the patient and to ensure that the patient is hemodynamically stable. This article reviews current knowledge regarding the management of convulsive SE in adults.
What is the classification of status epilepticus?
Classification of status epilepticus. Semiologically and electrophysiologically there are several types of seizures; these have been broadly classified as either generalized or partial seizures by the International League Against Epilepsy. In principle there can be as many types of SE as there are types of seizures.
What is nonconvulsive status epilepticus?
Nonconvulsive status epilepticus. Nonconvulsive SE (NCSE) refers to continuous or near-continuous generalized electrical seizure activity lasting for at least 30 min, but without physical convulsions. CSE may evolve into the nonconvulsive form after treatment or NCSE may arise de novo.
What is a SE?
Gastaut stated that ‘there are as many types of SE as there are types of epileptic seizures’ and defined SE as ‘a term used whenever a seizure persists for a sufficient length of time or is repeated frequently enough to produce a fixed or enduring epileptic condition’. [ 3] .
How many cases of SE are there in the US?
It has been estimated that up to 150,000 cases of SE occur annually in the US, with 55,000 associated deaths. [ 2] Geography, sex, age, and race influence the epidemiology of SE. An incidence of 6.2–18.3 per 100,000 population has been reported in the US. [ 12] Regardless of geographic influences, SE appears to be more frequent among men, blacks, and the aged. [ 13] The incidence of SE in the elderly population is at least twice that in the general population. [ 14] SE in the elderly is of great concern because concurrent medical conditions often exist that are likely to complicate therapy and worsen the prognosis. [ 15]
Is SE refractory to treatment?
The longer an episode of SE continues, the more refractory to treatment it becomes and the greater is the likelihood of complications. More prolonged seizures carry higher risk of mortality; [ 8] hence it would be useful to initiate treatment for SE even as the patient is being transported to the hospital. Paramedics and ambulance staff, if trained appropriately, could administer preliminary treatment even before shifting the patient to the hospital and save valuable time.
What are the stages of SE?
SE may be broadly divided into two stages [ Table 3 ]. [ 28] The first stage is characterized by generalized convulsive tonic–clonic seizures that are associated with an increase in autonomic activity, resulting in hypertension, hyperglycemia, sweating, salivation, and hyperpyrexia. During this phase, cerebral blood flow is increased due to increased cerebral metabolic demands. After approximately 30 min of seizure activity, patients enter the second phase, which is characterized by the failure of cerebral autoregulation, decrease in cerebral blood flow, increase in intracranial pressure, and systemic hypotension. During this phase, electromechanical dissociation may occur in which, although electrical cerebral seizure activity continues, the clinical manifestations may be restricted to minor twitching.
What is the Treatment Choice for Status Epilepticus?
There are certain guidelines which have to be followed for treating status epilepticus. A time-dependent treatment guideline is to be followed for proper management-
What are the Various Modes of Administration of the Treatment for Status Epilepticus?
Status epilepticus is a condition where a patient might need immediate medication. Thus the mode of drugs to be given as a treatment procedure for status epilepticus is also varied.
How to Reduce the Risk of Death from Status Epilepticus?
As it is clear that status epilepticus can be a form of medical emergency, it is important to understand the importance of proper medicine to reduce the risk of death due to status epilepticus. The patient should ask for a written care plan from the doctor or the nurse for emergency circumstances.
What is status epilepticus?
Status epilepticus is an emergency. If your child has a seizure or several seizures that last for 5 minutes or longer, call your local emergency services (911 in the U.S.).
How to help a child with a seizure?
In general, a witness to a seizure should:#N#Cushion and support your child’s head and body.#N #Move your child away from dangerous places, such as the street.#N#Move sharp objects out of the area.#N#Turn your child on his or her side. If your child vomits this will help keep their airway clear.#N#Avoid unnecessarily restraining your child. This will not stop the seizure.#N#Not place anything in your child’s mouth.#N#Call for emergency medical help.#N#Stay with your child until he or she recovers.
What is status epilepticus?
Status epilepticus is defined usually as a condition in which epileptic activity persists for 30 minutes or more. The seizures can take the form of prolonged seizures or repetitive attacks without recovery in between. There are various types of status epilepticus and a classification scheme is shown in table 1.
How long does anaesthesia last for seizures?
In most patients, if seizures continue for 60–90 minutes in spite of the treatment outlined above, full anaesthesia is required. In some emergency situations (for example, postoperative status, severe or complicated convulsive status, patients already in the intensive therapy unit (ITU)), anaesthesia can and should be introduced earlier. The prognosis in status requiring anaesthesia is much poorer, and there is a high risk of mortality and morbidity. The principles of treatment are similar for all anaesthetics, and a wide range of barbiturate and non-barbiturate anaesthetic agents could be used.
What causes cerebral damage?
The cerebral damage in status is caused by systemic and metabolic disturbance (for example, hypoxia, hypoglycaemia, raised intracranial pressure) and also by the direct excitotoxic effect of seizure discharges (which result in calcium influx into neurons and a cascade of events resulting in necrosis and apoptosis).
What should be included in an emergency investigation?
Emergency investigations should include assessment of the following: blood gases, glucose, renal and hepatic function, calcium, magnesium, full blood count, clotting screen, and anticonvulsant concentrations. Serum should be saved for toxicology or virology or other future analyses.
What is the best treatment for respiratory disease?
Alternatives include other intravenous benzodiazepines or intravenous lignocaine, the latter possibly being preferable in patients with respiratory disease. In most episodes of status, initial treatment will be highly effective. Even if seizures cease, 24 hour inpatient observation should follow.
What are the three first line treatments?
These are subanaesthetic doses of phenobarbitone, phenytoin or fosphenytoin. All three are given by intravenous loading, and followed by repeated oral (phen ytoin or phenobar bitone) or intravenous supplementation.
What is de novo absence?
De novo absence status of late onset is a condition which presents in later life, usually without a history of recent epilepsy. It is commonly caused by drug withdrawal (especially psychotropic drugs or benzodiazepines), and can be safely treated by intravenous diazepam, lorazepam or chlormethiazole.