
Full Answer
What is the best approach to treat chronic pain?
• RECOMMENDATION 1B: Use an integrated multidisciplinary approach that may include existing evidence-based psychological and behavioral interventions (e.g., CBT, coping skills, stress reduction, mindfulness-oriented recovery) to address chronic pain when clinically indicated.
What are primary care settings for chronic pain management?
Primary healthcare settings appears to be ideally situated to deliver holistic care for the patient with chronic pain, addressing the health needs within the community [ 9 ], while integrating preventative, promotive, curative, and rehabilitation services.
Why do we provide best practice recommendations and pain medication recommendations?
We provide best practice recommendations and pain medication recommendations (Tables (Tables11–4) with the hope that they can be used by orthopaedic practices and other specialties (eg, primary care and emergency medicine) to improve the management of acute pain following musculoskeletal injury.
What are the recommendations for pain management education for older adults?
• RECOMMENDATION 1C: Establish appropriate pain management education for physicians and health care providers who treat older adults. 2.7.3 Patients with Cancer-Related Pain and Patients in Palliative Care
What is the standard treatment for chronic pain?
The list of pharmacological options for chronic pain is extensive. This list includes nonopioid analgesics such as nonsteroidal anti-inflammatories (NSAIDs), acetaminophen, and aspirin. Additionally, medications such as tramadol, opioids, antiepileptic drugs (gabapentin or pregabalin) can be useful.
What is the practice of pain management?
Also called pain management clinics, they're health care facilities that focus on the diagnosis and management of chronic pain. There are two kinds. One focuses on procedures to deal with specific types of pain, like neck and back pain.
What are standards of assessing pain?
Patients should be asked to describe their pain in terms of the following characteristics: location, radiation, mode of onset, character, temporal pattern, exacerbating and relieving factors, and intensity. The Joint Commission updated the assessment of pain to include focusing on how it affects patients' function.
What is first line treatment for chronic pain?
Non-opioid medications are typically first-line medications for chronic, non-malignant, nociceptive pain. Select agents within this group include acetaminophen, NSAIDs and COX-2 inhibitors such as celecoxib.
Which of the following are standardized pain rating scales?
Pain Assessment ScalesNumerical Rating Scale (NRS)Visual Analog Scale (VAS)Defense and Veterans Pain Rating Scale (DVPRS)Adult Non-Verbal Pain Scale (NVPS)Pain Assessment in Advanced Dementia Scale (PAINAD)Behavioral Pain Scale (BPS)Critical-Care Observation Tool (CPOT)
What are 3 different types of pain management?
Pain Management for Specific Types of Pain Acute pain: nonopioids, weak opioids, opioids, nonpharmacological treatments such as ice or bioelectric therapy. Chronic pain: nonopioids, weak opioids, opioids, antidepressants, capsaicin cream, nonpharmacological treatments such as bioelectric therapy, radiation therapy.
What is PQRST stand for?
The mnemonic device PQRST offers one way to recall assessment:P. stands for palliative or precipitating factors, Q for quality of pain, R for region or radiation of pain, S for subjective descriptions of pain, and T for temporal nature of pain (the time the pain occurs).
What are the nursing interventions for pain?
Nursing Interventions for Acute PainProvide measures to relieve pain before it becomes severe. ... Acknowledge and accept the client's pain. ... Provide nonpharmacologic pain management. ... Provide pharmacologic pain management as ordered. ... Manage acute pain using a multimodal approach.More items...•
What should a nurse assess regarding a patient's pain?
Measuring pain Pain should be measured using an assessment tool that identifies the quantity and/or quality of one or more of the dimensions of the patients' experience of pain. This includes the: intensity of pain; intensity and associated anxiety and behaviour.
What is first line and second line treatment?
Second-line treatment is treatment for a disease or condition after the initial treatment (first-line treatment) has failed, stopped working, or has side effects that aren't tolerated. It's important to understand "lines of treatment" and how they differ from first line treatment and can play a role in clinical trials.
What is first line of treatment?
THAYR-uh-pee) The first treatment given for a disease. It is often part of a standard set of treatments, such as surgery followed by chemotherapy and radiation. When used by itself, first-line therapy is the one accepted as the best treatment.
What are comfort measures for pain management pharmacological?
Comfort therapy Heat/cold application. Lotions/massage therapy. Meditation. Music, art, or drama therapy.
What is chronic pain?
For these Guidelines, chronic pain is defined as pain of anyetiology not directly related to neoplastic involvement, asso-ciated with a chronic medical condition or extending in du-ration beyond the expected temporal boundary of tissue in-jury and normal healing, and adversely affecting the functionor well-being of the individual.
What is considered part of a multimodal strategy for chronic pain?
behavioral therapy, biofeedback, or relaxation training: Theseinterventions may be used as part of a multimodal strategyfor low back pain and for other chronic pain conditions.Supportive psychotherapy, group therapy, or counseling:These interventions may be considered as part of a multimo-dal strategy for chronic pain management.
What is a history and physical examination?
History and physical examination: The Task Force recog-nizes that conducting a history and physical examination andreviewing diagnostic studies by a physician are well establishedas essential components of each patient’s evaluation. Althoughno controlled trials were found that address the impact of con-ducting a history (e.g., reviewing medical records and patientinterviews), physical examination, or psychologic or behavioralevaluation, numerous studies address the identification of cer-tain health disorders (e.g., diabetes, multiple sclerosis, or post-traumatic injury) that are associated with specific pain condi-tions (e.g., complex regional pain syndrome [CRPS] orneuropathic pain) (Category B2 evidence). Studies with observa-tional findings suggest that a physical examination may aid inthe diagnosis of some chronic pain disorders (Category B2 evi-dence), and an observational study suggests that a psychologicevaluation may be helpful in the prediction of treatment success(Category B2 evidence).
What is chronic pain?
Chronic pain may result from an underlying disease or health condition, an injury, medical treatment (such as surgery), inflammation, or a problem in the nervous system (in which case it is called “neuropathic pain”); or the cause may be unknow n.
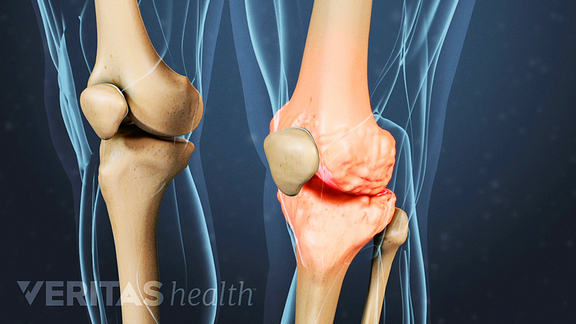
What are the most common chronic pain conditions?
Not all people with chronic pain have a health problem diagnosed by a health care provider, but among those who do, the most frequent conditions by far are low-back pain or osteoarthritis, according to a national survey. Other common diagnoses include rheumatoid arthritis, migraine, carpal tunnel syndrome, and fibromyalgia.
What are some complementary therapies that can help with pain?
A growing body of evidence suggests that some complementary approaches, such as acupuncture, hypnosis, massage, mindfulness meditation, spinal manipulation, tai chi, and yoga, may help to manage some painful conditions.
What is PubMed in medical terms?
A service of the National Library of Medicine, PubMed® contains publication information and (in most cases) brief summaries of articles from scientific and medical journals. For guidance from NCCIH on using PubMed, see How To Find Information About Complementary Health Approaches on PubMed.
How long does yoga help with back pain?
A 2018 evaluation of the research on yoga for low-back pain by the Agency for Healthcare Research and Quality (AHRQ) found that it improved pain and function in both the short term (1 to 6 months) and intermediate term (6 to 12 months). The effects of yoga were similar to those of exercise.
How long does chronic pain last?
Chronic pain is pain that lasts more than several months (variously defined as 3 to 6 months, but longer than “normal healing”). It’s a very common problem. Results from the 2012 National Health Interview Survey show that: About 25.3 million U.S. adults (11.2 percent) had pain every day for the previous 3 months.
How does pain affect your life?
Pain can affect quality of life and productivity, and it may be accompanied by difficulty in moving around, disturbed sleep, anxiety, depression, and other problems . 1. For more information about chronic pain, visit the National Institute of Neurological Disorders and Stroke.
Overview
This guideline provides recommendations related to the management of patients with chronic pain.
Members Only Content
Join APTA to get unlimited access to content including evidence-based research, guidance on payment changes, and other resources to help you thrive. Learn more about membership benefits.
What is chronic pain?
Chronic pain can be the result of an underlying medical disease or condition, injury, medical treatment, inflammation, or an unknown cause ( 4 ). Estimates of the prevalence of chronic pain vary, but it is clear that the number of persons experiencing chronic pain in the United States is substantial.
What are the consequences of chronic pain?
There are clinical, psychological, and social consequences associated with chronic pain including limitations in complex activities, lost work productivity, reduced quality of life, and stigma, emphasizing the importance of appropriate and compassionate patient care ( 4 ).
What is the opioid prescribed for?
Background. Opioids are commonly prescribed for pain. An estimated 20% of patients presenting to physician offices with noncancer pain symptoms or pain-related diagnoses (including acute and chronic pain) receive an opioid prescription ( 1 ).
What is the CDC guideline for opioids?
This guideline provides recommendations for primary care clinicians who are prescribing opioids for chronic pain outside of active cancer treatment, palliative care, and end-of-life care. The guideline addresses 1) when to initiate or continue opioids for chronic pain; 2) opioid selection, dosage, duration, follow-up, and discontinuation; and 3) assessing risk and addressing harms of opioid use. CDC developed the guideline using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) framework, and recommendations are made on the basis of a systematic review of the scientific evidence while considering benefits and harms, values and preferences, and resource allocation. CDC obtained input from experts, stakeholders, the public, peer reviewers, and a federally chartered advisory committee. It is important that patients receive appropriate pain treatment with careful consideration of the benefits and risks of treatment options. This guideline is intended to improve communication between clinicians and patients about the risks and benefits of opioid therapy for chronic pain, improve the safety and effectiveness of pain treatment, and reduce the risks associated with long-term opioid therapy, including opioid use disorder, overdose, and death. CDC has provided a checklist for prescribing opioids for chronic pain ( http://stacks.cdc.gov/view/cdc/38025) as well as a website ( http://www.cdc.gov/drugoverdose/prescribingresources.html) with additional tools to guide clinicians in implementing the recommendations.
How many people were prescribed opioids in 2005?
On the basis of data available from health systems, researchers estimate that 9.6–11.5 million adults, or approximately 3%–4% of the adult U.S. population, were prescribed long-term opioid therapy in 2005 ( 15 ). Opioid pain medication use presents serious risks, including overdose and opioid use disorder.
How often should you evaluate opioids?
Clinicians should evaluate benefits and harms with patients within 1 to 4 weeks of starting opioid therapy for chronic pain or of dose escalation. Clinicians should evaluate benefits and harms of continued therapy with patients every 3 months or more frequently.
Can opioids be used for chronic pain?
Although the transition from use of opioid therapy for acute pain to use for chronic pain is hard to predict and identify , the guideline is intended to inform clinicians who are considering prescribing opioid pain medication for painful conditions that can or have become chronic.
