Medication
8 rows · Rheumatoid arthritis is a chronic disorder for which there is no known cure. Fortunately in the ...
Procedures
Sep 02, 2018 · Rheumatoid arthritis (RA) is a chronic, inflammatory, systemic autoimmune disease, affecting the joints with varying severity among patients. The risk factors include age, gender, genetics, and environmental exposure (cigarette smoking, air …
Therapy
Treatment for RA usually includes the use of medications that slow disease and prevent joint deformity, called disease-modifying antirheumatic drugs (DMARDs); biological response modifiers (biologicals) are medications that are an effective second-line treatment.
Self-care
Methotrexate is a conventional disease-modifying anti-inflammatory drug (DMARD). It works to lower inflammation and slow an overactive immune system, which occurs in rheumatoid arthritis.The new guidelines strongly recommend methotrexate alone (monotherapy) as the first treatment for people with moderate to high disease activity who haven’t taken DMARDs before.
Nutrition
Oct 15, 2021 · Imaging results can also show how well treatment is working. Treatment The goals of RA treatment are to: Stop inflammation or reduce it to the lowest possible level (put disease in remission). Relieve symptoms. Prevent joint and organ damage. Improve function and overall well-being. Reduce long-term complications.
What is the latest RA treatment?
Natural Treatments for Rheumatoid Arthritis Heat and cold. . Ice packs can reduce joint swelling and inflammation. Put a cold compress or ice pack (wrapped in a... Relaxation. . Try progressive muscle relaxation. This is when you tense or tighten one muscle group and then relax it. Capsaicin. . It's ...
What are the natural treatments for RA?
May 18, 2021 · Rheumatoid arthritis is a chronic inflammatory disorder that can affect more than just your joints. In some people, the condition can damage a wide variety of body systems, including the skin, eyes, lungs, heart and blood vessels.
What is the first line treatment for RA?
What are treatment options for RA?

Which treatment is best for rheumatoid arthritis?
Methotrexate is usually the first medicine given for rheumatoid arthritis, often with another DMARD and a short course of steroids (corticosteroids) to relieve any pain. These may be combined with biological treatments....The DMARDs that may be used include:methotrexate.leflunomide.hydroxychloroquine.sulfasalazine.
Is RA a serious disease?
RA is a very serious autoimmune disease, in which your immune system mistakenly attacks your own body's tissues and causes severe joint pain, stiffness, severe fatigue, and sometimes deformity, usually in the hands, shoulders, knees, and/or feet. It affects men, women, and children of all ages.Sep 14, 2018
What is the safest treatment for RA?
The American College of Rheumatology recommends methotrexate as the first medication providers should consider when treating people with rheumatoid arthritis. In head-to-head clinical trials, methotrexate was found to be equally or more effective, and have fewer side effects, than other nonbiologic DMARDs.Oct 6, 2020
What is the main cause of rheumatoid arthritis?
Rheumatoid arthritis is an autoimmune condition, which means it's caused by the immune system attacking healthy body tissue. However, it's not yet known what triggers this. Your immune system normally makes antibodies that attack bacteria and viruses, helping to fight infection.
What are the five signs of rheumatoid arthritis?
5 Common Rheumatoid Arthritis Symptoms to Watch Out ForChronic Fatigue. Fatigue from RA goes beyond simple tiredness or sleepiness. ... Pain or Stiffness in the Morning. ... More Than One Joint is Affected. ... There are Issues With Your Eyes, Mouth, or Skin. ... Pain Moves From Smaller Joints to Larger Ones.Apr 13, 2018
Is RA curable?
There is no cure for rheumatoid arthritis. But clinical studies indicate that remission of symptoms is more likely when treatment begins early with medications known as disease-modifying antirheumatic drugs (DMARDs).May 18, 2021
Where does RA start?
Early rheumatoid arthritis tends to affect your smaller joints first — particularly the joints that attach your fingers to your hands and your toes to your feet. As the disease progresses, symptoms often spread to the wrists, knees, ankles, elbows, hips and shoulders.May 18, 2021
What are the 4 stages of rheumatoid arthritis?
The 4 Stages of Rheumatoid Arthritis ProgressionStage 1: Early RA. ... Stage 2: Antibodies Develop and Swelling Worsens. ... Stage 3: Symptoms Are Visible. ... Stage 4: Joints Become Fused. ... How to Know if Your RA Is Progressing. ... What Makes RA Get Worse? ... How Your RA Treatment Plan Prevents Disease Progression.More items...•Nov 14, 2018
What are usually the first signs of rheumatoid arthritis?
The early warning signs of RA include:Fatigue. Before experiencing any other symptoms, a person with RA may feel extremely tired and lack energy. ... Slight fever. Inflammation associated with RA may cause people to feel unwell and feverish. ... Weight loss. ... Stiffness. ... Joint tenderness. ... Joint pain. ... Joint swelling. ... Joint redness.More items...
What are 3 symptoms of rheumatoid arthritis?
What are the signs and symptoms of RA?Pain or aching in more than one joint.Stiffness in more than one joint.Tenderness and swelling in more than one joint.The same symptoms on both sides of the body (such as in both hands or both knees)Weight loss.Fever.Fatigue or tiredness.Weakness.
What does RA pain feel like?
A person with RA may feel intense pain in their joints during flares. This may feel like sustained pressure, a burning sensation, or a sharp pain. However, people with RA may also experience periods of remission when they feel few to no symptoms. In addition to causing pain in the joints, RA can affect the whole body.Jul 16, 2021
Is RA caused by stress?
Rheumatoid arthritis (RA) is a chronic inflammatory joint condition and an autoimmune disease that can be caused by stress, according to research. Stress triggers rheumatoid arthritis by setting off the immune system's inflammatory response in which cytokines are released.Aug 28, 2020
What Is Rheumatoid Arthritis (RA)?
Rheumatoid arthritis, or RA, is an autoimmune and inflammatory disease, which means that your immune system attacks healthy cells in your body by m...
What Are The Signs and Symptoms of RA?
With RA, there are times when symptoms get worse, known as flares, and times when symptoms get better, known as remission.Signs and symptoms of RA...
What Are The Risk Factors For RA?
Researchers have studied a number of genetic and environmental factors to determine if they change person’s risk of developing RA.Characteristics t...
Who Should Diagnose and Treat RA?
A doctor or a team of doctors who specialize in care of RA patients should diagnose and treat RA. This is especially important because the signs an...
What Are The Complications of RA?
Rheumatoid arthritis (RA) has many physical and social consequences and can lower quality of life. It can cause pain, disability, and premature dea...
How Can I Manage Ra and Improve My Quality of Life?
RA affects many aspects of daily living including work, leisure and social activities. Fortunately, there are multiple low-cost strategies in the c...
Learn More About Arthritis
1. Arthritis Types 2. Physical Activity for Arthritis 3. Frequently Asked Questions (FAQs) 4. Arthritis-Related Statistics
How to fix rheumatoid arthritis?
Surgery may help restore your ability to use your joint. It can also reduce pain and improve function. Rheumatoid arthritis surgery may involve one or more of the following procedures: Synovectomy. Surgery to remove the inflamed lining of the joint (synovium) can help reduce pain and improve the joint's flexibility. Tendon repair.
What are the drugs that slow the progression of rheumatoid arthritis?
Conventional DMARDs. These drugs can slow the progression of rheumatoid arthritis and save the joints and other tissues from permanent damage. Common DMARDs include methotrexate (Trexall, Otrexup, others), leflunomide (Arava), hydroxychloroquine (Plaquenil) and sulfasalazine (Azulfidine). Side effects vary but may include liver damage ...
How does rheumatoid arthritis affect your life?
The pain and disability associated with rheumatoid arthritis can affect a person's work and family life. Depression and anxiety are common, as are feelings of helplessness and low self-esteem. The degree to which rheumatoid arthritis affects your daily activities depends in part on how well you cope with the disease.
Why is rheumatoid arthritis so difficult to diagnose?
Rheumatoid arthritis can be difficult to diagnose in its early stages because the early signs and symptoms mimic those of many other diseases. There is no one blood test or physical finding to confirm the diagnosis. During the physical exam, your doctor will check your joints for swelling, redness and warmth.
What tests can be done to diagnose rheumatoid arthritis?
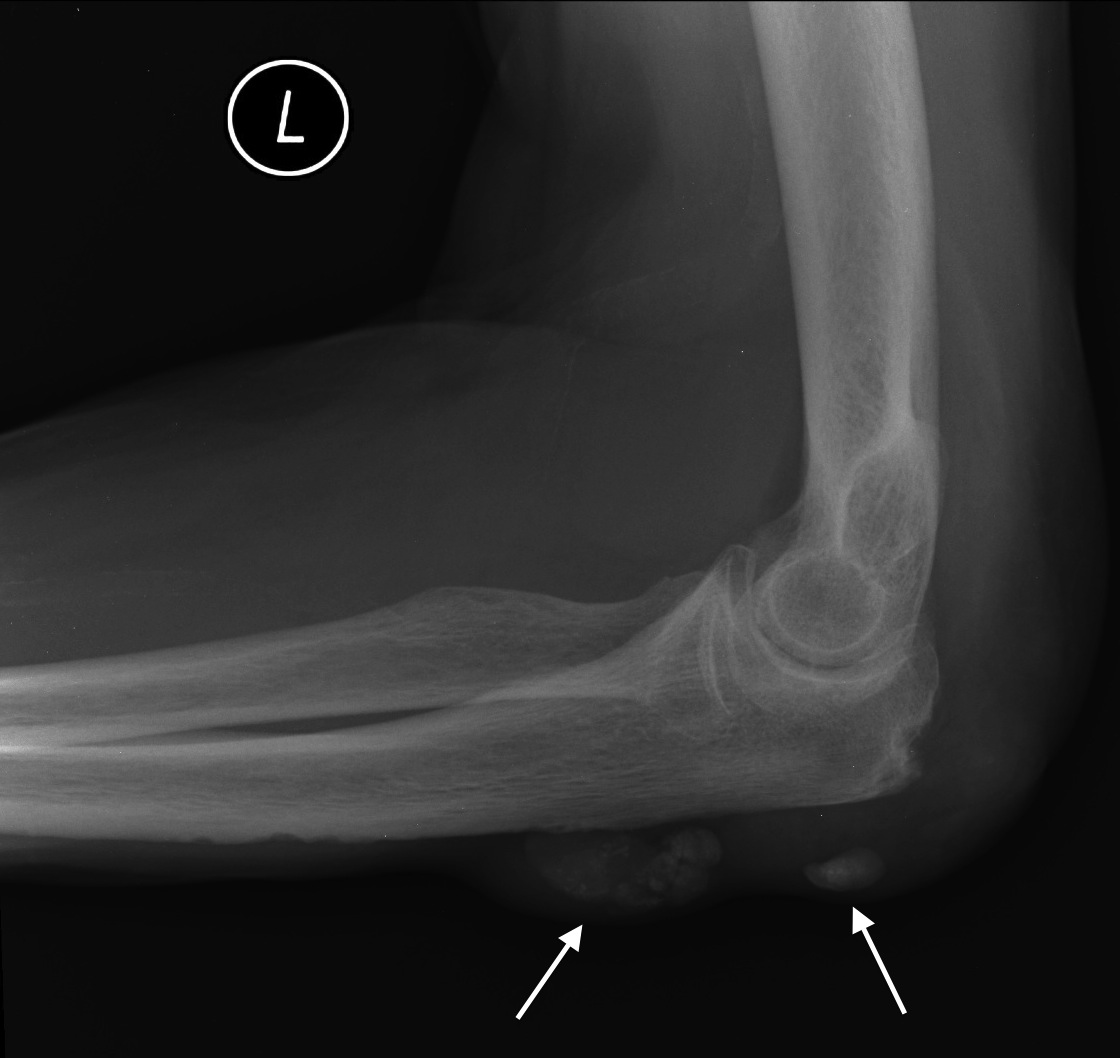
Imaging tests. Your doctor may recommend X-rays to help track the progression of rheumatoid arthritis in your joints over time. MRI and ultrasound tests can help your doctor judge the severity of the disease in your body.
What does elevated erythrocyte sedimentation rate mean?
People with rheumatoid arthritis often have an elevated erythrocyte sedimentation rate (ESR, also known as sed rate) or C-reactive protein (CRP) level, which may indicate the presence of an inflammatory process in the body.
How to get rid of a swollen joint?
If you're just getting started, begin by taking a walk. Avoid exercising tender, injured or severely inflamed joints. Apply heat or cold.
What is the goal of rheumatoid arthritis treatment?
The goal of rheumatoid arthritis treatment now aims toward achieving the lowest possible level of arthritis disease activity and remission if possible, minimizing joint damage, and enhancing physical function and quality of life.
What are the different types of rheumatoid arthritis drugs?
There are three general classes of drugs commonly used in the treatment of rheumatoid arthritis: non-steroidal anti-inflammatory agents (NSAIDs), corticosteroids, and disease modifying anti-rheumatic drugs (DMARDs). NSAIDs and corticosteroids have a short onset of action while DMARDs can take several weeks or months to demonstrate a clinical effect. DMARDs include methotrexate, sulfasalazine, leflunomide (Arava®), etanercept (Enbrel®), infliximab (Remicade®), adalimumab (Humira®), certolizumab pegol (Cimzia®), golimumab (Simponi®), abatacept (Orencia®), rituximab (Rituxan®), tocilizumab (Actemra®), anakinra (Kineret®), antimalarials (e.g. Plaquenil®). Other immunomodulators are occasionally used including azathioprine (Imuran) and cyclosporine. Because cartilage damage and bony erosions frequently occur within the first two years of disease, rheumatologists now move aggressively to a DMARD agent early in the course of disease, usually as soon as a diagnosis is confirmed. Analgesic drugs are also sometimes helpful in decreasing pain until DMARDs take effect. A summary table of how to monitor drug treatment in rheumatoid arthritis is included.
What are the benefits of DMARD?
Although both NSAIDs and DMARD agents improve symptoms of active rheumatoid arthritis, only DMARD agents have been shown to alter the disease course and improve radiographic outcomes. DMARDs have an effect upon rheumatoid arthritis that is different and may be slower. In most cases, when the diagnosis of rheumatoid arthritis is confirmed, DMARD agents should be started. The presence of erosions or joint space narrowing on x-rays of the involved joints is a clear indication for DMARD therapy, however one should not wait for x-ray changes to occur. The currently available drugs include: 1 Methotrexate (Rheumatrex®, Trexall®) 2 Hydroxychloroquine (Plaquenil ®) 3 Sulfasalazine (Azulfidine®) 4 Leflunomide (Arava®) 5 Tumor Necrosis Factor Inhibitors — etanercept (Enbrel®, adalimumab (Humira ®), and infliximab (Remicade®), certolizumab pegol (Cimzia®), golimumab (Simponi®) 6 T-cell Costimulatory Blocking Agents —abatacept (Orencia®) 7 B cell Depleting Agents —rituximab (Rituxan®) 8 Interleukin-6 (IL-6) Inhibitors– tocilizumab (Actemra®) 9 Interleukin-1 (IL-1) Receptor Antagonist Therapy —anakinra (Kineret®) 10 Intramuscular Gold 11 Other Immunomodulatory and Cytotoxic agents — azathioprine (Imuran®) and cyclosporine A (Neoral®, Sandimmune®)
What is a DMARD?
Disease Modifying Anti-rheumatic Drugs (DMARDS) Although both NSAIDs and DMARD agents improve symptoms of active rheumatoid arthritis, only DMARD agents have been shown to alter the disease course and improve radiographic outcomes. DMARDs have an effect upon rheumatoid arthritis that is different and may be slower.
How long does it take for folic acid to work after methotrexate?
These side effects can often be overcome by increasing folic acid or using an activated form of folic acid known as folinic acid (leukovorin®) given as a 5mg dose 12 hours and sometimes 24 hours after methotrexate is given. Some patients complain of GI upset (nausea or diarrhea) with oral methotrexate.
How long does it take for NSAIDS to work?
Usual Time to Effect: The onset of action is seen in as early as 4 to 6 weeks.
When did TNF antagonists start being used?
TNF antagonists were the first of the biological DMARDS to be approved for the treatment of RA. These drugs began to enter the market for rheumatoid arthritis in 1999 and are now considered a part the ACR recommendations for treatment of RA.
What is the best treatment for RA?
Gold salts, such as aurothioglucose (Solganal), auranofin (Ridaura), gold sodium thiomalate (Myochrysine), and D-penicillamine (Depen and Cuprimine) have been used frequently in the treatment of RA. These DMARDs require frequent blood and urine tests due to damage to the bone marrow and kidneys.
What is RA in medical terms?
Rheumatoid arthritis (RA) is a chronic, symmetrical, inflammatory autoimmune disease that initially affects small joints, progressing to larger joints, and eventually the skin, eyes, heart, kidneys, and lungs. Often, the bone and cartilage of joints are destroyed, and tendons and ligaments weaken [1].
How long does it take for RA to show symptoms?
Common symptoms of RA include morning stiffness of the affected joints for > 30 min, fatigue, fever, weight loss, joints that are tender, swollen and warm, and rheumatoid nodules under the skin. The onset of this disease is usually from the age of 35 to 60 years, with remission and exacerbation.
What is sulfasalazine used for?
Sulfasalazine (Azulfidine) is a DMARD typically used in the treatment of irritable bowel disease. Combined with anti-inflammatory medications, this DMARD can be used to treat RA.
What supplements can help with RA?
Home remedies have been proven to be helpful for patients suffering from RA, although they are not as effective as DMARDs. Fish oils and omega-3 fatty acid supplements are beneficial for the short-term symptoms of RA. Cumin has been shown to have anti-inflammatory effects in patients with this disease.
What is joint fusion?
Joint fusion can be done to stabilize joints that are not easily replaceable such as the ankle, wrist, thumb, and cervical spine. A procedure for soft-tissue release can be done to correct severe contractures around joints causing decreased range of motion; this is an older procedure that is not commonly utilized [45].
What are the side effects of biologics?
Nonetheless, biologics pose the problem of serious side effects, such as increased risk of infections. Other common side effects include neurologic diseases like multiple sclerosis and lymphoma [27, 28, 29]. Tumor necrosis factor (TNF) is a messenger protein that promotes inflammation in joints.
What is RA in medical terms?
What is rheumatoid arthritis (RA)? Rheumatoid arthritis, or RA, is an autoimmune and inflammatory disease, which means that your immune system attacks healthy cells in your body by mistake, causing inflammation (painful swelling) in the affected parts of the body. RA mainly attacks the joints, usually many joints at once.
What is RA in the hands?
RA mainly attacks the joints, usually many joints at once. RA commonly affects joints in the hands, wrists, and knees. In a joint with RA, the lining of the joint becomes inflamed, causing damage to joint tissue. This tissue damage can cause long-lasting or chronic pain, unsteadiness (lack of balance), and deformity (misshapenness).
What are the consequences of rheumatoid arthritis?
It can cause pain, disability, and premature death. Premature heart disease. People with RA are also at a higher risk for developing other chronic diseases such as heart disease and diabetes.
Why is RA risk the highest?
The risk of RA may be highest when people with these genes are exposed to environmental factors like smoking or when a person is obese. Smoking. Multiple studies show that cigarette smoking increases a person’s risk of developing RA and can make the disease worse. History of live births.
How to help arthritis?
Learn more about physical activity for arthritis. Go to effective physical activity programs. If you are worried about making arthritis worse or unsure how to safely exercise, participation in physical activity programs can help reduce pain and disability related to RA and improve mood and the ability to move.
What is the best way to diagnose RA?
A doctor or a team of doctors who specialize in care of RA patients should diagnose and treat RA. This is especially important because the signs and symptoms of RA are not specific and can look like signs and symptoms of other inflammatory joint diseases.
How do you know if you have RA?
Signs and symptoms of RA include: Pain or aching in more than one joint. Stiffness in more than one joint. Tenderness and swelling in more than one joint. The same symptoms on both sides of the body (such as in both hands or both knees) Weight loss. Fever.
What is the best treatment for rheumatoid arthritis?
Methotrexate. Methotrexate is a conventional disease-modifying anti-inflammatory drug (DMARD). It works to lower inflammation and slow an overactive immune system, which occurs in rheumatoid arthritis. The new guidelines strongly recommend methotrexate alone (monotherapy) as the first treatment for people with moderate to high disease activity who ...
How many recommendations are there for non-drug treatment for RA?
Since then, new drugs have hit the market, older drugs have been reassessed, and there’s more evidence for the role of nondrug treatments for RA. Of 44 recommendations, only seven were considered strong, meaning there’s clear evidence that the benefits of the treatment outweigh the risks and most patients endorse them.
How are biosimilars created?
Biosimilars are created by slightly changing the manufacturing process used for the original or reference drug. The 2020 guideline acknowledges the safety and efficacy of biosimilars and encourage their use — a shift from the ACR stance in 2015. One hurdle to broader use of biosimilars is that insurers have been reluctant to pay for them. In 2019, insurers approved a biosimilar before a biologic just 14% of the time. Plus, copays for biosimilars are often about the same as for the reference drug. Whether biosimilars will really make biologics more affordable remains to be seen.
What is the most important factor in all treatment considerations?
The most important factor in all treatment considerations is shared decision-making, where patients are informed of all their options, including nondrug ones, and have a full voice in their own care. “Patients were involved in every step of the process [of creating the update], and the recommendations truly reflect their perspectives,” Dr. Fraenkel says.
What is the treatment to target approach?
Although there’s not much evidence to support it, a treat-to-target approach is strongly recommended for patients who haven’t taken biologics or small molecule drugs. In treat-to-target, doctors and patients decide on a goal and adjust treatment until the goal is reached. Though everyone hopes for remission, many patients may not be able to achieve it. A more realistic aim is low disease activity, which keeps symptoms under control and helps maintain a good quality of life. Still, the guideline states the goal should be tailored to each patient and remission can be the target when possible.
Why are the remaining recommendations called conditional?
The remaining recommendations are called conditional because they lack good evidence one way or the other. The new guidelines don’t address vaccinations — particularly relevant right now — or nondrug therapies like diet and exercise. Those are expected in a later update. Here are some of the main takeaways:
Is methotrexate monotherapy or adalimumab?
The new guidelines strongly recommend metho trexate alone (monotherapy) as the first treatment for people with moderate to high disease activity who haven’t taken DMARDs before. Methotrexate mono therapy is strongly recommended over other conventional DMARDs, a biologic DMARD like adalimumab ( Humira) and small molecule drugs such as Janus kinase ...
What is RA in medical terms?
Rheumatoid arthritis is an inflammatory type of arthritis that can causes joint pain, swelling and damage. Learn what causes RA and how to treat it. Rheumatoid arthritis (RA) causes joint inflammation and pain. It happens when the immune system doesn’t work properly and attacks the lining of the joints (called the synovium).
Why is rest important for RA?
Rest is important when RA is active, and joints feel painful, swollen or stiff. Rest helps reduce inflammation and fatigue that can come with a flare. Taking breaks throughout the day protects joints and preserves energy.
How long does RA pain last?
In the early stages, people with RA may not see redness or swelling in the joints, but they may experience tenderness and pain. Joint pain, tenderness, swelling or stiffness that lasts for six weeks or longer. Morning stiffness that lasts for 30 minutes or longer. More than one joint is affected.
What percentage of people with RA have high ESR?
A high ESR or CRP combined with other clues to RA helps make the diagnosis. Rheumatoid factor (RF) is an antibody found (eventually) in about 80 percent of people with RA. Antibodies to cyclic citrullinated peptide (CCP) are found in 60 to 70 percent of people with RA. However, they are also found in people without RA.
Why does my joint feel so tender?
That’s the tissue lining around a joint that produces a fluid to help the joint move smoothly. The inflamed synovium gets thicker and makes the joint area feel painful and tender, look red and swollen and moving the joint may be difficult. Researchers aren’t sure why some people develop RA.
What is the best doctor for arthritis?
A doctor with specialized training in treating arthritis (called a rheumatologist) is the best person to make a correct diagnosis, using medical history, a physical examination and lab tests. Medical history.
What are the symptoms of RA?
The same joints on both sides of the body are affected. Many people with RA get very tired (fatigue) and some may have a low-grade fever. RA symptoms may come and go.
What is the best treatment for rheumatoid arthritis?
Physical therapy and occupational therapy make a big difference to your daily life. They are key parts of any rheumatoid arthritis treatment plan. Physical therapists can give you an exercise plan, teach you how to use heat and ice, do therapeutic massage, and encourage and motivate you.
How to reduce rheumatoid arthritis pain?
Exercise , Joint Pain, and Rheumatoid Arthritis. When your joints are stiff and painful, exercise might be the last thing on your mind. Yet with RA, exercising regularly is one of the best things you can do. People who work out live longer, with or without rheumatoid arthritis. Regular exercise can cut down on RA pain.
What is the goal of a therapist?
The goal is to improve your emotional and psychological well-being as you develop ways to relax, handle stress, and pace yourself. For instance, it may include activity scheduling, guided imagery, relaxation, distraction, and creative problem-solving. Exercise, Joint Pain, and Rheumatoid Arthritis.
What is the best treatment for arthritis pain?
Acupuncture. Studies show that acupuncture curbs pain, may lower the need for painkillers, and is good for helping affected joints stay flexible. Mind/body therapy. Mind/body therapies can help with stress management, plus improve sleep and how you react to pain.
What joints need replacement?
If joint pain and inflammation become unbearable or joints are severely damaged, some people need joint replacement surgery. The hips and knees, and sometimes the shoulders, are the most common joints that get replaced. Surgery can dramatically improve pain and mobility.
How to treat joint damage?
Treatment usually includes medications, occupational or physical therapy, and exercise. Some people need surgery to correct joint damage. Early treatment is key to good results. And with today’s treatments, joint damage can often be slowed or stopped.
What are the side effects of IV steroids?
More widespread IV reactions may include chest pain, trouble breathing, and hives. Each drug has its own set of side effects that you should talk about with your doctor. Steroids. For severe RA or when symptoms flare, your doctor may recommend steroids to ease pain and stiffness.

Diagnosis
Treatment
Clinical Trials
Lifestyle and Home Remedies
Specialist to consult
Alternative Medicine
- Following a strict treatment regimen could bring RA into remission. Remission means that the level of disease activity has decreased in the body. It is never an indication that symptoms will not return, but following remission, many patients can go for long periods of time without experienci…
Coping and Support
Preparing For Your Appointment