Treatment for pericoronitis may involve: 4
- Dental cleaning/flushing of food and other debris from the area
- Antibiotic administration (to take by mouth)
- An antibacterial oral rinse
- Pain relief (either over-the-counter pain relievers or prescription medication may be suggested by the dentist)
What is acute pericoronitis and how is it treated?
Acute pericoronitis is when the symptoms intensify to fever, swelling, and pain, which indicate a spreading infection. Pericoronitis is differentiated from periodontal disease (or periodontitis) in that it occurs specifically around a partially erupted tooth where the tooth has not completely emerged from the gum overlying it.
What can the dentist do for pericoronitis?
The dentist may also prescribe a pain medication. If the pain and inflammation are severe, or if the pericoronitis recurs, it may be necessary to have oral surgery to remove the gum flap or wisdom tooth. Your dentist can make the appropriate referral to the oral and maxillofacial surgeon.
How do you prevent pericoronitis?
Prevention of pericoronitis. The only thing a patient with an impacted tooth can do to prevent pericoronitis is to take extra care for the oral hygiene around that tooth, and try to avoid injuring the area with hard foods. Unfortunately there is not much that can be done to prevent the impaction of a tooth.
What is pericoronitis and how do you get it?
This allows an opening for bacteria to enter around the tooth and cause an infection. In cases of pericoronitis, food or plaque (a bacterial film that remains on teeth after eating) may get caught underneath a flap of gum around the tooth.

Can pericoronitis go away on its own?
Unfortunately, pericoronitis won't go away on its own. If it goes untreated, it can become dangerous after only a couple of weeks. Typically, either the flap of tissue or the wisdom tooth needs to be removed. If an infection is present, an antibiotic will be needed, as well.
What is the fastest way to cure pericoronitis?
Most people with pericoronitis have a flap of gum tissue partially covering the crown of the erupting tooth....Home remedies include:over-the-counter pain relievers.warm salt-water rinses.oral water irrigators.good oral hygiene, including brushing and flossing.
Is pericoronitis serious?
Inflamed and painful gum tissue around your wisdom teeth and molars may be signs of pericoronitis. If you leave these symptoms untreated, you risk spreading an infection to your neck, causing jaw spasms. In rare cases, complications can be life-threatening.
What is pericoronitis caused by?
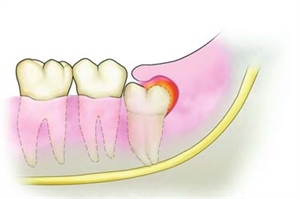
What causes Pericoronitis? Pericoronitis occurs around a wisdom tooth that has failed to come in or has only partially erupted. A partially-erupted wisdom tooth can leave a flap of gum tissue that collects food particles and other debris—an ideal breeding ground for bacteria.
What does pericoronitis look like?
The dentist will diagnose the condition by examining the wisdom teeth and checking for signs and the appearance of pericoronitis. The dentist will look to see if the gums are inflamed, red, swollen, or draining pus. They will also look to see if there is a gum flap in the affected area.
Does Salt Water Cure pericoronitis?
The most conservative treatment option is to use a salt water rinse to clean the infected area, flushing out any bacteria and any food pieces that might be trapped in the gum. To reduce the chance of the infection recurring, a dentist might decide to remove the piece of gum that is causing part of the trouble.
How can I treat pericoronitis at home?
If a wisdom tooth has pericoronitis or another type of abscess, a saltwater rinse can help clean the infected area until the source is treated. Dissolve a small amount of salt in warm water and swish for 30 seconds one to two times per day.
Can I brush over pericoronitis?
Treatment. Now that you know the risks and the unpleasant symptoms of this condition, how do you get well from pericoronitis? If you have mild pericoronitis, it's possible to get better with some diligent home care. You can gently brush the affected area to loosen up the plaque and bacteria build up.
When should I worry about pericoronitis?
The most common symptoms of pericoronitis is pain and swelling around the tooth. It is possible to treat these symptoms with over the counter pain medications and rinsing the mouth with warm salt water. If this helps manage the symptoms and the rest of the tooth emerges, there is no need to worry about it.
Can mouthwash cure pericoronitis?
What About Mouthwash for Pericoronitis? Mouthwash can be a useful tool in a pericoronitis treatment plan. Simple saltwater rinse can help reduce mild inflammation and is safe to use while you are waiting to see your dentist.
How do I know if my pericoronitis is infected?
Acute symptoms include:Pain.Swelling in the gum tissue (caused by an accumulation of fluid)Pus discharge.Trismus, or difficulty opening your mouth and jaw, also called lockjaw.Pain with swallowing.Fever.Loss of appetite.Infection.More items...•
Is pericoronitis common?
Pericoronitis is a dental condition that causes infection and inflammation of the soft tissues surrounding a partially erupted tooth, as an article in the British Journal of General Practice (BJGP) explains. Approximately 81% of people in their 20s experience this condition at some time.
What to do if you have pericoronitis?
Those who have severe symptoms of pericoronitis should immediately contact a dentist, or other healthcare provider. Symptoms of pericoronitis are grouped into three different categories according to their frequency and intensity, 2 these include: Acute-involves limited mouth opening and more severe symptoms.
What is the best medicine for pericoronitis?
Pain relievers (such as ibuprofen [Advil] or acetaminophen [Tylenol] or other over-the-counter pain relievers prescribed by the dentist). Note: Avoid the use of hot compresses (which may increase the swelling) particularly for those with severe symptoms of pericoronitis such as fever or swelling of the neck or face)
What is the prevalence of pericoronitis in Greece?
The prevalence of pericoronitis was 4.92% of the 20 to 25-year-old study participants.
What is chronic pain?
Chronic-involves low grade pain without severe symptoms. The treatment of pericoronitis is often dependent on the level (acute, sub-acute or chronic) of the disease a person is experiencing.
How to tell if you have pericoronitis?
Mild symptoms of pericoronitis may include: 2 . Painful, swollen gum tissue (near the tooth that is affected) Difficulty biting down (without hitting the swollen area) A discharge of pus from the inflamed area. A bad taste in the mouth or unpleasant smell.
Which tooth is most affected by pericoronitis?
The tooth that is most often affected by pericoronitis is the lower third or final set of molars sometimes called wisdom teeth. 1 In fact, it is rare that pericoronitis involves any teeth other than the bottom wisdom teeth.
Is oral hygiene a factor in pericoronitis?
Oral hygiene was found to be a marginally significant factor in the prevalence of the disease. Smokers were found to be more susceptible to pericoronitis (but the frequency of smoking was not impactful). The chronic type of pericoronitis was the most frequent form of the disease.
How to treat pericoronitis?
It's normal to experience a short-term case of pericoronitis that lasts for three to four days when teeth first erupt, explains the BJGP article. If this happens, there are several actions you can take at home to ease your symptoms and improve your oral hygiene: 1 Brush your teeth thoroughly twice a day. 2 Floss or use interdental brushes daily. 3 Rinse your mouth with a chlorhexidine-based mouthwash.
How to treat a swollen gum?
If this happens, there are several actions you can take at home to ease your symptoms and improve your oral hygiene: Brush your teeth thoroughly twice a day. Floss or use interdental brushes daily. Rinse your mouth with a chlorhexidine-based mouthwash.
Can a cold precede a pericoronitis?
This illness can sometimes precede the development of pericoronitis, and the article concludes that 43% of patients with pericoronitis had a cold prior to the infection.
Is pericoronitis a complication of wisdom teeth?
Rest assured that pericoronitis is a common complication related to wisdom teeth, and your dentist can guide you toward the best treatment option for you. This article is intended to promote understanding of and knowledge about general oral health topics.
What is the best treatment for pericoronitis?
Prosthodontist. Oral surgeon. Treatments for pericoronitis include: Oral hygiene/oral irrigators and rinses: If the pericoronitis is in a small area and hasn’t spread, treatment may be rinsing your mouth with warm salt water. Your dentist can flush out food debris or bacteria, or give you an oral rinse.
What is the diagnosis of pericoronitis?
Pericoronitis Diagnosis. Your dentist will examine your wisdom teeth to see how they are coming in, and determine if they are partially erupted. They may take an X-ray periodically to determine the alignment of the wisdom teeth.
How do you know if you have pericoronitis?
Symptoms of pericoronitis can be either acute (short-term) or chronic (be ongoing). Acute symptoms include: Pain. Swelling in the gum tissue (caused by an accumulation of fluid) Pus discharge. Trismus, or difficulty opening your mouth and jaw, also called lockjaw. Pain with swallowing. Fever.
How to treat pericoronitis?
How you treat pericoronitis depends on how severe it is. In the most mild of cases, you might see some relief by rinsing out your mouth with saline or a mouthwash. If the infection is more severe, your dentist might prescribe antibiotics to clear it up. A pain reliever that also reduces swelling, such a ibuprofen, can also help improve your comfort.
What causes pericoronitis?
What Causes It. Pericoronitis occurs when a tooth only comes in part way and when a portion of gum tissue is left over the tooth. The gum tissue often has an opening that is the perfect place for food to become lodged and for bacteria to accumulate. The bacteria are what are responsible for the infection. As they multiply, the gum becomes more and ...
Where does pericoronitis occur?
Although pericoronitis can develop on either side of the mouth or on the top or bottom rows, it’s more common on the bottom row.
Can you get pericoronitis if you have wisdom teeth?
The good news is that once your wisdom teeth are gone, the risk for recurring pericoronitis drops significantly. It’s rare for a person to have a recurring infection once the wisdom teeth are taken out and the gum flap repaired.
What is the medical term for pericoronitis?
What is the medical definition of pericoronitis? Pericoronitis is inflammation of the gum tissue surrounding the crown portion of a tooth. Pericoronitis usually affects the lower third molar (wisdom tooth) where gum tissue overlaps the chewing surface of the tooth. Pericoronitis can be either chronic or acute.
How long does pericoronitis last?
With timely care and treatment, pericoronitis can properly be managed or eliminated. Symptoms of pericoronitis can last for days to weeks depending on the severity. The condition should resolve in approximately one to two weeks with treatment.
What are the risk factors for pericoronitis?
Risk factors for pericoronitis include the presence of excess gum tissue (operculum) overlying the wisdom tooth and difficult access to the wisdom teeth for proper cleaning.
What is the difference between periodontal disease and pericoronitis?
Pericoronitis is differentiated from periodontal disease (or periodontitis) in that it occurs specifically around a partially erupted tooth where the tooth has not completely emerged from the gum overlying it.
How do you know if you have pericoronitis?
Signs and symptoms of pericoronitis can range from mild to severe and include. pain, swelling of the gums, tenderness, redness of gum tissue, bad breath ( halitosis ), bad taste from pus, difficulty opening the jaw (trismus), difficulty swallowing ( dysphagia ),
What kind of doctor can treat gum infection?
In situations where surgery is required or if it is a severe and complicated case, dental specialists such an oral surgeon or a periodontist (gum surge on) can provide treatment. In very rare instances, should the infection become more widespread, emergency services with physician care might be needed.
Can pericoronitis spread to the head?
Complications can occur with pericoronitis. Although rare, the infection can spread from the mouth into the head and neck and cause a serious complication called "Ludwig's angina .".
Why does pericoronitis occur?
It develops when the molar becomes partially impacted due to bacteria accumulation. Typically, the tooth is only partially exposed (partial eruption), and excess gum tissue overlaps the tooth. Pericoronitis is a type of gingivitis. It develops around teeth as they are erupting out of the gums. Pericoronitis happens when ...
How long does it take for pericoronitis to resolve?
The prognosis for pericoronitis is very good after treatment is complete. The condition typically resolves in about one to three weeks (depending on the patient). Pericoronitis can return if the original infection that caused the condition is not treated.
How do you know if you have pericoronitis?
Symptoms of Pericoronitis. The symptoms associated with pericoronitis vary based on the severity of the infection. Milder pericoronitis cases are referred to as acute pericoronitis, symptoms include: Painful, swollen gum tissue near the erupted tooth. Difficulty biting down in the area without hitting the swollen tissue.
What is the best treatment for wisdom tooth pericoronitis?
You can take over-the-counter pain medication like acetaminophen, ibuprofen, or pain relievers that your dentist prescribes. The next step in treatment depends on your wisdom tooth’s status.
What are the symptoms of pericoronitis?
Bad breath or halitosis. Loss of appetite. The symptoms associated with more severe cases of pericoronitis: Swelling of the face. Swollen lymph nodes. Jaw spasms. Trismus, more commonly referred to as “lockjaw”. Numbness or tingling of the face.
Does pericoronitis go away on its own?
Pericoronitis will not go away on its own. It is essential to treat the condition immediately and properly before any chronic symptoms and conditions arise. Contact your dentist as soon as you start noticing any symptoms of pericoronitis.
Can pericoronitis spread into the bloodstream?
It is also associated with other deep infections in the neck, throat, and head. There is also the risk that pericoronitis can spread into the bloodstream. This life-threatening condition is known as sepsis. If you develop any symptoms of sepsis, seek emergency medical care immediately.
How long does it take for pericoronitis to heal?
Usually, the symptoms of pericoronitis can be relieved with conservative treatment in about one week. However, if the tooth is partially impacted and food and bacteria keep building up under the gum, pericoronitis will more than likely return.
How do you know if you have pericoronitis?
Symptoms of pericoronitis can include: Pain. Swollen gum tissue in the area of the affected tooth. It can be difficult to bite down comfortably without catching the swollen tissue between your teeth. It can progress to become a knob-like mass of tissue that is very painful when you chew or open and close your mouth.
What causes pericoronitis in wisdom teeth?
Generally, a pericoronitis infection will be caused by: Gum flap infection. In case of a partially erupted wisdom tooth, part of the tooth is exposed, but part of it remains covered by a flap of gum tissue. Food particles and other debris may get trapped under this flap of gums and cause an initial inflammation.
Can pericoronitis spread into surrounding tissues?
In severe cases of pericoronitis the infection may spread into surrounding tissues, developing to cellulitis, a very serious, often life-threatening infection that must be treated quickly to prevent further spread and possible swelling of the airway.
Can wisdom teeth be affected by pericoronitis?
Pericoronitis may affect any tooth that has eruption problems and becomes impacted, but since impaction is a very rare condition in the rest of the teeth, it most often occurs with the wisdom teeth, most common ly those of the lower jaw . Pericoronitis is a main cause of wisdom tooth pain.
How do you know if you have pericoronitis?
What are the symptoms of Pericoronitis? Milder symptoms of pericoronitis include painful, swollen gum tissue near the affected tooth. You may find it hard to bite down in that area without hitting the swollen tissue . You may also notice an unpleasant smell or taste in your mouth, and a discharge of pus in the area.
Can pericoronitis affect swallowing?
These are signs of a spreading infection into the throat and neck, which could affect your ability to breathe and swallow, and could be life-threatening. For this reason, if you notice the early signs of pericoronitis, it’s important to contact your dentist immediately.
Can pericoronitis recur?
Sometimes, pericoronitis develops near a tooth that is still in the process of erupting, which will continue to come in normally. In that case, your dentist will monitor the area to ensure that it stays clean and infection does not recur, until the tooth has fully come in.
What is the best medication for pericoronitis?
Over-the-counter medications, such as ibuprofen (Advil) or acetaminophen (Tylenol), can be used to manage the pain caused by acute pericoronitis.
What causes pericoronitis?
Bacteria accumulation is the main cause of pericoronitis. When the tooth is partially erupting and still has much gingiva covering it, food debris and bacteria may get trapped in-between the erupting tooth and the overlapping gum tissue. Pericoronitis begins with an inflammation of the flap of the overlapping gingival tissue (operculum).
What is the term for an abscess under the operculum?
Pericoronitis begins with an inflammation of the flap of the overlapping gingival tissue (operculum). This is known as operculitis. Operculitis leads to the formation of an abscess under the operculum, which develops into the pericoronal infection (pericoronitis). Pericoronitis, if left untreated, can radiate to other parts of the mouth.
How do you know if you have pericoronitis?
The signs and symptoms of pericoronitis include: Halitosis (bad breath) Bad taste as a result of oozing pus, Trismus (difficulty in opening your jaw), Dysphagia (difficulty in swallowing), Feeling unwell. Fever, Loss of appetite, Pain,
Can a dentist treat pericoronitis?
Pericoronitis can be treated by any licensed dentist. However, in cases where surgery is required to treat the gum tissue infection or if the pericoronitis is a complicated or severe one, dental professionals such as a periodontist (gingival surgeon) or an oral surgeon would be required to handle the treatment.
Is pericoronitis a chronic infection?
This gum tissue infection can either be acute or chronic. Acute pericoronitis is associated with pain, swelling, and fever, which indicate that the bacterial infection is radiating. Chronic pericoronitis is associated with mild constant inflammation in the affected area . Pericoronitis mostly affects teenagers and young adults.
Is pericoronitis the same as periodontitis?
Pericoronitis is not the same as periodontitis in that pericoronitis occurs exactly around a tooth that is just erupting, where the tooth has not fully erupted from the gum covering it.