
Percutaneous transluminal angioplasty, stenting and atherectomy are minimally invasive (endovascular) procedures that restore blood flow when arteries are clogged due to peripheral artery disease. Stenting, in which a tube is placed in the artery to hold it open, is often part of the angioplasty procedure.
What is percutaneous (endovascular)?
Percutaneous adult congenital heart disease treatment - ASD and PFO. Percutaneous ventricular assist device placement. Endovascular aortic stenting. Endoscopic lead placement for defibrillator or pacemaker devices. Endoscopic radial artery and saphenous vein harvesting for bypass surgery.
What is endovascular treatment for peripheral artery disease?
Percutaneous transluminal angioplasty, stenting and atherectomy are minimally invasive (endovascular) procedures that restore blood flow when arteries are clogged due to peripheral artery disease. Stenting , in which a tube is placed in the artery to hold it open, is often part of the angioplasty procedure.
What are the treatment options for complex endovascular conditions?
Apr 24, 2015 · Advances in endovascular therapies during the past decade have broadened the options for treating peripheral vascular disease percutaneously. Endovascular treatment offers a lower risk alternative to open surgery in many patients with multiple comorbidities.
What is endovascular surgery?
Jun 03, 2021 · Endovascular surgery is a procedure that is performed using minimally invasive catheter techniques on the arteries or veins. Procedures include aneurysm repair, grafts, stents, varicose vein repair, and more. Endovascular surgery is often performed on an outpatient basis.
What is percutaneous endovascular therapy?
What is endovascular catheterization?
What angioplasty means?
What is the purpose of a percutaneous transluminal coronary angioplasty?
What is the difference between endovascular and vascular surgery?
Where are endovascular procedures performed?
What is the difference between angiogram and angioplasty?
What happens if 3 arteries are blocked?
How many years a person can live after angioplasty?
Is PTCA open-heart surgery?
Is PCI and PTCA same?
What are the complications of PTCA?
- Bleeding at the catheter insertion site (usually the groin, but the arm may be used in certain circumstances)
- Blood clot or damage to the blood vessel at the insertion site.
- Blood clot within the vessel treated by ptca/stent.
What is a percutaneous transluminal angioplasty?
Percutaneous transluminal angioplasty, in which a balloon inside the artery inflates at the site of a fatty clog to press it against the artery walls, allows the blood to flow again. Percutaneous transluminal angioplasty, stenting and atherectomy are minimally invasive (endovascular) ...
What are the treatments for peripheral artery disease?
Other treatments for peripheral artery disease include diet, exercise and medication to combat atherosclerosis, and open bypass surgery.
What is a transluminal angioplasty?
Percutaneous transluminal angioplasty is a minimally invasive procedure used to open a blocked artery. Your physician will follow this procedure:
What is the procedure called when a tube is placed in the artery to hold it open?
Stenting, in which a tube is placed in the artery to hold it open, is often part of the angioplasty procedure.
What is the process of removing plaque from a blockage?
Atherectomy is the process of de-bulking — removing some of the plaque from a blockage. If performed, it takes place just before the angioplasty balloon is used. There are several different types of ather ectomy procedures. Rotational atherectomy .
How successful is percutaneous AAA repair?
Haas et al performed 13 procedures with 100% success using the percutaneous technique with devices ranging from 16 F to 22 F.1 Torsello et al performed a randomized prospective study evaluating percutaneous EVAR to femoral artery exposure and noted the length of stay and time to ambulation was significantly shorter in the percutaneous group.2 More recently, Morasch et al evaluated percutaneous AAA repair versus AAA repair and femoral artery exposure. His study included 47 patients who had undergone percutaneous AAA repair and 35 patients who had undergone FAC EVAR. The Gore Excluder device was used in all patients for EVAR, and they were able to successfully complete a percutaneous repair in 93%. Average blood loss in their percutaneous group was 459 mL, and the average length of stay was 1.49 days.3 Our initial results were comparable to those of Morasch et al, and we have used three different devices for EVAR. Krajcer et al have performed percutaneous AAA repair for years and have performed the procedure under local anesthesia and conscious sedation.4
What is evar repair?
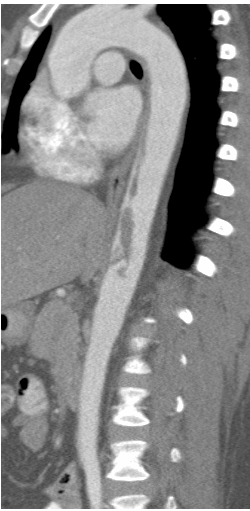
Endovascular aortic aneurysm repair (EVAR) is increasingly popular as a durable option for aor tic aneurysm repair given appropriate anatomy. Vascular access for EVAR is typically performed with bilateral femoral artery exposure. Complications for femoral artery exposure in the setting of EVAR are not uncommon and include hematoma, infection, and seroma. The evolution and development of techniques used in the performance of EVAR have continued throughout its development. Currently, we repair approximately 70% to 80% of aneurysm patients with EVAR using a variety of devices. The diagnostic imaging workup utilizes a single CT scan followed by Preview 3-D reconstruction (Medical Metrx Systems [MMS], Lebanon, NH). As a result of our experience with suture-based closure devices in other percutaneous procedures, we initiated a percutaneous closure algorithm for EVAR patients. With adequate attention to femoral anatomy and precise positioning of point of access in the femoral artery, percutaneous closure of sheath sizes up to 24 F (outer diameter) have been achieved routinely, resulting in essentially no postoperative pain.
Is percutaneous AAA repair feasible?
Our initial results demonstrate that percutaneous AAA repair is feasible if the patient has been adequately evaluated preoperatively. Our protocol stresses two critical factors: (1) careful preoperative imaging of the femoral arteries, and (2) precise positioning of the access using a micropuncture technique.
Can evar be performed with a high degree of success?
Percutaneous EVAR can be performed with a high degree of success.
Is AAA repair a sedation procedure?
Percutaneous AAA repair is an attractive option in patients with hostile abdomens (Figure 5) in which even femoral artery exposure can be quite difficult and fraught with high complication rates (Figure 6). This technique also makes the EVAR procedure more amenable to performance under conscious sedation because the amount of local anesthesia needed is small and there is essentially no postoperative pain. Postoperatively, these small stab incisions are the only wounds that need to be closed, and in our experience, all of the patients were without discomfort on postoperative day 1 (Figure 7).
What is endovascular surgery?
Endovascular surgery is an innovative, less invasive procedure used to treat problems affecting the blood vessels, such as an aneurysm, which is a swelling or "ballooning" of the blood vessel. The surgery involves making a small incision near each hip to access the blood vessels.
What are the complications of endovascular surgery?
As with any procedure, endovascular surgery does have potential complications, which may include: 1 Blockage of the blood flow through the graft 2 Fever and an increase in white blood cell count shortly after the surgery 3 Graft fracturing 4 Infection 5 Leaking of blood around the graft 6 Movement of the graft away from the targeted position
How to determine if aneurysm is endovascular?
To determine whether your aneurysm can be treated with endovascular surgery, you will have tests, including a CT scan and angiography, which allow your doctor to view your aorta and blood vessels. These tests also allow the doctor to select the appropriate size graft.
What tests are done before endovascular surgery?
You also may have tests to determine the health of your heart, such as a stress test and an electrocardiogram (ECG), which records the electrical activity of the heart.
What is the procedure for aneurysms?
Before the procedure begins, you will have either a sedative and regional anesthesia to make you more comfortable and numb the area of operation, or general anesthesia that will put you to sleep completely. The area of insertion will be cleaned and shaven to prevent infections. Your doctor will make a small incision around the hip, near the crease between the hip and thigh, to access your blood vessels. A guide wire is inserted through the incision and a pushed through a blood vessel to the aneurysm.
Is endovascular surgery better than general anesthesia?
An alternative to open surgery, endovascular surgery offers many advantages, including a shorter recovery period, less discomfort, local or regional anesthesia instead of general anesthesia, smaller incisions, less stress on the heart and fewer risks for patients with other medical conditions. This procedure may benefit patients who need surgery but are at a high-risk of complications because of other conditions.
Is endovascular surgery feasible?
Advanced Endovascular Procedures. In some cases, standard endovascular repair is not always feasible for patients. Sometimes the aneurysm is too close to important branches of the aorta or the arteries are too narrow or too complicated to permit passage of the catheter used in endovascular surgery. In these cases, the patient has three options: no ...
What is endovascular surgery?
Endovascular surgery is a procedure that is performed using minimally invasive catheter techniques on the arteries or veins. Procedures include aneurysm repair, grafts, stents, varicose vein repair, and more. Endovascular surgery is often performed on an outpatient basis.
What is the procedure to repair an aneurysm in the aortic wall?
Surgery is done to repair the aneurysm in the aortic wall, the aneurysm is removed and replaced by an artificial blood vessel (a man-made tube comprised of synthetic material).
What is the difference between open surgery and general anesthesia?
Open Surgery. A local or regional anesthesia is used to numb the local area. General anesthesia is administered to induce sleep. A very small incision is made near each hip (to access the blood vessels). A large incision is made in the side of the chest or breastbone (for a thoracic aneurysm) to see the aorta in full view.
Where is the catheter placed for aneurysm surgery?
A catheter is placed into the blood vessels in the hip and threaded through to the aorta . The aorta is clamped in an area above and below the aneurysm to stop the bleeding during surgery. A special fabric tube called an endovascular graft is inserted through the arteries (inside the catheter) and positioned in the aorta.
Is endovascular surgery a risk?
Just as with any other type of surgery, endovascular procedures pose a risk of potential complications, these include:
What is a percutaneous valve replacement?
A percutaneous valve replacement is a minimally invasive procedure to replace a diseased heart valve. The malfunctioning valve is removed and replaced with a manufactured valve, which may be mechanical. Other valve replacements may be crafted from animal tissue, or human tissue harvested from the patient’s own membrane enveloping the heart (pericardium).
What is balloon valvuloplasty?
Percutaneous balloon valvuloplasty is widely performed to dilate the mitral valve, but other procedures are in testing and clinical trial phases. Percutaneous mitral valve repair has been performed only in clinical trials, while percutaneous replacement is yet to be performed on humans.
Can aortic valve replacement be performed percutaneously?
Currently, only aortic and pulmonary valve replacements are performed percutaneously. Only valve repairs and dilatation are percutaneously performed in the mitral and tricuspid valves. Percutaneous valve replacement is performed to treat the following conditions:
Is tricuspid valve repair under clinical trials?
At present percutaneous tricuspid valve repair procedure is under clinical trials and valve replacement is in early stages of development.
Can a heart valve be repaired?
Heart valves that are diseased can be treated both surgically (traditional heart valve surgery) and non-surgically (balloon valvuoplasty). The mitral valve is the most commonly repaired heart valve, but the aortic, pulmonic, and tricuspid valves may also undergo some of these repair techniques.
What is endovascular surgery?
Endovascular procedures are performed by a variety of operators from different specialties including vascular surgeons, interventional radiologists and cardiologists, vascular medicine specialists, and some cardiovascular surgeons. Despite consensus guidelines for diagnosis and treatment of PAD, each specialty has its own specific recommendations for the required volume of cases and acquired knowledge to treat vascular disease. 35 – 37 Although progress in other vascular areas such as carotid disease have been made, few evidenced-based disease-specific guidelines (claudication versus CLI) are available for lower extremity PAD. 38, 39
What is the endovascular procedure for PAD?
Collectively, endovascular procedures for PAD have evolved and require not only technical skills, but also a full knowledge of all treatment options such as surgical, hybrid (combined surgical and endovascular procedures), and endovascular procedures. In addition, treating PAD and CLI requires a solid knowledge of noninvasive vascular testing, differential diagnosis of leg pain and lower extremity ulcers, risk and complications associated with all treatment options, and a full set of endovascular skill sets including the ability to recognize and manage procedural complications. These are all required so that optimal, personalized treatment can be offered to each patient. 20
What are the treatments for peripheral artery disease?
Percutaneous therapies for peripheral artery disease continue to evolve with new techniques and devices. Although guidelines-recommended therapies have impacted cardiovascular morbidity and mortality, endovascular interventions have been shown to reduce limb pain, improve quality of life, and prolong walking distance for those with claudication and to reduce amputation rates among those with critical limb ischemia. Novel devices such as drug-eluting stents and drug-coated balloons have improved patency for moderate-length lesions, whereas others allow treatment of heavily calcified and tortuous segments. New adjunctive devices to cross lesions and reduce or modify associated plaque have also been developed, although level 1 data regarding their efficacy are sparse. There has also been a better mechanistic understanding of lower extremity endovascular treatment using tools such as intravascular ultrasound. This information has highlighted the need for better stent size selection for the femoropopliteal arterial segments and larger balloon diameters for the tibial arteries. Moreover, a wound perfusion approach with direct in-line flow, the so-called angiosome approach, and reconstruction of the pedal loop have been advocated for improved wound healing. Technical advances such as the tibiopedal access and reentry methods have allowed crossing of lesions that were considered no option for the endovascular approach in the past. Collectively, there has been increased awareness, interest, and commitment by various specialty societies and organizations to advance the treatment of peripheral artery disease and critical limb ischemia. This is also evident by the recent coalition of 7 professional societies and organizations that represented >150 000 allied health professionals and millions of patients with peripheral artery disease at the 2015 Centers for Medicaid and Medicare Services Medicare Evidence Development and Coverage Analysis Committee meeting. The percutaneous therapies for peripheral artery disease continue to evolve with longer follow-up with randomized data and larger prospective registries. In the future, it is hopeful that we will treat the lower extremity arteries according to segments, taking into account plaque morphology, luminal versus subintimal crossing, location, and stenotic versus occlusive disease. Until then, we must identify the most cost-effective, efficacious, and safe treatment for each patient. The goal of this article is to aid the practicing vascular specialist consider the optimal choices for the management of patients with vascular disease.
What is PAD in aorta?
PAD affects the aorta, common, external and internal iliac, common femoral and profunda, superficial femoral, popliteal, infrapopliteal (anterior tibial, posterior tibial, peroneal), and intrinsic pedal arteries. In general, individuals with claudication have significant in-flow disease (aortoiliac, common femoral artery [CFA]) and femoropopliteal disease. Ischemic rest pain is typically associated with at least 2-level disease and is often relieved once inflow disease has been addressed. Tissue loss, however, is associated with multilevel disease with a significant proportion of patients having infragenicular tibial and intrinsic pedal artery disease. 24 The technical expertise required, the devices used, and the patency for each segment are different and depend on the degree of stenosis or occlusion, lesion length, calcification, and clinical presentation. The main challenges for endovascular therapies continue to involve the CFA, distal superficial femoral and popliteal, and tibial and plantar arteries.
What is endovascular intervention?
The main goal of endovascular intervention for CLI, unlike claudication, is to relieve rest pain, heal ischemic ulcers, and prevent amputation. In these patients, end points including amputation-free survival and major adverse limb events (MALEs), which include above-ankle amputation of the index limb or major reintervention (defined as new surgical bypass graft, jump or interposition graft revision, thrombectomy or thrombolysis), have been suggested. 18, 19 However, these end points fail to capture other important outcomes such as recurrent hospitalization for infection, pain control, endovascular reintervention, and impaired quality of life ( Figure 1 ). 20, 21 Because of these limitations, it is our belief that a renewed focus on complete wound healing, rates of wound healing, and time to wound healing may be a step forward for this field beyond amputation-free survival, MALE, and MALE plus perioperative death within 30 days. 20, 22 To this end, time to wound healing was recently shown to predict MALE, major amputation, and mortality in patients undergoing endovascular therapy for CLI ( Figure 2 ). 23 Indeed, the incremental value of current interventions is relatively small, and few interventions for CLI to date have shown a reduction in amputation rates. Therefore, time to wound healing may serve as an important end point to conduct comparative effectiveness trials among various techniques and endovascular strategies for CLI. However, given the heterogeneity of wound size, depth, and locations, better baseline assessment tools are required for a more balanced comparisons. We would suggest primary end points that would encompass MALE in combination with objective assessments of wound healing and pain relief (based on relevancy for the patient), and periprocedural complications.
What is PAD in claudication?
PAD, defined by the Rutherford class, may present as asymptomatic (or having atypical features) or as the common symptom, claudication (Rutherford I–III). Patients with the more advanced form, CLI, present with ischemic rest pain, tissue loss, or gangrene (Rutherford IV–VI). Endovascular therapy has been recommended for patients with lifestyle-limiting (or disabling) claudication and for individuals with CLI. 2, 3, 10 Because of the different presentations (claudication versus CLI), different end points have been included in clinical trials, making comparisons of technologies challenging. For claudication device trials, primary patency has been the gold-standard end point, largely defined by regulatory agencies to support the notion that the treatment is safe and effective in restoring arterial perfusion through the treated segment. More recently, the combination of patency and clinically driven target lesion revascularization has gained momentum as a more relevant end point for treating patients with claudication. 11, 12 Other important end points include secondary patency, assisted primary patency, and quality-of-life metrics such as the Walking Impairment Questionnaire, the Short-Form-36 Physical Functioning Score, 13 the Peripheral Artery Questionnaire, 14 and the PAD Quality of Life Questionnaire. 15 However, given that the majority of patients are treated with endovascular therapy to improve pain-free walking distances (time), objective evidence of improving these parameters is most important. 5, 16 Treadmill exercise testing may allow objective assessment of the functional efficacy of available endovascular treatments beyond patency and quality-of-life questionnaires. 5, 16 Because many centers do not routinely perform objective treadmill exercise testing, use of the standardized 6-minute walk test has recently been adopted in claudication trials. 17
Is endovascular strategy based on literature?
The subsequent sections provide suggested endovascular strategies based on literature. However, there are scenarios in which clinical practice has advanced faster than publication of peer-reviewed data. In those cases, we suggest alternate strategies; however, these are not based on literature, and many devices are used off-label by practitioners who feel that these strategies are best for their patients. We are not endorsing any specific category or device.
What is a percutaneous transcatheter?
Percutaneous transcatheter treatment is one type of therapy for deep venous thrombosis (DVT). DVT is a blood clot that forms in a large vein deep in the body. It happens most often in a leg. The procedure uses a thin, flexible tube called a catheter to help remove the blood the clot. During the treatment, a healthcare provider will insert ...
How does a percutaneous clot procedure work?
Percutaneous means that the procedure is done through a small puncture in the skin instead of a large incision.
How to break up a DVT?
Your healthcare provider might use one of several types of percutaneous transcatheter treatments. The catheter may be used to send clot-dissolving medicine to the DVT. This can help break up the clot. Or, your healthcare provider might use small tools to help break up the clot. In some cases, a tiny balloon or metal, mesh coil (stent) is inserted in the vein to help hold it open.
What is the tube used for a blood clot?
For example, it might carry clot-dissolving medicine. It may have a tiny deflated balloon or other device attached. The tube will be threaded through the blood vessel all the way to the site of the blood clot. Continuous X-ray images may be used to show exactly where the tube is.
What tests are needed for DVT?
You may need some tests before the procedure, such as: Ultrasound, to measure blood flow in the leg and help diagnose DVT. Venogram, to get an image of your veins and the blood clot. Computed tomography (CT) scan, to get more information about the blood clot.
Can you stop taking blood thinners before surgery?
You may need to stop taking some medicines ahead of time, such as blood thinners. If you smoke, you’ll need to stop before your procedure.
Can a transcatheter be used for post thrombotic syndrome?
Want to decrease the risk of post-thrombotic syndrome. Transcatheter treatment is not the only kind of treatment for a blood clot. You must have specific clinical factors to be a candidate for this procedure. Many people with blood clots are treated with medicines called blood thinners.
What does PVD mean in surgery?
Requires harvesting of saphenous veins and upper extremity veins, precluding their use for coronary artery bypass. PVD = peripheral vascular disease. Surgical bypass of severely occluded vessels has been considered the gold standard for use in symptomatic patients who do not respond to more conservative treatments.
Which artery is the easiest to approach percutaneously?
The iliac arteries are technically among the easiest vessels to approach percutaneously and are the largest peripheral lower extremity vessels with the highest flow rates. These factors optimize the outcome of percutaneous transluminal angioplasty (PTA) and stenting ( Table 2). Surgical bypass has a durable high rate of patency, reported as 93 percent at 42 months in a recent study, 8 but it is a major surgical procedure with potential for systemic complications in patients with preexisting significant comorbid conditions.
How do you diagnose peripheral vascular disease?
The primary care physician can easily identify patients who are at risk for the disease with a questionnaire and a relatively simple test— the ankle brachial index. More than 70 percent of patients diagnosed with the disease remain stable or improve with conservative management. Those who do not improve may undergo contrast angiography or magnetic resonance angiography, which may be used in planning for surgery or percutaneous intervention. Surgical bypass is the gold standard for extensive vascular occlusive disease, but endovascular interventions, including percutaneous transluminal angioplasty and stent placement, are being used more frequently, particularly in patients with significant comorbid conditions.
How many people are affected by peripheral vascular disease?
Based on incidence rates extrapolated to today's increasingly aging population, PVD affects as many as 10 million people in the United States. 1 As the population ages, the family physician will be faced ...
Is metallic stent better than PTA?
The introduction of metallic stents has improved outcome in patients in whom PTA results were suboptimal. This technique has also opened the way for percutaneous treatment of complex, long-segment stenoses and occlusions, and the treatment of aortic bifurcation occlusive disease. Initial technical success of stent placement in aortoiliac occlusive disease is 96 percent, higher than that of PTA alone ( Figure 2). 9 Primary patency rates are 63 percent, and secondary patency rates are 86 percent at five years, respectively, approaching that of surgical bypass. 12
Is aortic bifurcation reconstruction performed percutaneously?
Aortic bifurcation reconstruction, once the sole realm of surgical bypass, is now performed successfully using percutaneous techniques. In one study 12 that used bilateral iliac stents for treatment of aortic bifurcation disease with at least 12 months of follow-up, primary and secondary angiographic patency rates were attained in 89 and 93 percent of 28 patients, respectively—again approaching that of surgical bypass. 13
Is PVD considered an occlusive disease?
For purposes of revascularization, PVD is considered in terms of inflow (aortoiliac) and outflow (infrainguinal) occlusive disease. In both cases, surgical revascularization represents the gold standard against which the results of percutaneous revascularization with angioplasty and stents are compared.
