What does PCI stand for in heart?
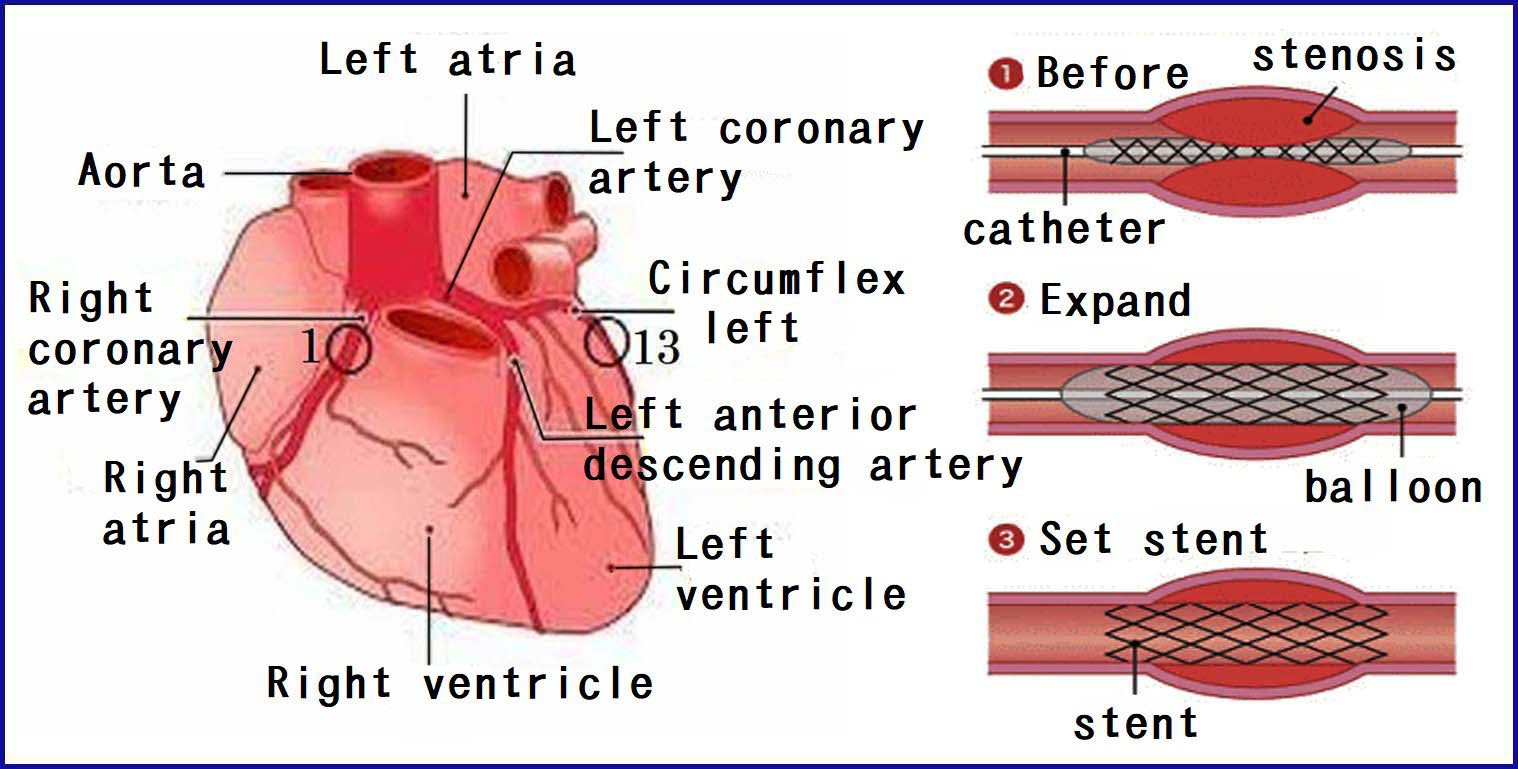
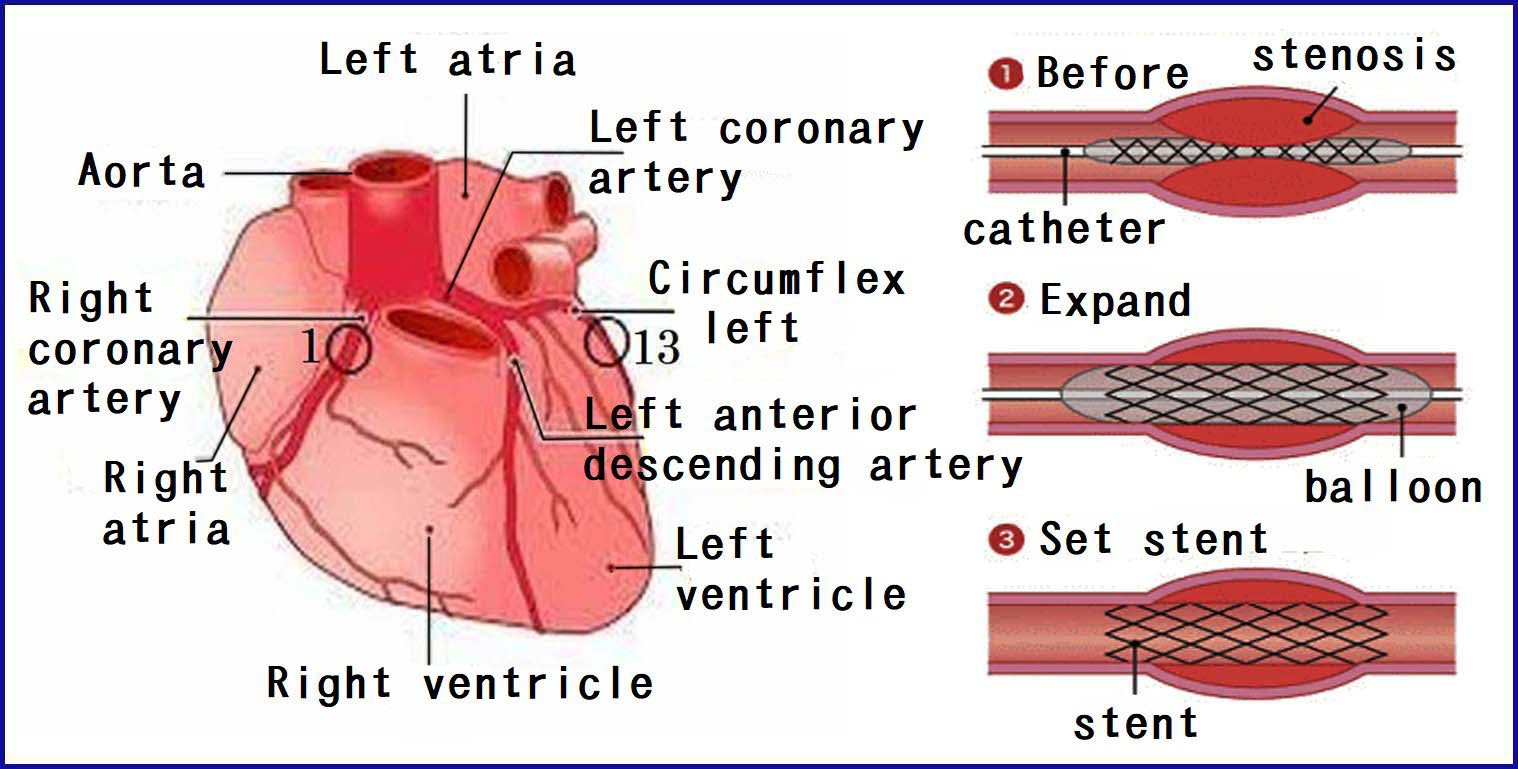
Percutaneous coronary intervention (PCI) is a treatment to open a blocked artery. Arteries are the blood vessels that carry oxygen-rich blood through your body. You may need a PCI if you have a buildup of a fatty, waxy substance (plaque) in your arteries. Or you may have a PCI to clear blockages after a heart attack.
What is a PCI heart procedure?
Percutaneous coronary intervention (PCI) refers to a family of minimally invasive procedures used to open clogged coronary arteries (those that deliver blood to the heart). By restoring blood flow, the treatment can improve symptoms of blocked arteries, such as …
What does PCI stand for in cardiology?
Percutaneous Coronary Intervention (PCI, formerly known as angioplasty with stent) is a non-surgical procedure that uses a catheter (a thin flexible tube) to place a small structure called a stent to open up blood vessels in the heart that have been narrowed by plaque buildup, a condition known as atherosclerosis.
What is cardiac PCI procedure?
Jul 31, 2015 · Percutaneous Coronary Intervention or PCI (also called Percutaneous Transluminal Coronary Angioplasty or PTCA) is a medical procedure in which a balloon is used to open a blockage in a coronary artery narrowed by atherosclerosis. This procedure usually involves placement of stents to improve the blood flow to the heart.
Is PCI and stent the same?
Percutaneous Coronary Intervention (PCI, formerly known as angioplasty with stent) is a non-surgical procedure that uses a catheter (a thin flexible tube) to place a small structure called a stent to open up blood vessels in the heart that have been narrowed by plaque buildup, a condition known as atherosclerosis.
How long does a PCI procedure take?
Patients also may experience brief episodes of angina while the balloon is inflated, briefly blocking the flow of blood in the coronary artery. The percutaneous coronary intervention procedure can last from 30 minutes to two hours, but is usually completed within 60 minutes.
How long do you stay in hospital after PCI?
Stable elective PCI cases can be typically monitored for 6 hours then sent home with no significant risk of complications beyond those that could occur over 24 hours and beyond.Aug 5, 2019
Why is PCI done?
The main goal of PCI is to open up clogged arteries, but there are different ways your doctor can do that. PCI types include: Balloon angioplasty. A balloon is inserted and inflated in your artery to press plaque out of the way.Oct 21, 2021
What are the complications of PCI?
Complications can include:Injury to the heart arteries, including tears or rupture.Infection, bleeding, or bruising at the catheter site.Allergic reaction to the dye or contrast used.Kidney damage from the dye or contrast.Blood clots that can lead to stroke or heart attack.More items...
How much blockage requires a stent?
“Patients typically develop symptoms when an artery becomes narrowed by a blockage of 70 percent or more,” says Menees. “Most times, these can be treated relatively easily with stents. However, with a CTO, the artery is 100 percent blocked and so placing a stent can be quite challenging.”Jul 18, 2017
How long can you live after stents?
Survival was 99.5% at 1 year and 97.4% after 5 years; "event free survival" was 84.6% at 1 year and 65.9% after 5 years; "ischemia free survival" was 84.6% at 1 year and 44.8% after 5 years.
How is life after stent in heart?
It generally takes most people a couple of weeks to start returning to their normal activities after angioplasty/stenting. Before you leave hospital, you'll be given detailed instructions for exercise, medications, follow-up appointments, ongoing wound care and resuming normal activities.
Can you live a normal life after a stent?
It's important to remember that you can live a full and active life with a coronary stent. You can find some general guidelines about returning to working, resuming your everyday activities and making some heart-healthy lifestyle changes below.
When is PCI recommended?
Primary PCI is only indicated when symptoms duration is 12-24 hours (delayed presentation) if severe congestive heart failure, hemodynamic/electrical instability or continued angina is present. Primary PCI is not recommended when symptom onset is more than 12 hours and the patient is asymptomatic (OAT trial).
What is the difference between CABG and PCI?
All comparisons of CABG to PCI or medical therapy that demonstrate survival effects with CABG also demonstrate infarct reduction. Thus, CABG may differ from PCI by providing "surgical collateralization," prolonging life by preventing myocardial infarctions.Mar 5, 2019
What is the difference between PCI and cardiac catheterization?
Cardiac catheterization or “cardiac cath” and percutaneous coronary intervention (PCI) are minimally-invasive medical procedures used to help diagnose and treat conditions of the heart and blood vessels. You may need a cardiac cath or PCI to: Determine if you have a disease of the heart, blood vessels or heart valves.
Why do we need PCI?
Why is it done? PCI improves blood flow, thus decreasing heart-related chest pain (angina), making you feel better and increasing your ability to be active. PCI is usually scheduled ahead of time.
What is IV line?
An intravenous (IV) line is inserted so, if necessary, you can be given medications quickly. Electrodes will be placed on your body to monitor your heart, and a small device called a pulse oximeter may be clipped on a finger or ear to track the oxygen level in your blood.
How does a catheter work?
Using a special type of X-ray called fluoroscopy, the catheter is threaded through the blood vessels into the heart where the coronary artery is narrowed. When the tip is in place, a balloon tip covered with a stent is inflated. The balloon tip compresses the plaque and expands the stent. Once the plaque is compressed and the stent is in place, ...
How long do you have to stay flat after a catheter is inserted?
You will need to remain lying flat during this time. If the catheter was inserted in the groin, you will have to keep your leg straight for several hours. If it was inserted in the arm, your arm will be kept elevated on pillows and kept straight with an arm board.
How is balloon angioplasty done?
Balloon angioplasty employs a deflated balloon-tipped narrow catheter that is inserted through the skin of the groin or arm into an artery. The catheter is threaded through the artery until it arrives in the coronary artery where there is narrowing or blockage. The catheter tip is then inserted through the narrowed area.
When is a stent inserted?
It is inserted into a coronary artery usually just after an angioplasty has been done to open the vessel. The stent slowly releases the drug with which it is coated. The drug may, for example, be sirolimus.
What is a stent used for?
A stent is an extendable metal scaffold that can be used to keep open previously narrowed coronary arteries after angioplasty has been performed. The mechanism used to place the stent in a narrowed or blocked coronary artery is very similar to balloon angioplasty. The difference is that the un-extended or collapsed stent surrounds the balloon.
Why are stents important?
Stents are useful because they keep the coronary artery open when the balloon is deflated, preventing most arteries from narrowing again (termed elastic recoil) after the balloon is deflated. Recurrent narrowing (restenosis) sometimes may still occur after the stent is placed due to formation of scar tissue.
What is a PCI?
The American College of Cardiology/American Heart Association (ACC/AHA) Task Force on Practice Guidelines was formed to gather information and make recommendations about appropriate use of technology for the diagnosis and treatment of patients with cardiovascular disease. Percutaneous coronary interventions (PCI) are an important group of technologies in this regard. Although initially limited to PTCA, and termed percutaneous transluminal coronary angioplasty (PTCA), PCI now includes other new techniques capable of relieving coronary narrowing. Accordingly, in this document, rotational atherectomy, directional atherectomy, extraction atherectomy, laser angioplasty, implantation of intracoronary stents and other catheter devices for treating coronary atherosclerosis are considered components of PCI. In this context PTCA will be used to refer to those studies using primarily PTCA while PCI will refer to the broader group of percutaneous techniques. These new technologies have impacted the effectiveness and safety profile initially established for PTCA. Moreover, important advances have occurred in the use of adjunctive medical therapies such as glycoprotein (GP) IIb/IIIa receptor blockers. In addition, since publication of the previous Guidelines in 1993, greater experience in the performance of PCI in patients with acute coronary syndromes and in community hospital settings has been gained. In view of these developments, further review and revision of the guidelines is warranted. This document reflects the opinion of the third ACC/AHA committee charged with revising the guidelines for PTCA to include the broader group of technologies now termed PCI.
What are the advantages of PCI?
The major advantage of PCI is its relative ease of use, avoiding general anesthesia, thoracotomy, extracorporeal circulation, CNS complications, and prolonged convalescence. Repeat PCI can be performed more easily than repeat bypass surgery, and revascularization can be achieved more quickly in emergency situations.
What is the American Heart Association Task Force on Practice Guidelines?
A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1993 Guidelines for Percutaneous Transluminal Coronary Angioplasty) Endorsed by the Society for Cardiac Angiography and Interventions
How many PCI procedures are performed annually?
More than 500,000 PCI procedures are performed yearly in the U.S., and it has been estimated that more than 1,000,000 procedures are performed annually worldwide. New coronary devices have expanded the clinical and anatomical indications for revascularization initially limited by balloon catheter angioplasty. For example, stents reduce both the acute risk of major complications and late-term restenosis. The success of new coronary devices in meeting these goals is in part represented by the less frequent use of PTCA alone (<30%) and the high (>70%) penetration of coronary stenting in the current practice of interventional cardiology. Atherectomy devices and stenting, associated with improved acute angiographic and clinical outcomes compared to PTCA, in specific subsets, continue to be applied to a wider patient domain that includes multivessel disease and complex coronary anatomy. However, strong evidence (level A data from multiple randomized clinical trials) is only available for stenting in selected patients undergoing single-vessel PCI. These Guidelines will focus on the Food and Drug Administration (FDA) approved balloon-related and nonballoon coronary revascularization devices.
What are the components of PCI?
Accordingly, in this document, rotational atherectomy, directional atherectomy, extraction atherectomy, laser angioplasty, implantation of intracoronary stents and other catheter devices for treating coronary atherosclerosis are considered components of PCI.
What are procedural complications?
As outlined in the 1998 coronary interventional document, procedural complications are divided into six basic categories: death, MI, emergency CABG, stroke, vascular access site complications, and contrast agent nephropathy. Key data elements and definitions to measure the clinical management and outcomes of patients undergoing diagnostic catheterization and/or PCI have been defined in the Clinical Data Standards document and the ACC-National Cardiovascular Data Registry™ Catheterization Laboratory Module version 2.0. These rigorous definitions for key adverse events are endorsed by this Writing Committee for inclusion in the present PCI Guidelines (Table 1 ).
Is PCI good for MI?
Observational studies support the value of PCI for patients who develop cardiogenic shock in the early hours of MI. For patients who do not have mechanical causes of shock, such as acute mitral regurgitation or septal or free wall rupture, mortality among those having PCI is lower than those treated by medical means.
Advanced PCI techniques used during CHIP
Advanced PCI techniques used during CHIP include rotational, orbital and laser atherectomy (shaves away plaque from the vessel wall, especially calcified plaque), specialized antegrade and retrograde coronary artery chronic total occlusion (CTO) approaches and complex bifurcation stenting.
High-risk factors
A number of factors may lead to a patient being considered high-risk and a candidate for CHIP including:
Protected percutaneous coronary intervention
High-risk CAD patients that have also been diagnosed with advanced heart failure and/or severe heart valve disease are particularly vulnerable during the CHIP procedure due to a weakened heart muscle that compromises blood pressure and cannot pump blood efficiently to the body.
Meet the CHIP Team
Northwestern Medicine Bluhm Cardiovascular Institute is a nationally recognized destination for those who require highly specialized cardiovascular care.
/iStock_000015879631_Large-56a5c5863df78cf77289d937.jpg)