Outpatient parenteral antimicrobial therapy (OPAT) allows patients requiring intravenous antibiotics to be treated outside hospital OPAT is suitable for many infections, especially cellulitis, bone and joint infections, and infective endocarditis
Full Answer
What are parenteral antibiotics?
what are parenteral antibiotics? Parenteral antibioti: It just means injectable antibiotics. Ask U.S. doctors your own question and get educational, text answers — it's anonymous and free! Doctors typically provide answers within 24 hours. Educational text answers on HealthTap are not intended for individual diagnosis, treatment or prescription.
What is Outpatient parenteral antimicrobial therapy?
Outpatient parenteral antimicrobial therapy (OPAT) is defined as the administration of parenteral antimicrobial therapy in at least 2 doses on different days without intervening hospitalization. Recommendations made in the updated guideline for the prescription and management of OPAT are summarized below.
Are Chinese parents more likely to self-medicate their children with antibiotics?
It’s worth noting that nationality was associated with the practices of PSMA in this study, showing that Chinese parents were more likely to self-medicate with antibiotics for children than Occidental parents, the same as the above findings conducted in separate countries [18, 20, 23, 48, 52, 53].
How long does it take to administer antibiotics to a patient?
The usual practice is 30 minutes [73]. Given the rarity of severe immediate type 1 allergic reactions, it is reasonable to administer the first dose of an antimicrobial in a patient’s home under the supervision of a competent healthcare worker in patients with no prior history of allergy to antimicrobials in the same class.
What is parental antibiotic?
The preferred parenteral regimens for community and first-level facility use are a combination of procaine penicillin G and gentamicin, or ceftriaxone given alone, which are safe and retain efficacy when dosed at extended intervals (≥24 hours) by intramuscular administration.
What is a first line treatment antibiotic?
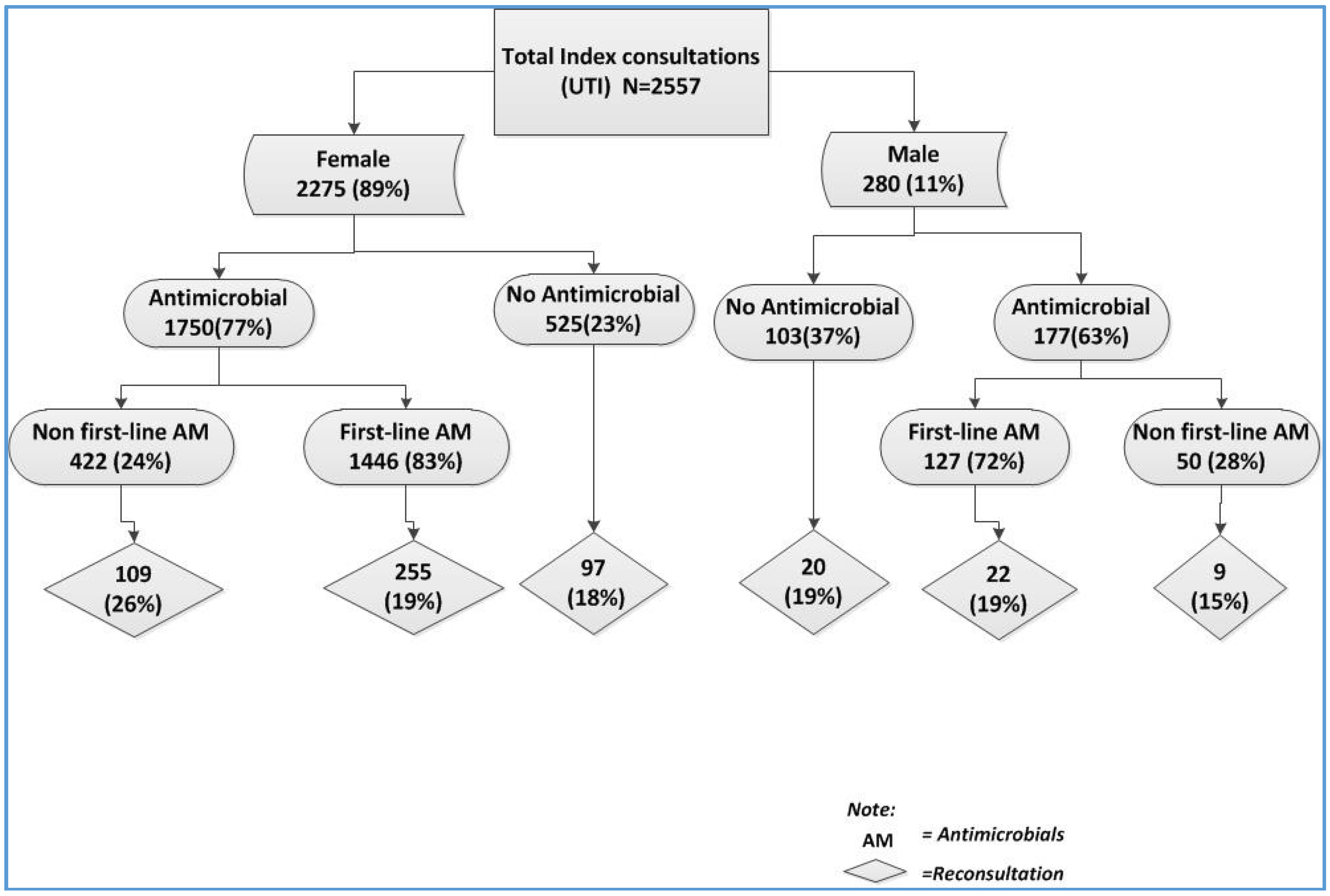
Antibiotics were classified as “first-line” (amoxicillin, TMP-SMX, or erythromycin) or “second-line” (clarithromycin, azithromycin, amoxicillin-clavulanate, cephalosporin, or fluoroquinolone).
What are the different types of antibiotic therapy?
The main types of antibiotics include:Penicillins - for example, phenoxymethylpenicillin, flucloxacillin and amoxicillin.Cephalosporins - for example, cefaclor, cefadroxil and cefalexin.Tetracyclines - for example, tetracycline, doxycycline and lymecycline.Aminoglycosides - for example, gentamicin and tobramycin.More items...•
What is antibiotic treatment used for?
Antibiotics are used to treat or prevent some types of bacterial infections. They are not effective against viral infections, such as the common cold or flu. Antibiotics should only be prescribed to treat health problems: that are not serious but are unlikely to clear up without antibiotics – such as acne.
What are third line antibiotics?
In the event that antibiotic susceptibility testing is unavailable, third line treatment options include rifabutin, rifaximin and sitafloxacin based therapies.
What are second line antibiotics?
The most commonly used second-line therapies include amoxicillin-clavulanate, second- or third-generation cephalosporins (eg, cefuroxime, cefpodoxime, cefdinir), macrolides (ie, clarithromycin), fluoroquinolones (eg, ciprofloxacin, levofloxacin, moxifloxacin), and clindamycin.
What are the 4 classes of antibiotics?
Antibiotic class defines a set of related antibiotics. State-level rates of penicillins, macrolides, cephalosporins, and fluoroquinolones are displayed. Also displayed are all antibiotic classes, which include these four classes plus additional classes not available for release at the state level.
What are the 7 types of antibiotics?
Top 10 List of Antibiotic Classes (Types of Antibiotics)Penicillins.Tetracyclines.Cephalosporins.Quinolones.Lincomycins.Macrolides.Sulfonamides.Glycopeptides.More items...•
What are the 8 classes of antibiotics?
A Guide to the 8 Most Common Classes of AntibioticsPenicillins. Alexander Fleming discovered in 1928 that mold derived from penicillin stopped the growth of bacteria. ... Cephalosporins. ... Sulfonamides. ... Fluoroquinolones. ... Macrolides. ... Tetracyclines. ... Aminoglycosides. ... Carbapenems.
What are the 4 types of infections?
The four different categories of infectious agents are bacteria, viruses, fungi, and parasites. When studying these agents, researchers isolate them using certain characteristics: Size of the infectious agent.
What are side effects of antibiotics?
The most common side effects of antibiotics affect the digestive system. These happen in around 1 in 10 people.vomiting.nausea (feeling like you may vomit)diarrhoea.bloating and indigestion.abdominal pain.loss of appetite.
What are antibiotics give two examples?
Antibiotics are chemical substances produced by a living organism that kill or stop the growth of disease-causing micro-organisms such as fungi and bacteria. Examples of antibiotics: Penicillin. Streptomycin.
What is OPAT?
OPAT is the administration of intravenous (IV) antibiotics outside of an acute care hospital, such as in a skilled nursing facility, outpatient infusion center, or in the home.
Johns Hopkins Bayview Medical Center OPAT Clinic
The Infectious Disease Division has an integrated OPAT management program for patients discharged from Johns Hopkins Bayview Medical Center. This means patients will be managed by a team of specialists from both Johns Hopkins Bayiew Medical Center and Johns Hopkins Hospital depending on which antibiotics patients need.
Johns Hopkins Bayview Medical Center
William F Wright, DO, MPH leads the Johns Hopkins Bayview OPAT clinic. Other physicians with a special clinical interest in OPAT include Mamuka Machaidze, MD; and Sara Karaba, MD, PhD. The Johns Hopkins Bayview Medical Center OPAT clinic is located at:
Rockland Physician Practice at Greenspring Station
Sara Keller, MD, MPH, MSPH leads the Greenspring OPAT clinic. Other physicians with a special clinical interest in OPAT include Christopher Lippincott, MD, MPH ; Maryana Shenderov, MD; and Mamuka Machaidze, MD and William Wright, DO, MPH . The Johns Hopkins Rockland Physician Practice at Greenspring is located at:
John G. Bartlett Specialty Practice
Sara Keller, MD, MPH, MSPH leads the Bartlett OPAT clinic. Other physicians with a special clinical interest in OPAT include Christopher Lippincott, MD, MPH; Maryana Shenderov, MD; Karen Coffey, MD, MPH; Juhi Moon, MD; Mamuka Machaidze, MD; and William Wright, DO, MPH. The John G. Bartlett Specialty Practice is located at:
Clinical Excellence Award
In response to post-discharge safety issues, Johns Hopkins Bayview formed a multidisciplinary team to improve tracking and care coordination for patients on IV antibiotics.
Methods
This study was nested within a multicenter retrospective cohort study 12, 13 of young infants evaluated for invasive bacterial infections in the emergency departments (EDs) of 11 geographically diverse children’s hospitals ( Supplemental Table 3 ).
Results
Of the 497 infants ≤60 days old in the parent study cohort who had a pathogen isolated in blood or CSF culture, we identified 140 infants with bacteremia and UTI caused by the same pathogen. Applying exclusion criteria, we assembled a cohort of 115 infants ≤60 days of age with bacteremic UTI ( Fig 1 ).
Discussion
In this multicenter study of young infants with bacteremic UTI, shorter courses of parenteral antibiotic therapy (ie, ≤7 days) were not associated with significantly more frequent UTI recurrence or all-cause reutilization when compared with longer courses of parenteral antibiotic therapy.
Conclusions
Young infants with bacteremic UTI who received ≤7 days of parenteral antibiotic therapy did not have significantly more 30-day recurrent UTIs or hospital reutilization than infants who received longer courses of parenteral therapy. Our data indicates that ≤7 days of parenteral antibiotic therapy may be safe in this population.
Febrile Young Infant Research Collaborative
We would like to acknowledge the following group participants in the Febrile Young Infant Research Collaborative for their contributions to this study: Elizabeth R. Alpern, MD, MSCE (Northwestern University Feinberg School of Medicine, Chicago, IL), Whitney L. Browning, MD (Vanderbilt University School of Medicine, Nashville, TN), Elana A.
Competing Interests
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
