Medication
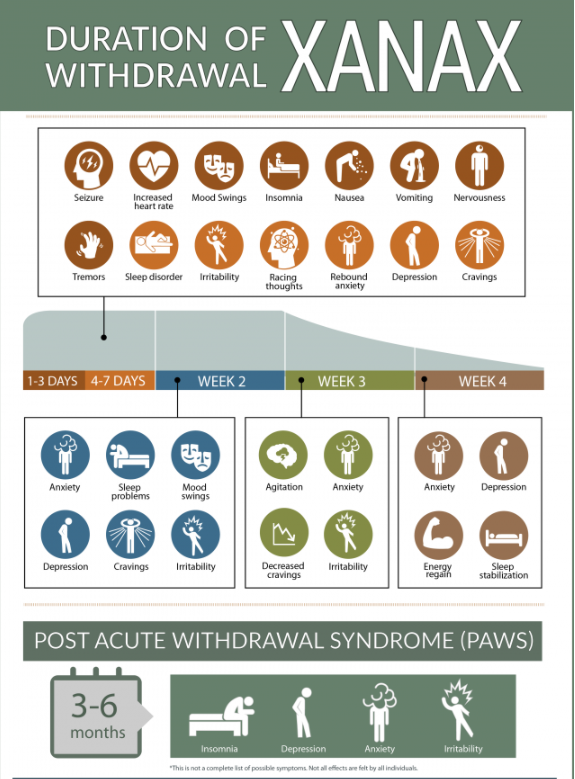
- Use medication only as a backup to behavioral changes.
- Use the lowest dose that is effective.
- Don't take a pill every night. Instead, use medication only when an uninterrupted night's sleep is really important. ...
- Try to stop using medication after three to four weeks.
- Discontinue medication gradually to avoid rebound insomnia.
Therapy
- Here are the steps to fall asleep fast the military way:
- Relax the muscles in your face, including the tongue, jaw, and the muscles around the eyes.
- Relax your shoulders by dropping them as far down as they will go.
- Relax your upper and lower arm, one side at a time.
- Breathe out, relaxing your chest.
Self-care
These 6 best natural home remedies for deep sleep will help you fall asleep fast and stay asleep:
- Orange blossom tea or orange blossom water
- Oatmeal
- Magnesium
- Zinc
- Ashwagandha
- Homeopathic remedies for insomnia
Nutrition
What Are The Effective Ways On How To Stop Insomnia Naturally Without Using Pills?
- Keep Your Slumber Surroundings Tranquil: Your slumber surroundings are very important to your good sleep. ...
- Go To Bed And Wake Up On Time: One of the ways on how to stop insomnia naturally is that you need to go to bed at the same ...
- Avoid Caffein After 2 P.M: If you have some caffein, it takes about 12 hours to make caffein disappear completely. ...
See more
How long does it take to get over insomnia?
How to cure insomnia in twelve minutes?
What is the best natural treatment for insomnia?
How to stop insomnia naturally and effectively without pills?
What is the best long term solution for insomnia?
Basic tips:Stick to a sleep schedule. Keep your bedtime and wake time consistent from day to day, including on weekends.Stay active. ... Check your medications. ... Avoid or limit naps. ... Avoid or limit caffeine and alcohol and don't use nicotine. ... Don't put up with pain. ... Avoid large meals and beverages before bed.
Is there a permanent cure for insomnia?
Can My Insomnia Be Cured? Absolutely. It may not be easy though, as curing insomnia often means improving your sleep hygiene and establishing habits that are more conducive to good sleep. And habits, especially routines you follow every day, can be tough to break.
What causes chronic insomnia?
Common causes of insomnia include stress, an irregular sleep schedule, poor sleeping habits, mental health disorders like anxiety and depression, physical illnesses and pain, medications, neurological problems, and specific sleep disorders.
Is insomnia a mental illness?
Insomnia is rarely an isolated medical or mental illness but rather a symptom of another illness to be investigated by a person and their medical doctors. In other people, insomnia can be a result of a person's lifestyle or work schedule.
What is the best medication for insomnia?
It is important to keep in mind that standard medical practice advises against using prescription medication for insomnia for longer than a few wee...
How can I get rid of insomnia?
There are a few ways to alleviate insomnia without the use of pharmaceuticals. Making sure you only get into bed when you are going to sleep, and g...
What is sleep hygiene?
Sleep hygiene encompasses practices meant to establish good sleeping habits. For example, if you watch television, read, or use a smartphone or tab...
Does drinking alcohol help you get a deep sleep?
There are many home remedies to help you sleep that include some type of alcohol. Unfortunately, the idea that drinking alcohol is good for sleep i...
What is the best treatment for insomnia?
Cognitive behavioral therapy for insomnia (CBT-I) can help you control or eliminate negative thoughts and actions that keep you awake and is generally recommended as the first line of treatment for people with insomnia. Typically, CBT-I is equally or more effective than sleep medications.
What is the therapy for learning insomnia called?
Remaining passively awake. Also called paradoxical intention , this therapy for learned insomnia is aimed at reducing the worry and anxiety about being able to get to sleep by getting in bed and trying to stay awake rather than expecting to fall asleep.
What is the purpose of sleep study?
Tests are done to monitor and record a variety of body activities while you sleep, including brain waves, breathing, heartbeat, eye movements and body movements.
How does sleep restriction work?
Sleep restriction. This therapy decreases the time you spend in bed and avoids daytime naps, causing partial sleep deprivation, which makes you more tired the next night. Once your sleep has improved, your time in bed is gradually increased. Remaining passively awake.
How to get rid of insomnia?
If these measures don't work, your doctor may recommend cognitive behavioral therapy, medications or both , to help improve relaxation and sleep.
What is the diagnosis of insomnia?
Diagnosis. Depending on your situation, the diagnosis of insomnia and the search for its cause may include: Physical exam. If the cause of insomnia is unknown, your doctor may do a physical exam to look for signs of medical problems that may be related to insomnia. Occasionally, a blood test may be done to check for thyroid problems ...
How to reduce anxiety at bedtime?
Relaxation techniques. Progressive muscle relaxation, biofeedback and breathing exercises are ways to reduce anxiety at bedtime. Practicing these techniques can help you control your breathing, heart rate, muscle tension and mood so that you can relax. Sleep restriction.
How long does insomnia last?
These symptoms must occur for at least 3 months despite adequate opportunities for sleep on a nightly basis.
How to treat insomnia 4?
Treating chronic insomnia 4 includes two main objectives: improving sleep quality and duration, and reducing associated daytime impairments. A chronic insomnia treatment regimen typically includes at least one behavioral intervention, which often takes the form of cognitive behavioral therapy for insomnia (CBT-i); if therapy and other behavioral interventions are not effective, your doctor may recommend some form of sleep medication.
How does biofeedback 7 help with insomnia?
Biofeedback 7 – which helps you control different bodily functions based on your blood pressure, breathing and heart rates, and other metrics – can also be effective for reducing insomnia symptoms and improving sleep . The number of qualified behavioral sleep medicine therapists in the U.S. is fairly limited.
What is sleep hygiene?
Specifically, sleep hygiene focuses on increasing behaviors that improve sleep quality and quantity while eliminating behaviors that cause sleep problems.
What is chronic insomnia?
Chronic Insomnia Treatment. Insomnia is a disorder characterized by persistent difficulty 1 with sleep onset, maintenance, consolidation, or quality. People who have insomnia struggle with sleep despite adequate opportunities for sleep, and also experience excessive daytime sleepiness and other dysfunctions when they are awake.
What is CBT I?
In most cases, CBT-i is provided by a licensed psychologist who has received training for this type of treatment. CBT-i focuses on pinpointing the anxieties people with insomnia often have about sleep, and then replacing these anxieties with healthier beliefs and attitudes.
What is insomnia diagnosis?
Lack of motivation or energy. An insomnia diagnosis will include a standard medical exam and questionnaire. These procedures allow your doctor to determine whether the insomnia is an isolated condition, or if you’re experiencing insomnia symptoms due to an underlying disease or medical disorder.
How long does it take for CBT to be drug free?
85% of the patients who received the medication withdrawal alongside CBT were drug free after 10 weeks. [2]
What are the components of cognitive behavioral therapy?
The core components of cognitive behavioral therapy include stimulus control, sleep restriction and sleep hygiene - all of which are covered in my free sleep training course.
Can sleeping pills help with insomnia?
Sleeping pills are not a long term solution for insomnia. Behavioral changes are often far more effective (and non-addictive).
Does CBT improve sleep quality?
Most of those who underwent CBT reported that they were still enjoying an improved quality of sleep, two years later. [1]
Is CBT better than sleeping pills?
Behavioral techniques such as CBT have been proven to be more effective than sleeping pills when it comes to improving sleep and curing insomnia.
What is insomnia treatment?
Insomnia Treatment. Insomnia is when someone is unable to sleep as much as they would like to, and there is no discernible cause. This can be a very frustrating situation, as the lack of sleep’s effects can worsen as sleep debt increases over time. 1 There are a number different insomnia treatments, some of which are behavioral ...
How Do You Treat Insomnia?
It is important to know what is and what is not insomnia. Insomnia doesn’t include situations where someone is being kept awake or prevented from sleeping by an external stimulus. It is also not considered insomnia if a stimulant like caffeine or the effect of other drugs are the reason someone is unable to sleep. If the difficulty sleeping occurs for at least three nights a week and continues for at least three months, and is not the result of another mental illness, then it is likely to be classified as insomnia. 2
How to get rid of insomnia without drugs?
There are a few ways to alleviate insomnia without the use of pharmaceuticals. Making sure you only get into bed when you are going to sleep, and getting out of bed if you are unable to fall asleep within twenty minutes, can help establish good sleeping habits. 4 There are also two methods which are somewhat paradoxical in how they work. Sleep restriction, whereby you actively avoid sleeping as much as you would like, can make you tired enough to quickly fall asleep and stay asleep. You can also try to stay awake in bed, and the focus on staying awake can relieve you of the anxiety of being unable to sleep.
What is sleep hygiene?
Sleep hygiene encompasses practices meant to establish good sleeping habits. For example, if you watch television, read, or use a smartphone or tablet in bed, your body may learn to associate the bed with activities other than sleeping. A good sleep hygiene practice would be to only use the bed when sleeping.
How to fall asleep fast?
If you want to learn how to fall asleep fast, you should establish sleep hygiene, or good sleep habits. If you often do things other than sleep when in bed, your body and brain may have learned that going to bed doesn’t always mean going to sleep. By limiting your activities in bed to simply sleeping, you can break this association. If you find yourself lying in bed unable to sleep for at least twenty minutes, you should rise and do something else before returning to bed.
What medications are approved for long term use?
There are prescription drugs which are approved for long-term use by the United States Food and Drug Administration, such as zolpidem, zaleplon, ramelteon, and eszopiclone. Any use of a prescription sleeping pill should be under the care of a practicing medical doctor. 3.
What is the best medication for insomnia?
Drugs that are used as insomnia treatments include zolpidem, ramelteon, zaleplon, and eszopiclone. These substances are available by prescription, and should only be taken if recommended by a doctor.
Is insomnia a disorder?
Insomnia is a very common disorder with a preva-lence of approximately 25% for acute insomniaand 10% for chronic insomnia. Chronic insomniais associated with increased fatigue, cognitiveimpairment, mood disturbance, physical com-plaints and reduced quality of life.1–4Beyond thesesequelae, there is now considerable evidence thatchronic insomnia increases the risk of substanceabuse,5psychiatric illness (especially major depres-sive disorder),5–11hypertension and/or cardiovasculardisease,12dysregulation of glucose homeostasis,13immunosuppression14and increased mortality.15Despite the prevalence and consequences of allow-ing insomnia to go untreated, there are no bestpractice guidelines for its long-term management.In this review, we will provide:
Is insomnia a chronic disease?
At present, insomnia is considered a chronic dis-order and there is no rational approach to itspharmacological management over the long term.There is no evidence that the medical treatment ofinsomnia results in clinical improvements that per-sist beyond the period in which active treatment isprovided. In fact, it is generally accepted that whentreatment is discontinued, insomnia recurs withequal or worse severity (depending on the medica-tion). Given that primary insomnia is a chronicdisorder and ‘insomnialytics’ have no effectsbeyond active treatment, the only remainingoption for the pharmacological management ofinsomnia is long-term treatment or maintenancetherapy. While such an approach is now the stan-dard of practice for disorders such as hypertensionand major depression, there has been a reluctanceto engage a similar strategy for chronic insomnia.The major concerns are two-fold: is primaryinsomnia sufficiently serious to warrant long-termtreatment; and are the BZRA sedatives effective in thelong term without habituation and dose escalation?
What is insomnia?
For others, insomnia is a chronic problem that affects mood, daytime alertness and performance, and emotional and physical health. Chronic insomnia often starts out innocently enough. Stress or trouble at home or work interferes with sleep for a few nights. But then the habits that come along with not sleeping—looking at the clock, ...
How to break the cycle of insomnia?
One widely used behavioral approach, called stimulus control therapy, aims to break harmful sleep habits and thoughts over the course of several weeks. A new approach that uses a 25-hour program called intensive sleep retraining may be enough to break the cycle in a day.
How long does intensive sleep retraining last?
Intensive sleep retraining works like this: The night before undergoing the program, a person with chronic insomnia sleeps (or stays in bed) no more than five hours. The next day, he or she reports to a sleep lab around bed time. The next 25 hours are divided into 50 thirty-minute sessions.
How long is a 25 hour sleep session?
The next 25 hours are divided into 50 thirty-minute sessions. During each one, the person tries to fall asleep. If successful, the participant is woken up after just three minutes of sleep, asked if he or she had been asleep, and told that he or she had indeed fallen asleep.
Is Montmorency Cherry good for insomnia?
If you are looking into some thing more economical, there are natural supplements available to treat chronic insomnia. The Montmorency cherry is an effective aid for sleep loss because it has natural melatonin built in. My next door neighbor struggled with insomnia for years.
Does stress cause insomnia?
I like your article here about chronic insomnia. One thing you do mention is how chronic stress can precipitate and continue the ongoing problems with insomnia.many people don’t realize until it’s too late the chronic effects of stress.
Is sleep retraining expensive?
As the researchers themselves point out, though, intensive sleep retraining is expensive. Many people who need it can’t afford it.
How long does insomnia last?
1, 2 Insomnia is classified as short-term if it persists less than 3 months and chronic if it persists at least 3 months and occurs at least three times per week. 1, 2 Similar essential features of insomnia are described in the American Psychiatric Association (APA) Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition and include dissatisfaction with sleep quantity or quality with complaints of difficulty initiating or maintaining sleep. 3 The sleep disturbance must also cause clinically significant distress or impairments in social, occupational, or other important areas of functioning and may occur independently or during the course of another mental disorder or medical condition. 3 For many, insomnia becomes a long-term and persistent condition. A recent longitudinal study based on annual survey data demonstrated that 37.5% of participants with insomnia disorder at baseline continued to report insomnia symptoms through 5 years of follow-up. 4
How often do you get insomnia?
Chronic insomnia disorder, which affects 6–10% of the population, is diagnostically characterized by ongoing difficulties with initiating or maintaining sleep occurring at least three times per week, persisting for at least 3 months, and associated with daytime impairment. While chronic insomnia is often considered a condition primarily related to impaired sleep, the disorder can also adversely affect domains of physical and mental health, quality of life, and daytime function, which highlights the importance of treating the multidimensional sleep disorder. Owing to misperceptions about the safety and effectiveness of treatment options, many individuals with insomnia may not seek professional treatment, and alternatively use ineffective home remedies or over-the-counter medications to improve sleep. Some physicians may even believe that insomnia is remediated by simply having the patient “get more sleep”. Unfortunately, treatment of insomnia is not always that simple. The disorder’s complex underlying pathophysiology warrants consideration of different nonpharmacologic and pharmacologic treatment options. Indeed, recent insights gained from research into the pathophysiology of insomnia have facilitated development of newer treatment approaches with more efficacious outcomes. This narrative review provides a summary of the diagnostic criteria and pathophysiology of insomnia and its subtypes. Further, this review emphasizes new and emerging nonpharmacologic and pharmacologic treatments for chronic insomnia, including recent enhancements in approaches to cognitive behavioral therapy for insomnia (CBT-I) and the new dual orexin receptor antagonist (DORA) pharmacologics. These advances in treatment have expanded the treatment options and are likely to result in improved outcomes in patients with chronic insomnia.
How does sleep signaling work?
Wake/sleep signaling in the brain is driven by two competing sets of brain circuitry: one set of neurotransmitter pathways that promotes sleep and another set that promotes wakefulness. 60 Transitions between sleep and wake states are dependent on the relative strengths of the two opposing sets of circuits and the end result has been described as akin to a flip-flop switch. 60 Historically, the most common approach in the pharmacologic treatment of insomnia has been to increase the sleep signal, such as with medications that target the γ-aminobutyric acid (GABA)-A receptor. However, this may not be the best approach physiologically if the insomnia disorder is due to excessive wake signaling occurring at the time when the individual is expected to fall asleep and remain asleep. Decreasing the excessive wake signal has recently become a viable option for medication treatment now that orexin has been identified as a key central promotor of wakefulness.
What is secondary insomnia?
The International Classification of Sleep Disorders, Third Edition and Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition also describe several secondary insomnias, which arise from co-occurring primary or causative conditions including mental disorders (eg, major depressive disorder), medical conditions (eg, pain), substance use, or another sleep disorder (eg, breathing-related sleep disorder). 1, 3 Despite these insomnia subtypes, it is often difficult to differentiate between them clinically due to substantial symptom overlap between primary and secondary insomnia. Additionally, it is often difficult to assign causation to any single factor or establish the precise nature of the relationship between insomnia and a co-occurring condition. 3 Indeed, insomnia frequently persists despite resolution of other conditions and often requires independent treatment. 5, 6 Some studies have shown that cotreatment of insomnia and co-occurring conditions yield more rapid improvement of both conditions compared with independent treatment of only the co-occurring condition, supporting the treatment of insomnia as an independent condition in patients considered to have the “secondary” condition due to a primary medical or mental cause. 7, 8 Other than the different treatments required for distinctive comorbidities, effective treatments for insomnia generally are the same across “primary” or “secondary” insomnia. 1, 2, 9, 10 It is important to note, however, that for some of the more recent insomnia treatments (eg, dual orexin receptor antagonists [DORAs]), less is known about their effectiveness in patients with insomnia and comorbidities as these newer agents are relatively new and studies of those that have become commercially available have not yet been conducted to evaluate their efficacy specifically in insomnia patients with co-occurring disorders.
How does insomnia affect quality of life?
The consequences of insomnia extend even further in that it can also reduce quality of life (QOL), impair neurocognitive functioning, 31 and pose economic and public health burdens through increased health care utilization, sick leave, and decreased work productivity. 32, 33 An international cross-sectional survey comparing health-related QOL among sufferers of chronic insomnia with good sleepers found that people with insomnia reported significantly reduced health-related QoL as assessed using the 36-Item Short-Form Health Survey. 34, 35 Likewise, the National Epidemiologic Survey on Alcohol and Related Conditions-III (2012–2013) found that the annual loss of quality-adjusted life-years associated with insomnia was significantly greater than other medical conditions assessed, including arthritis, depression, and hypertension. 36
What are the different types of insomnia?
11–13 The main categories are difficulty falling asleep (sleep-onset insomnia), difficulty staying asleep (sleep-maintenance insomnia), early-morning awakenings coupled with an inability to return to sleep (terminal insomnia), and combined insomnia (more than one of these categories). 13, 14 Additionally, insomnia with objective short sleep duration (<6 hours by polysomnography) has also been identified as an important phenotype. 15 Identification of a patient’s specific insomnia phenotype (eg, sleep-onset versus sleep-maintenance insomnia) may help guide treatment. 14 It is critically important to recognize the dynamic nature of insomnia, and that the stability of a patient’s insomnia symptoms may vary over time. 13 A 4-month longitudinal study of general practice attenders found that only 17–51% of the patients reported the same sleep complaint (s) at follow-up. 12 Similarly, in a large, longitudinal community-based study of individuals with current or lifetime insomnia, approximately 60% retained the same insomnia symptom phenotype after 1 year; 40% had a different phenotype. 14 The demonstration in these studies that many patients have conversion of their insomnia symptoms 12, 14 highlights that ongoing assessment is needed to monitor for potential changes in the presenting insomnia symptoms.
How many people have insomnia?
In industrialized nations, chronic insomnia disorder is estimated to occur in 5–10% of the general population, although some studies suggest that the rate is as high as 33% of the adults. 2, 37 Despite the large percentage, a relatively low proportion consult a health care provider about their sleep. 38–40 The low consultation rate may be due to limited knowledge among the general population about the safety and availability of insomnia treatments that can be offered by clinicians. Self-treatment with over-the-counter sleep aids, as well as alcohol, is not unusual. 41 Owing to this low rate of consultation about insomnia, health care providers may not consistently recognize and diagnose the condition, 39 which likely contributes to undertreatment of insomnia. 13, 39, 42
How to treat insomnia?
Regardless of the type of therapy used, the treatment of chronic insomnia has two primary objectives: improving sleep quality and quantity , and improving daytime impairments . Initial approaches to treatment usually include at least one behavioral intervention, such as stimulus control therapy or relaxation therapy. Biofeedback therapy is also used. When pharmacotherapy is required, the choice of a specific drug within a class should be directed by: 1) symptom pattern; 2) treatment goals; 3) past treatment responses; 4) patient preference; 5) cost; 6) the availability of other treatments; 7) comorbid conditions; 8) contraindications; 9) concurrent medication interactions; and 10) potential adverse effects. 25
How long does insomnia last?
The Centers for Disease Control and Prevention further classifies insomnia as episodic (lasting at least one month but less than three months); persistent (lasting three months or longer); or recurrent (two or more episodes within one year).24
What is insomnia related to?
Associated insomnia is primarily related to an underlying mental or mood disorder, such as depression, dysthymia, cyclothymia, bipolar disorder, anxiety, or schizophrenia.17,20–23This form of insomnia may also be caused by inadequate sleep hygiene (i.e., habits that are inappropriate for good quality of sleep), such as psychologically stressful activities; the consumption of caffeine, nicotine, alcohol, or heavy meals; or vigorous physical activity near bedtime.17Other potential causes of associated insomnia include concomitant medical conditions (e.g., infections and metabolic diseases) and the use of substances or medications (e.g., alcohol, stimulants, and antidepressants).17
What is insomnia in the DSM-5?
According to the Diagnostic and Statistical Manual of Mental Disorders,fifth edition (DSM-5), insomnia is defined as dissatisfaction with sleep quantity or quality that results in clinically significant distress or impairment in social, occupational, or other important areas of functioning. Insomnia is associated with one or more of the following symptoms: difficulty initiating sleep (sleep-onset insomnia or initial insomnia); difficulty maintaining sleep (sleep-maintenance insomnia or middle insomnia); and early-morning awakening with the inability to return to sleep (late insomnia).4
What are the causes of insomnia?
Primary chronic insomnia may be caused by several predisposing (genetic and constitutional) factors, including hyperactivity of stress response mechanisms or of the HPA axis; anxiety and depression; and abnormalities in the circadian rhythm (circadian sleep-wakefulness control).12,14,17–19Precipitating and perpetuating factors, such as psychosocial features (e.g., fatigue and irritability), behavioral changes, and cognitive characteristics, also contribute to insomnia.13
How many people have sleep disorders?
An estimated 50 million to 70 million adults in the U.S. have chronic sleep and wakefulness disorders.5Insomnia is more common in women (25%) than in men (18%), and its prevalence increases with age, affecting approximately 50% of the elderly population.6Data from the years 2008 through 2010 from the National Health Interview Survey indicated that 62% of adults in the U.S. slept seven to eight hours and that 28% slept six or fewer hours in a 24-hour period.7In the National Health and Nutrition Examination Survey (2005–2010), approximately 4% of U.S. adults 20 years of age and older reported that they had taken prescription sleep aids during the previous 30 days.8
What are the two forms of sleep?
People experience two forms of sleep: rapid eye movement (REM) and nonrapid eye movement (NREM). Sleep typically begins with the NREM phase, which is followed by the REM phase. NREM sleep is subdivided into three stages in which brain activity, eye movement, and skeletal muscle tone progressively decrease, placing the individual in a deeper state of sleep. Later in the cycle, when the individual enters REM sleep, electrical activity in the brain increases, contributing to increased blood flow to the brain, changes in respiratory and cardiac rates, and dreaming.1REM sleep correlates with activities of the hypothalamic-pituitary-adrenal (HPA) axis and the sympathetic nervous system in healthy humans.2
Diagnosis
Treatment
Clinical Trials
Lifestyle and Home Remedies
Alternative Medicine
Preparing For Your Appointment