Medication
What tests do doctors use to diagnose primary biliary cholangitis?
- Blood tests. For a blood test, a health care professional will take a blood sample from you and send the sample to a lab.
- Imaging tests
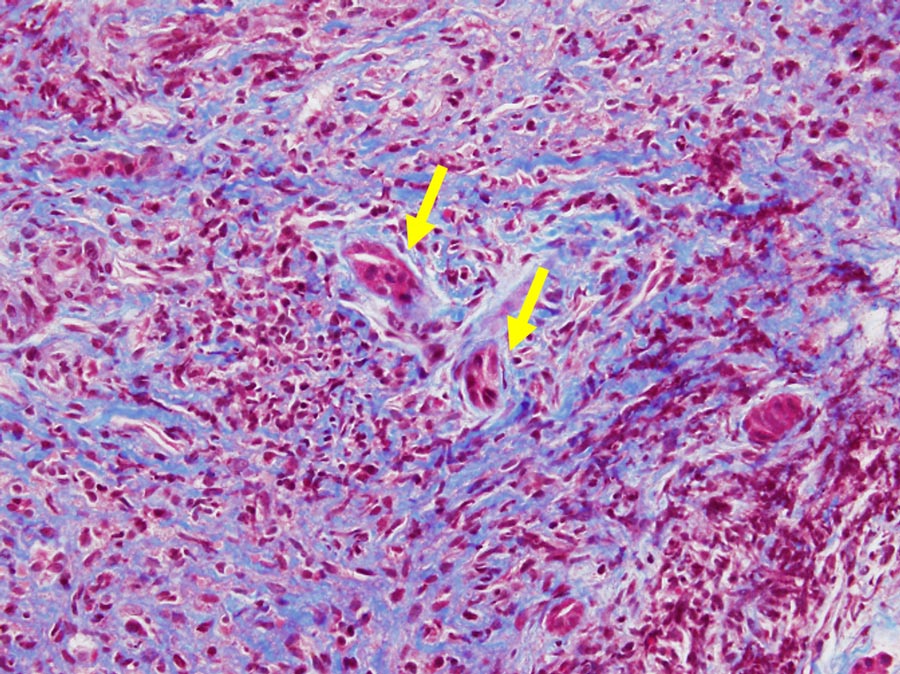
- Liver biopsy. During a liver biopsy, a doctor will take small pieces of tissue from the liver. A pathologist will examine the tissue with a microscope.
Procedures
What can I do to help prevent further liver damage?
- carefully follow your doctor’s instructions and take your medicines and dietary supplements as directed.
- quit smoking External link .
- avoid drinking alcohol. ...
- have regular checkups, as recommended by your doctor.
- talk with your doctor before taking prescription medicines. ...
- try to reach and stay at a healthy body weight.
Self-care
Tests and procedures used to diagnose primary sclerosing cholangitis include:
- Liver function blood test. A blood test to check your liver function, including levels of your liver enzymes, can give your doctor clues about your diagnosis.
- MRI of your bile ducts. ...
- X-rays of your bile ducts. ...
- Liver biopsy. ...
Nutrition
What causes primary biliary cholangitis?
- infections
- cigarette smoking
- exposure to certain chemicals
How will your doctor diagnose primary biliary cholangitis?
How can primary biliary cholangitis be treated?
How to diagnose PSC?
What causes primary biliary cholangitis?
How long can you live with primary sclerosing cholangitis?
CP Studies have suggested that the median transplant-free survival of patients with PSC ranges from 9.3—18 years; however, in a large population-based study on the epidemiology and natural history of PSC that we recently performed in The Netherlands, a median transplant-free survival of 21.3 years was found.
What is the survival rate of PSC?
Patient and Graft Survival Rate and PSC Recurrence. The rate of patient survival, estimated by Kaplan Meier analysis, was 77.8% at 1 year, 73.2% at 3 years, 63.0% at 5 years, 57.5% at 7 years, and 54.6% at 10 years (Figure
What are the final stages of PSC?
Ludwig et al (33) described four stages of PSC: cholangitis or portal hepatitis (stage 1); periportal fibrosis or periportal hepatitis (stage 2); septal fibrosis, bridging necrosis or both (stage 3); and biliary cirrhosis (stage 4).
Does PBC shorten life expectancy?
People with PBC may not develop any symptoms for up to 10 years. And if a person has an earlier stage of PBC (stage 1 or 2), their life expectancy is normal. If a person with PBC has advanced symptoms as seen in an advanced stage, the average life expectancy is about 10-15 years . However, everyone is different.
Can you live a long time with PSC?
However, with limited treatment options, people with PSC can live for many years with a number of debilitating symptoms such as fatigue, itch, and pain, as well as the emotional burden of an uncertain future [6, 10], all of which can impact on quality of life (QoL) [11, 12].
Is PSC always fatal?
As individuals with PSC age, they often eventually develop life-threatening complications such as liver (hepatic) failure. Individuals with PSC are at a greater risk than the general population of developing a form of cancer that affects the bile ducts (cholangiocarcinoma).
Is primary sclerosing cholangitis serious?
In primary sclerosing cholangitis, inflammation causes scars within the bile ducts. These scars make the ducts hard and narrow and gradually cause serious liver damage.
How do you prevent recurrent cholangitis?
Prevention. Consider maintenance therapy/antibiotics (ie, sulfamethoxazole and trimethoprim [SMZ-TMP] or a fluoroquinolone) for patients with recurrent cholangitis.
Can sclerosing cholangitis be cured?
Currently, no cure or effective treatments for primary sclerosing cholangitis (PSC) exist. However, doctors can treat narrowed or blocked bile ducts and symptoms of PSC.
How long can you take ursodiol?
You may need to take ursodiol for up to two years for the treatment of gallstones. Once the gallstones have dissolved, your physician may continue your treatment for three to four months to ensure that they have completely cleared up.
What is the prognosis for primary biliary cholangitis?
Prognosis for PBC Patients who present without symptoms tend to develop symptoms over 2 to 7 years but may not do so for 10 to 15 years. Once symptoms develop, median life expectancy is 10 years.
Is primary biliary cholangitis fatal?
The rate at which PBC progresses varies between individuals. Sometimes, it can take decades. Without treatment, the liver can become so badly damaged that it no longer works properly. This is known as liver failure and can be fatal.
How can i treat primary sclerosing cholangitis?
Difficult problem: Psc: autoimmune swelling/scarring of bile ducts within and outside the liver; often associated with infl. Bowel (usually ulc colitis). Increased risk ... Read More
When does sclerosing cholangitis onset?
Sorry to hear: Primary sclerosing cholangitis tends to occur more frequently in males than women and onset may be between 20-30yrs old. Sometimes it is isolated, ot... Read More
What is the definition or description of: primary sclerosing cholangitis?
PSC: Primary sclerosing cholangitis ( psc) is a chronic liver disease caused by progressive inflammation and scarring of the bile ducts of the liver. The in... Read More
Do people with primary sclerosing cholangitis have a lot of pain?
Depends: Primary sclerosing cholangitis ( ps c) causes destruction of the bile ducts inside and outside of the liver. The first symptoms of the disease include ... Read More
Will primary sclerosing cholangitis kill me?
Yes: It is a disease that slowly progresses and eventually without treatment leads to hepatic failure which has a very high mortality rate.
What is the prognosis and life expectancy for a person with primary sclerosing cholangitis?
Aside from liver transplantation, there are no effective treatments for PSC. In the US, studies suggest that life expectancy ranges from 9 to 18 years if the patient does not undergo liver transplantation. Using different population study models, researchers in the Netherlands concluded that life expectancy may be longer than 21 years from the time when the diagnosis is made.
How do doctors make a diagnosis of primary sclerosing cholangitis?
In patients with inflammatory bowel disease, the health care professional should have a high suspicion of the diagnosis because of the relationship between PSC and ulcerative colitis.
What causes primary sclerosing cholangitis?
The cause of PSC is unknown but it has an association with inflammatory bowel disease , especially ulcerative colitis. It is thought that there may be an autoimmune component to the disease, where the body's immune system attacks the bile ducts in the liver and causes them to become, inflamed and narrowed.
What is PSC in liver?
PSC is a progressive disease, damaging the bile ducts and reducing the bile flow, ultimately leading to portal hypertension, cirrhosis, and liver failure. Some cancers are associated with primary sclerosing cholangitis including gallbladder cancer, hepatocellular cancer ( cancer of the liver cells) and cholangiocarcinoma ( cancer of the bile ducts).
What is the term for a disease in which the bile ducts in the liver become inflame?
Primary sclerosing cholangitis describes a disease process in which the bile ducts in the liver become inflamed, narrow and prevent bile from flowing properly.
What is the term for the liver cells that die when you have liver failure?
As the disease progress, liver cells die and are replace by scar tissue. This is called cirrhosis and is associated with liver failure.
What is the survival rate for liver transplant?
The three-year U.S. survival rate for all transplants is 81%. The five-year survival rate is about 75%, according to the data from the Scientific Registry of Transplant Recipients.
What is the first line of treatment for sclerosing cholangitis?
Bile acid sequestrants. Medications that bind to bile acids — the substances thought to cause itching in liver disease — are the first line treatment for itching in primary sclerosing cholangitis.
What test is used to diagnose sclerosing cholangitis?
Tests and procedures used to diagnose primary sclerosing cholangitis include: Liver function blood test. A blood test to check your liver function, including levels of your liver enzymes, can give your doctor clues about your diagnosis. MRI of your bile ducts.
Why is a bile duct test rarely used?
But this test is rarely used for diagnosis because of the risk of complications. To make your bile ducts visible on an X-ray, your doctor uses a flexible tube passed down your throat to inject dye into the area of your small intestine where your bile ducts empty.
Can sclerosing cholangitis recur after liver transplant?
Though uncommon, it's possible for primary sclerosing cholangitis to recur after a liver transplant.
Can you take antibiotics for sclerosing cholangitis?
To prevent and treat these infections, people with primary sclerosing cholangitis may take repeated courses of antibiotics or continue taking antibiotics for long periods. Before any procedure that could cause an infection, such as an endoscopic procedure or abdominal surgery, you'll also need to take antibiotics.
Does sclerosing cholangitis slow or reverse the liver?
Many medications have been studied in people with primary sclerosing cholangitis, but so far none have been found to slow or reverse the liver damage associated with this disease.
Can alternative medicine help with sclerosing cholangitis?
No alternative medicine treatments have been found to treat primary sclerosing cholangitis. But some complementary and alternative therapies may help you cope with the signs and symptoms of the disease. Talk to your doctor about your options.
How long does a PSC patient live after transplant?
CPStudies have suggested that the median transplant-free survival of patients with PSC ranges from 9.3—18 years; however, in a large population-based study on the epidemiology and natural history of PSC that we recently performed in The Netherlands, a median transplant-free survival of 21.3 years was found. Diagnosis of PSC was commonly preceded by a period of up to 5 years when, in retrospect, symptoms or abnormal laboratory values could be attributed to the disease. The findings from this population-based review were recently published in Hepatology.
What is the survival rate for a liver transplant?
As for the prognosis of patients who undergo liver transplantation for PSC, the 5-year survival rate is approximately 85%.
What are the symptoms of cirrhosis of the liver?
These signs and symptoms typically include splenomegaly, ascites, portal hypertension, and jaundice. Patients also are at increased risk for the development of cholangiocarcinoma (CCA), which can occur at any time. The presenting symptoms of CCA usually are progressive fatigue, weight loss, and jaundice.
Does CPAt help with fatigue?
CPAt present, there is no medical or endoscopic therapy with proven efficacy to halt disease progression. This implies that therapy is directed to alleviate symptoms. Ursodeoxycholic acid (UDCA), a hydrophilic, dihydroxy bile acid, can ameliorate pruritus and fatigue. Pruritus that does not respond to resins such as cholestyramine can be treated with a low to medium dose of rifampicin, which is a pregnane X receptor agonist and enhances the metabolism of pruritogens probably by inducing biotransforming enzymes and transport molecules. As a third-line therapy, the opioid antagonist naltrexone can be used. When patients have increased cholestatic complaints and an increase in alkaline phosphatase and/or bilirubin levels, the a priori chance of existence of a symptomatic-dominant stricture is about 60%. MRC is indicated in this situation. When a dominant stricture is identified, ERC with either balloon dilatation or short-term stenting is warranted. Whichever of these ERC methods is more effective is the topic of an ongoing multinational clinical trial.
Is PSC a premalignant condition?
CPUndoubtedly, PSC is a premalignant condition. Research by our collaborative Dutch PSC research group estimated that the risk of CCA within 30 years from diagnosis of comorbid PSC and ulcerative colitis amounts to about 20%. The risk of colorectal cancer within 30 years of diagnosis of comorbid PSC and ulcerative colitis is 15%. Patients with PSC also are at an increased risk for gallbladder carcinoma and hepatocellular carcinoma.
What is cholangitis syndrome?
Cholangitis syndromes are complex end-stage hepatobiliary disorders.1Given this broad concept, a wide range of abnormalities fall into the diagnostic criteria for cholangitis. These are generally associated with severe inflammation and fibrosis of the hepatobiliary system that is characterized by eventual narrowing and obstruction of the bile ducts.2Therapeutic interventions for obviating the obstructive lesions in biliary-hepatic ducts is the primary approach for management of cholangitis. Nevertheless, the only established curative therapy for cholangitis is liver transplantation, especially in patients with progressed disease.3New hopes are emerging, however, as improvements have been reported with therapies involving antibiotics and antifibrotic drugs.
What causes cholangitis in the bile duct?
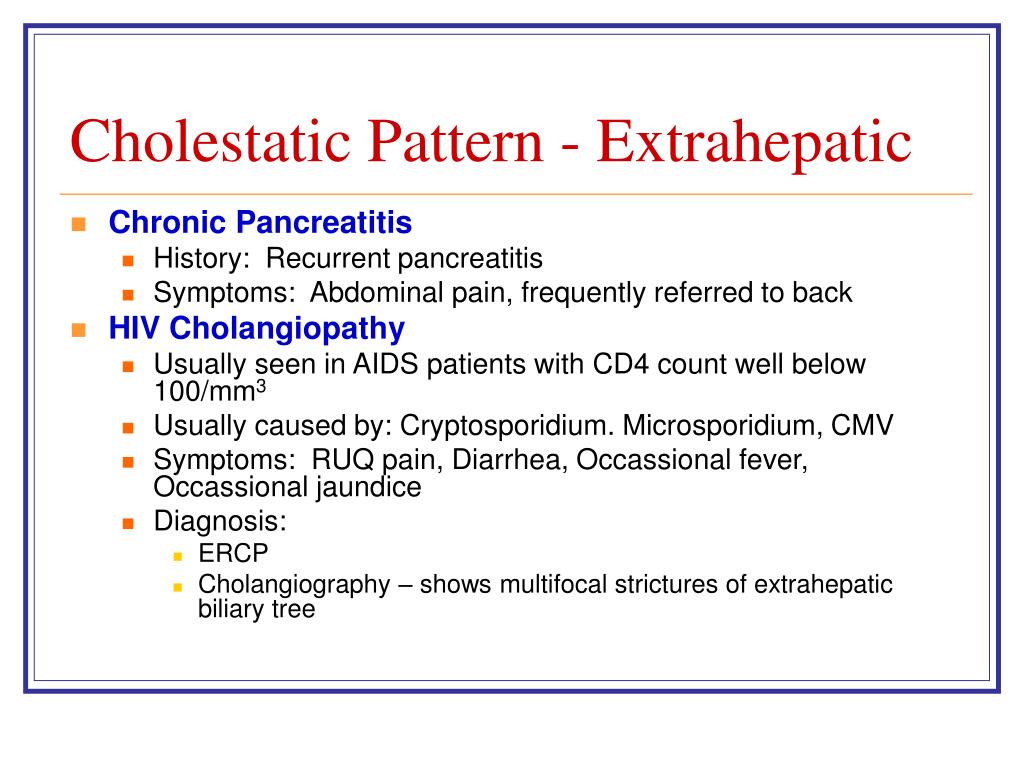
Bile stone and obstruction of the bile duct are considered the main causes for acute bacterial cholangitis.36In addition, bile duct obstruction in AC may also be triggered by other etiologies. Choledocholithiasis has been described among the most common etiologies for AC; nevertheless, this phenomenon is often accompanied by secondary bacterial infections within the biliary system.40Other etiologies include gallstones, malignancies (source being pancreas, gallbladder, cholangiocarcinoma, or metastatic tumors) or benign obstructions (surgical, pancreatitis, or chronic cholangitis), and some parasitic disorders.8In a survey of 31 patients, Gossard et al.41reported cholecystectomy, stones in bile ducts, chronic pancreatitis, and abdominal trauma as the causes for AC.
What is ERCP for cholangitis?
Instead of a diagnostic method, ERCP may also be performed as a therapeutic procedure for biliary drainage in cholangitis.51The role of biliary drainage procedures is of critical importance in the management of cholangitis. This approach provides a therapeutic alternative for patients who may not tolerate surgical drainage interventions.51ERCP-guided implantation of a biliary endoprosthesis or stent represents the gold standard therapeutic for biliary stricture.52This method is an effective therapeutic modality that can be tolerated even by elderly patients.51Therapeutic ERCP may be indicated when patients are in shock, show signs of nervous system involvement, or show coagulation defects.51Overall, other drainage procedures may be considered in cases in which ERCP is not possible, or under conditions for which ERCP is not available. Performing ERCP may not be feasible when there is pyloric or duodenal stenosis. ERCP may also fail if the catheter cannot be inserted properly or in patients with prior operations on the gastrointestinal tract.52
Is PSC a serious disease?
PSC is a serious disorder with yet unknown etiology ; however, a role has been proposed for immune dysregulation in the progression of PSC.4Bacterial infections secondary to bile fluid stasis may also complicate PSC.7On the other hand, the most common form of secondary cholangitis is acute cholangitis (AC; also known as recurrent pyogenic cholangitis, supportive cholangitis and ascending cholangitis). AC is characterized by infections involving the biliary system and leading to inflammation and obstruction of the biliary ducts.8,9Furthermore, the insidious role of the immune system has been highlighted in IgG4-associated cholangitis (IAC). Autoantibodies of IgA class that are reactive against biliary epithelial cell have been recently identified in IAC.10Nevertheless, the immune system may not be the sole contributor in IAC, as bile stones or bile duct abnormalities also have been related to occurrence of this condition.11
Is cholangitis a hepatobiliary disease?
Cholangitis is a serious life-threatening situation affecting the hepatobiliary system. This review provides an update regarding the clinical and pathological features of various forms of cholangitis. A comprehensive search was performed in the PubMed, Scopus, and Web of Knowledge databases. It was found that the etiology and pathogenesis of cholangitis are heterogeneous. Cholangitis can be categorized as primary sclerosing (PSC), secondary (acute) cholangitis, and a recently characterized form, known as IgG4-associated cholangitis (IAC). Roles of genetic and acquired factors have been noted in development of various forms of cholangitis. PSC commonly follows a chronic and progressive course that may terminate in hepatobiliary neoplasms. In particular, PSC commonly has been associated with inflammatory bowel disease. Bacterial infections are known as the most common cause for AC. On the other hand, IAC has been commonly encountered along with pancreatitis. Imaging evaluation of the hepatobiliary system has emerged as a crucial tool in the management of cholangitis. Endoscopic retrograde cholangiography, magnetic resonance cholangiopancreatography and endoscopic ultrasonography comprise three of the modalities that are frequently exploited as both diagnostic and therapeutic tools. Biliary drainage procedures using these methods is necessary for controlling the progression of cholangitis. Promising results have been reported for the role of antibiotic treatment in management of AC and PSC; however, immunosuppressive drugs have also rendered clinical responses in IAC. With respect to the high rate of complications, surgical interventions in patients with cholangitis are generally restricted to those patients in whom other therapeutic approaches have failed.
Is cholangitis a autoimmune disorder?
Cholangitis presentation may be observed in the context of a broader autoimmune disorder characterized with high levels of IgG4 in serum along with proliferation of lymphocytic populations positive for IgG4 (known as IgG4-related cholangitis).11,27Accordingly, IAC is characterized with infiltration of the biliary system with IgG4-positive lymphocytes.28Involvement of the bile ducts and pancreatitis are common features described in AIC. IAC is predominantly encountered in older individuals, and is mainly a feature of male subjects.27,29,30However, IAC has also been reported in children and adolescents;31the pathogenesis of this form of cholangitis is under investigation.
How long does it take for sclerosing cholangitis to progress?
PSC progresses slowly, but after roughly 10 to 15 years, it can lead to portal hypertension (high pressure in the blood vessels that drain into the liver) and cirrhosis (severe scarring of the liver), which in turn can result in liver failure. In some patients, PSC can lead to bile duct cancers. People who develop serious complications from PSC usually consider liver transplant surgery.
What is Primary Sclerosing Cholangitis (PSC)?
Primary sclerosing cholangitis (PSC) is an uncommon disease in which an overactive immune system attacks the bile ducts. Bile is an important digestive juice that is needed to break down fats and absorb vitamins A, D, E and K. It’s made in your liver and travels through thin tubes (called ducts) into your gallbladder and small intestine. With PSC, the bile ducts become inflamed and scarred, developing narrowed areas in the process and causing bile to back up into your liver. This can damage the liver.
What blood test can be used to determine if you have sclerosing cholangitis?
The diagnosis can be confirmed using one of several methods: Magnetic resonance cholangiopancreatography (MRCP).
What supplements can help with sclerosing cholangitis?
Vitamin supplements can help your body get the nutrients you need, including vitamins for bone health. Osteoporosis (brittle bones) is common in patients with primary sclerosing cholangitis, and your bone density needs to be monitored by your doctor.
When is sclerosing cholangitis diagnosed?
Primary sclerosing cholangitis is often diagnosed between the ages of 30 to 40, and it’s more common in men and patients with inflammatory bowel disease.
Can an overactive immune system cause sclerosing cholangitis?
It’s believed that an overactive immune system causes primary sclerosing cholangitis, but what triggers this over-activity still isn’t clearly known. A genetic predisposition for PSC likely exists, and exposure to certain bacteria, viruses or toxins is believed to somehow trigger the immune system, which reacts in an inappropriate way and causes injury to the bile ducts. Primary sclerosing cholangitis is often diagnosed between the ages of 30 to 40, and it’s more common in men and patients with inflammatory bowel disease.
Can bile ducts get worse over time?
If you do have symptoms, they may develop slowly, come and go, and may – or may not – get worse over time. Bile that backs up into your liver can cause cirrhosis, which can lead to liver failure. It can also lead to bile duct infections, and long term bile duct inflammation may lead to bile duct cancer. Common symptoms of primary sclerosing ...
What percentage of patients with PSC have cholangiocarcinoma?
Cholangiocarcinoma (cancer of the intra- and/or extrahepatic bile ducts) may develop in up to 10 to 15 percent of patients with PSC.
What are the complications of PSC?
The complications associated with PSC are recurrent cholangitis and bacteremia and cholangiocarcinoma.
What is PSC in the liver?
PSC is a chronic condition resulting from obstruction of bile flow in the liver because of inflammation and fibrosis of the bile ducts . The cause of PSC is unknown. Recent data support both genetic and acquired factors. The literature has described familial occurrence of both PSC and chronic ulcerative colitis.
What is the effect of PSC on bile ducts?
Whatever the mechanism of PSC, it results in inflammation of the bile ducts, which leads to fibrosis (scar tissue) resulting in strictures. The strictures can lead to elevations in bilirubin levels, recurrent cholangitis or pruritus. To relieve the obstruction, balloon dilation of the ducts may be performed.
What are the symptoms of PSC?
The symptoms of PSC are gradual onset of progressive fatigue and pruritus (itching) followed by jaundice. Fever and right upper quadrant pain are other manifestations. PSC may also be detected on routine blood tests during physical examinations.
Is observation a good prognosis?
If the patient has no symptoms and is in the early stages, as confirmed by liver biopsy, observation would be a reasonable choice. In this case the prognosis is very good and there is no specific therapy available.
Is colchicine a randomized controlled trial?
Agents such as cupruretic therapy, immunosuppressive therapy such as steroids, azathioprine, methotrexate and anti-fibrotic agents such as colchicine have not been shown to be effective in randomized control led trials.
What is the best treatment for end stage liver disease?
Liver transplantation is the best course of treatment for patients with end-stage liver disease. During liver transplantation , the diseased liver portion is removed and replaced with a healthy one. It is a long and complex surgery, and you need to take medications for the rest of your life to prevent your body from rejecting the organ.
Can you treat PCS with a sclerosing cholangitis?
Once a diagnosis of primary sclerosing cholangitis (PCS) is confirmed, you can begin treatment. There are a number of different treatment options for PCS, and your doctor will discuss with you the best course of treatment.
How long does it take to get a liver transplant after PSC?
Many people with PSC will ultimately need a liver transplant, typically about 10 years after being diagnosed with the disease. PSC may also lead to bile duct cancer. Endoscopy and MRI tests may be done to monitor the disease. If playback doesn't begin shortly, try restarting your device.
How long does it take for a PSC to progress?
Symptoms may remain at a stable level, they may come and go, or they may progress gradually. Liver failure may occur 10-15 years after diagnosis, but this may take even longer for some PSC patients.
Does cirrhosis cause liver to lose its function?
As cirrhosis progresses and the amount of scar tissue in the liver increases, the liver slowly loses its ability to function . The scar tissue may block drainage of the bile ducts leading to infection of the bile. PSC advances very slowly. Many patients may have the disease for years before symptoms develop.

Diagnosis
Treatment
Clinical Trials
Lifestyle and Home Remedies
Specialist to consult
Alternative Medicine
- Tests and procedures used to diagnose primary sclerosing cholangitis include: 1. Liver function blood test.A blood test to check your liver function, including levels of your liver enzymes, can give your doctor clues about your diagnosis. 2. MRI of your bile ducts.Magnetic resonance cholangiopancreatography (koh-lan-jee-o-pan-cree-uh-TOG-ruh-fee) uses magnetic resonance imaging (MRI) to make images of your liver and bile ducts and is the tes…
Preparing For Your Appointment
- Treatments for primary sclerosing cholangitis focus on managing complications and monitoring liver damage. Many medications have been studied in people with primary sclerosing cholangitis, but so far none have been found to slow or reverse the liver damage associated with this disease.