
Folinic acid (Leucovorin) intravenous infusion (I.V.), given over two hours before fluorouracil on Day 1 Oxaliplatin
Oxaliplatin
This medication is used to treat advanced cancer of the colon and rectum.
Folinic acid
Folinic acid, also known as leucovorin, is a medication used to decrease the toxic effects of methotrexate and pyrimethamine. It is also used in combination with 5-fluorouracil to treat colorectal cancer, may be used to treat folate deficiency that results in anemia, and methanol poisoning. It is t…
Full Answer
Can 5-Fluorouracil be used to treat colorectal cancer?
The liver is the most frequent site of metastases in colorectal cancer. Commonly used anticancer drugs in colorectal cancer are 5-fluorouracil, oxaliplatin and irinotecan 5-fluorouracil (5-FU) and oxaliplatin have very few numbers of studies that support their safety in hepatic dysfunction, but phar …
Is fluorouracil plus oxaliplatin an effective adjuvant for colon cancer?
The standard adjuvant treatment of colon cancer is fluorouracil plus leucovorin (FL). Oxaliplatin improves the efficacy of this combination in patients with metastatic colorectal cancer. We evaluated the efficacy of treatment with FL plus oxaliplatin in the postoperative adjuvant setting.
Can leucovorin and fluorouracil be taken together?
As a result fluorouracil may stay in the cancer cell longer and exert its anti-cancer effect on the cells. Leucovorin has almost no side effects of its own but when used in combination with fluorouracil it can increase the severity of side effects of that drug.
Is 5-fluorouracil (5-FU) safe in hepatic dysfunction?
Commonly used anticancer drugs in colorectal cancer are 5-fluorouracil, oxaliplatin and irinotecan 5-fluorouracil (5-FU) and oxaliplatin have very few numbers of studies that support their safety in hepatic dysfunction, but phar … The liver is the most frequent site of metastases in colorectal cancer.
Why is leucovorin given before 5-FU?
When given in combination with Leucovorin, Leucovorin can enhance the binding of fluorouracil to an enzyme inside of the cancer cells. As a result fluorouracil may stay in the cancer cell longer and exert its anti-cancer effect on the cells.
Why do you give leucovorin with oxaliplatin?
Adding oxaliplatin to a regimen of fluorouracil and leucovorin improves the adjuvant treatment of colon cancer.
Why is leucovorin given FOLFOX?
Often called "leucovorin rescue," it essentially saves the body from toxicity by providing another source of folic acid to those healthy cells in need over a required two- to three-day period of multiple doses.
How do I prepare for FOLFOX?
How To Prepare For FOLFOX InfusionsEat a large meal the night before treatment.Take an anti-nausea pill before sleep and another in the morning.Eat at least one hour before treatment - preferably foods that will minimize the effect in case you vomit. Scrambled eggs and toast are the choice for Karen B.
Is leucovorin compatible with oxaliplatin?
Oxaliplatin and Leucovorin should not be combined in the same infusion bag. Oxaliplatin is not compatible with normal saline. Do not piggyback or flush lines with normal saline. Leucovorin dose remains at 400 mg/m2 IV over 2 hours when concurrent oxaliplatin is omitted.
Why is folinic acid given with fluorouracil?
Folinic acid is often given with 5FU to treat cancers of the colon, rectum and other parts of the digestive system. It makes 5FU work better. It may also be given with tegafur-uracil which is a similar drug to 5FU. Folinic acid is sometimes given with methotrexate, which is used to treat different types of cancer.
When should leucovorin be administered?
Leucovorin comes as a tablet to take by mouth. It is usually taken every 6 hours until laboratory tests show it is no longer needed. Sometimes leucovorin is taken on a different schedule, depending on the reason it is needed. Take leucovorin at around the same time(s) every day.
When do you give leucovorin?
Leucovorin is also given with a chemotherapy agent called methotrexate, but in this case it is given to "rescue" normal, healthy cells from the damage caused by the methotrexate. In order to give the methotrexate time to kill the cancer cells, leucovorin is started 12-24 hours after the methotrexate is given.
How does leucovorin work with 5-FU?
5-Fluorouracil (5-Fu) and leucovorin (LV) are often given in combination to treat colorectal cancer. 5-Fu/LV prevents cell proliferation by inhibiting thymidylate synthase, which catalyzes the conversion of deoxyuridine monophosphate to deoxythymidine monophosphate.
Is FOLFOX and 5FU the same?
The drugs used in FOLFOX In this information, we call fluorouracil by its more common name, 5FU. Folinic acid is sometimes called calcium folinate or leucovorin. Folinic acid is not a chemotherapy drug, but is often given with 5FU to make it work better.
What is FOLFOX regime?
An abbreviation for a combination chemotherapy regimen that is used to treat colorectal cancer. It includes the drugs leucovorin calcium (folinic acid), fluorouracil, and oxaliplatin. There are several different FOLFOX regimens, including FOLFOX-4, FOLFOX-6, modified FOLFOX-6 (mFOLFOX-6), and FOLFOX-7.
Is FOLFOX strong chemo?
Chemotherapy medications such as FOLFOX are potent drugs. Although they kill harmful cancer cells, they can also damage healthy tissue and cause a range of side effects.
Can 5-FU be given without leucovorin?
Conclusion: Oxaliplatin/5-FU combination therapy without leucovorin achieved a relatively high response rate even in patients resistant to the previous 5-FU chemotherapy, and toxicity was minimal.
How does leucovorin help in a methotrexate overdose?
Leucovorin is in a class of medications called folic acid analogs. It works by protecting healthy cells from the effects of methotrexate or similar medications while allowing methotrexate to enter and kill cancer cells.
What are side effects of oxaliplatin?
Side EffectsDiarrhea, changes in taste, mouth sores, nosebleeds, tiredness, headache, dizziness, or trouble sleeping may occur. ... Temporary hair loss may rarely occur. ... Oxaliplatin can sometimes affect how your nerves work (peripheral neuropathy).More items...
What is the difference between FOLFOX and mFOLFOX6?
mFOLFOX6 is the code name of your colon or rectal cancer treatment regimen. mFOLFOX6 may also be used to treat other types of cancer. Most people call this regimen FOLFOX. A regimen is a combination of medications to treat cancer.
What is the phase 1 study of Folfox?
The goal of the Phase I part of this clinical research study is to find the highest tolerable dose of a combination of dasatinib, cetuximab, and FOLFOX (5-fluorouracil [5-FU], leucovorin [LV], and Eloxatin [oxaliplatin]) that can be given to patients with metastatic colorectal cancer. The safety of these drugs in combination will also be studied.
What to do before liver biopsy?
Before the liver biopsy, you will receive fluids and drugs for relaxation and/or pain through an needle in your arm or hand. You will be awake during the biopsy. A radiologist will find the tumor in the liver with the help of radiographic imaging procedures such as an ultrasound or CT scan.
What is the minimum number of prior regimens for metastatic colorectal cancer?
Patient must have previously progressed on systemic therapy for metastatic colorectal cancer, with no limit on the number of prior regimens. For patients in the Phase II cohort, they must have progressed on 5-FU or capecitabine and oxaliplatin [patients with KRAS mutated tumors], and either cetuximab or panitumumab [patients with KRAS wild type tumors].
How many tablespoons of blood is drawn for liver cancer?
A long, hollow needle will be inserted through the skin into the liver tumor, and a tissue sample (s) will be taken. On Day 8, blood (about 1-2 tablespoons) will be drawn for routine tests. You will have extra blood samples drawn (1 tablespoon each time) before receiving the study drugs and on Day 8 of Cycles 2 and 4.
Which drugs cause Torsades de Pointes?
Patients currently taking the following drugs that are generally accepted to have a risk of causing Torsades de Pointes:haloperidol, methadone, amiodarone, sotalol, erythromycins, clarithromycin cisapride, chlorpromazine, bepridil, droperidol, arsenic, chloroquine, domperidone, halofantrine, levomethadyl, pentamidine, sparfloxacin, lidoflazine, quinidine, procainamide, disopyramide, ibutilide, dofetilide. Subjects who have discontinued any of these medications must have a wash-out of at least 5 days (or 14 days for amiodarone) prior to the first dose of dasatinib.
Does dasatinib slow down EGFR?
Blocking EGFR may stop or slow the growth of tumor cells . Dasatinib is a drug that inhibits a protein called c-Src. High levels of c-Src may make it harder for chemotherapy to work against the cancer. If dasatinib can inhibit c-Src, the chemotherapy may be more effective against the cancer.
Can you take a diary while taking Dasatinib?
In this diary, you will write down the date, the time, and the number of dasatinib tablets taken. Certain drugs and herbal supplements may not be taken while you are receiving dasatinib.
What anticancer drugs are used for colorectal cancer?
Commonly used anticancer drugs in colorectal cancer are 5-fluorouracil, oxaliplatin and irinotecan 5-fluorouracil (5- FU) and oxaliplatin have very few numbers of studies that support their safety in hepatic dysfunction, but phar …. The liver is the most frequent site of metastases in colorectal cancer.
Is 5-fluorouracil leucovorin safe for liver cancer?
Severe liver dysfunction and safe use of 5-fluorouracil leucovorin and oxaliplatin in one patient with metastatic colorectal carcinoma. The liver is the most frequent site of metastases in colorectal cancer. Commonly used anticancer drugs in colorectal cancer are 5-fluorouracil, oxaliplatin and irinotecan 5-fluorouracil (5-FU) ...
What is leucovorin given with methotrexate?
When given in combination with methotrexate, Leucovorin is given to lessen the side effects of methotrexate (see methotrexate).
How long does it take for leucovorin to work after methotrexate?
Leucovorin is normally started 24 hours after methotrexate is given. This delay gives the methotrexate a chance to exert its anti-cancer effects.
How does leucovorin work?
How Leucovorin Works: Leucovorin is a compound similar to folic acid, which is a necessary vitamin. It has been around and in use for many decades. Leucovorin is a medication frequently used in combination with the chemotherapy drugs fluoruracil and methotrexate. Leucovorin is not a chemotherapy drug itself, however it is used in addition ...
What is leucovorin used for?
What Leucovorin Is Used For: In combination with fluoruracil to treat cancers such as; colon and rectal, head and neck, esophageal, and other cancers of the gastrointestinal tract. As an antidote to effects of certain chemotherapy drugs such as methotrexate. Treatment of megaloblastic anemia when folic acid deficiency is present.
Can leucovorin be given in combination with fluorouracil?
Important things to remember about the side effects of Leucovorin: The side effects with treatment of Leucovorin are likely attributable to other chemotherapy medications being given in combination with Leucovorin. When given in combination with fluorouracil (5-FU) the side effects of fluorouracil may be more severe (see fluorocuracil).
Is leucovorin a folic acid?
Leucovorin is a reduced folic acid. Leucovorin is used in combination with other chemotherapy drugs to either enhance effectiveness, or as a "chemoprotectant" (For more detail, see "How Leucovorin Works" section below).
Does fluorouracil stay in the body?
Fluorouracil when given alone stays in the body for only a short time. When given in combination with Leucovorin, Leucovorin can enhance the binding of fluorouracil to an enzyme inside of the cancer cells. As a result fluorouracil may stay in the cancer cell longer and exert its anti-cancer effect on the cells.
What is the best adjuvant treatment for stage 3 colon cancer?
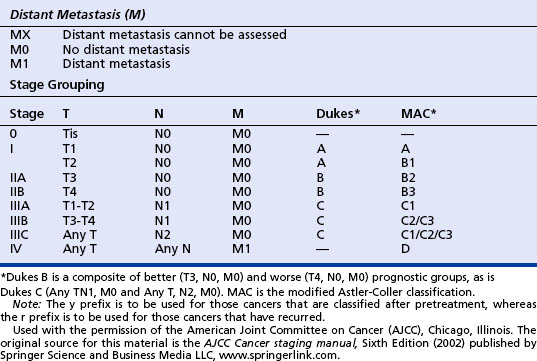
The demonstration that postoperative adjuvant treatment with fluorouracil and levamisole reduced the mortality rate by 33 percent among patients with stage III colon cancer 4 prompted several trials, which established six months of treatment with fluorouracil plus leucovorin (FL) as the standard adjuvant chemotherapy for stage III colon cancer. 5-11 Oxaliplatin is a third-generation platinum derivative, which, when combined with fluorouracil and leucovorin, is among the most effective chemotherapies for metastatic colorectal cancer. 12-15 To determine whether oxaliplatin can also benefit patients with disease in an earlier stage, we conducted an international phase 3 clinical trial in patients with stage II or III colon cancer — the Multicenter International Study of Oxaliplatin/5-Fluorouracil/Leucovorin in the Adjuvant Treatment of Colon Cancer (MOSAIC).
What is the hazard ratio for recurrence in the group given FL plus oxalip?
The hazard ratio for recurrence in the group given FL plus oxaliplatin, as compared with the FL group, was 0.77 (95 percent confidence interval, 0.65 to 0.91; P=0.002).
What is the interaction test for colon cancer?
A test for interaction is an appropriate statistical approach to the question of whether the benefit of adjuvant treatment differs between stage II and stage III colorectal cancer. 23 In our study, this test showed no significant interaction between the stage of disease and the treatment, indicating that FL plus oxaliplatin benefited both stage II and stage III colorectal cancer. From a clinical standpoint, stage II colon cancer occurs in a heterogeneous, node-negative population in which clinical and biologic prognostic factors other than the status of lymph-node involvement need to be taken into account. Tools are being developed to help physicians assess the risk–benefit ratio of adjuvant chemotherapies for individual patients. 22
What is the best treatment for colon cancer?
The standard adjuvant treatment of colon cancer is fluorouracil plus leucovorin (FL). Oxaliplatin improves the efficacy of this combination in patients with metastatic colorectal cancer. We evaluated the efficacy of treatment with FL plus oxaliplatin in the postoperative adjuvant setting.
How long is a FL infusion?
Eligible patients were randomly assigned to receive FL alone or with oxaliplatin. In the FL group, each cycle comprised a 2-hour infusion of 200 mg of leucovorin per square meter of body-surface area followed by a bolus of 400 mg of fluorouracil per square meter and then a 22-hour infusion of 600 mg of fluorouracil per square meter given on 2 consecutive days every 14 days, for 12 cycles. In the group given FL plus oxaliplatin, the same FL regimen was used, plus a two-hour infusion of 85 mg of oxaliplatin (Eloxatin, Sanofi-Synthelabo) per square meter on day 1, given simultaneously with leucovorin, with the use of a Y infusion device. The use of disposable pumps (LV5 infusors, Baxter Healthcare) allowed outpatients to receive a continuous infusion of fluorouracil.
What are the adverse effects of oxaliplatin?
Neutropenia, diarrhea, and vomiting were the most frequent grade 3 or 4 adverse effects in the group given FL plus oxaliplatin ( Table 2 ). Grade 3 or 4 neutropenia was much commoner with FL plus oxaliplatin than with FL (41.1 percent vs. 4.7 percent, P<0.001) but was complicated by fever or infection in only 1.8 percent of cases (20 patients) in the group given FL plus oxaliplatin and in 0.2 percent of cases (2 patients) in the FL group (P<0.001). The incidence of thromboembolic events among patients who received at least one cycle of the assigned regimen was similar in the two groups (63 of 1108 patients [5.7 percent] and 72 of 1111 patients [6.5 percent], respectively).
How often are patients assessed for chemo?
Patients were assessed before randomization, every two weeks during treatment, and then every six months for five years. The baseline assessment involved a medical history taking, physical examination, biologic tests, measurement of the carcinoembryonic antigen level, chest radiography, and abdominal ultrasonography or computed tomography. Patients were monitored for adverse effects throughout the treatment period and until 28 days after the last cycle of chemotherapy, unless treatment-related adverse effects required additional follow-up.
How is the FOLFOX regimen given?
The FOLFOX regimen is an intravenous (IV) infusion, meaning it’s slowly given directly in a vein. Most of the FOLFOX medications should be given at an infusion center, either at an oncologist's (cancer specialist’s) office or at a hospital. This is because a healthcare provider or nurse will very closely watch you for allergic reactions and side effects during your infusion.
What type of cancer does FOLFOX treat?
The most common type of cancer that FOLFOX is used for is colorectal cancer. However, it may also be used for other cancers, such as:
What does FOLFOX stand for?
FOLFOX is an abbreviation. It stands for the three medications that make up this chemotherapy regimen. Those medications include:
What are the side effects of FOLFOX chemotherapy?
Everyone tolerates chemotherapy differently. There may be some who don’t experience many side effects and others who experience a lot. Below we’ll discuss potential side effects of each FOLFOX medication. Be sure to let your oncologist know what you experience after your treatments.
What is the best chemotherapy for colorectal cancer?
A common chemotherapy regimen used for colorectal cancer is FOLFOX.
How long does it take for Folfox to cure cancer?
In the MOSAIC trial discussed earlier, 78% of participants using FOLFOX had disease-free survival after 3 years of using the regimen. This means there was no sign of cancer for 3 years after completing FOLFOX treatment. Researchers also noted that using FOLFOX lowered the risk of cancer returning by 23% compared to only using 5-FU and leucovorin.
Does Folfox slow the spread of cancer?
In the MOSAIC trial, FOLFOX slowed the growth and spread of cancer cells more effectively for people with stage 3 colorectal cancer than the combination of 5-FU and leucovorin. It wasn’t as helpful for people with stage 2 colorectal cancer.
5-Flourouracil
Colon and rectal cancer. Breast cancer. Gastrointestinal cancers including: anal, esphageal, pancreas and gastric (stomach). Head and neck cancer * Hepatoma (liver cancer). Ovarian cancer. Topical use (cream or solution) in basal cell cancer of the skin and actinic keratoses. -see document fluorouracil (cream).
Leucovorin
In combination with fluoruracil to treat cancers such as; colon and rectal, head and neck, esophageal, and other cancers of the gastrointestinal tract.
Oxaliplatin
Oxaliplatin is used to treat colon or rectal cancer that has spread (metastasized), it is often given in combination with other anticancer drugs (fluorouracil and leucovorin).
