Futile treatment is treatment that has only a very low chance of achieving meaningful benefit for the patient in terms of:
- improving quality of life;
- sufficiently prolonging life of acceptable quality; or
- bringing benefits that outweigh the burdens of treatment.
Full Answer
When is a treatment futile?
Hippocrates clearly stated that physicians should “refuse to treat those who are overmastered by their disease, realizing that in such cases medicine is powerless.” 1 Webster's dictionary defines futile as “serving no useful purpose, completely ineffective.” 2 The word futile refers to a specific action, whereas futility is the relationship between an action and a desired goal.
What is “futility” in medicine?
Feb 16, 2020 · Futile or non-beneficial treatment is not defined in law, but is often used to describe treatment which is of no benefit, cannot achieve its purpose, or is not in the person’s best interests. Health professionals generally decide whether particular treatment for a person is futile or non-beneficial.
How can we overcome the need for medical futility?
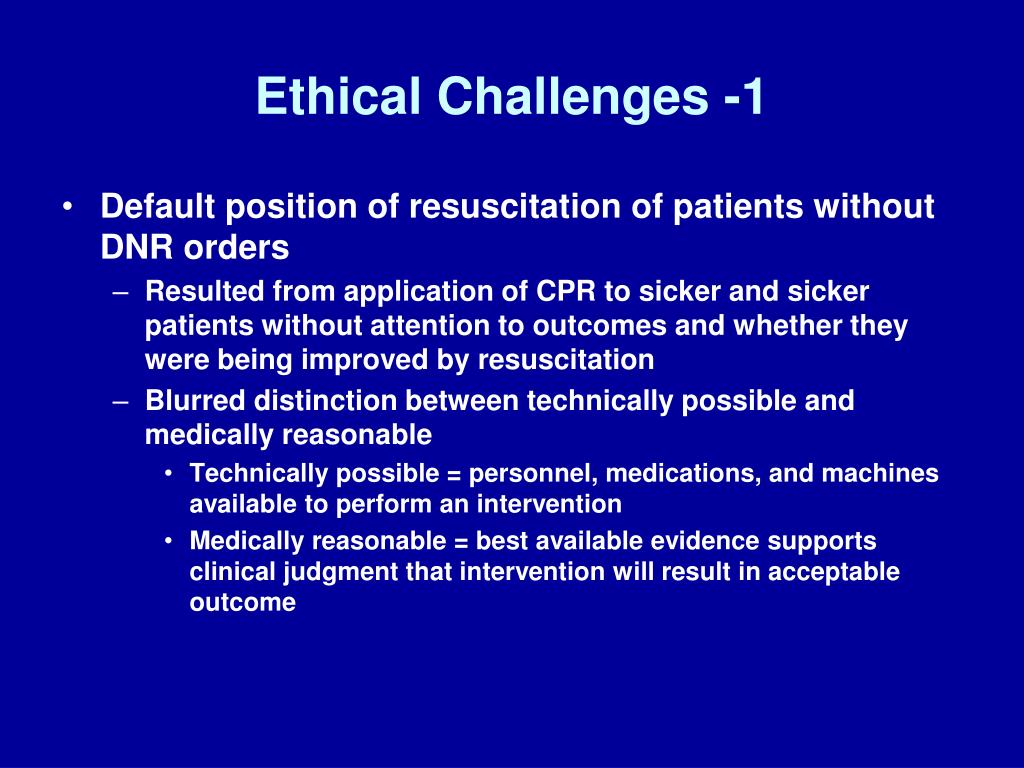
Medical futility means that the proposed therapy should not be performed because available data show that it will not improve the patient's medical condition. Medical futility remains ethically controversial for several reasons. Some physicians summarily claim a treatment is futile without knowing the relevant outcome data.
Is it legal for a doctor to offer futile interventions?
Feb 11, 2007 · Most medical ethicists and scholars define a medically futile situation as one in which interventions are extremely unlikely to produce a significant patient benefit. A medically futile treatment is commonly defined as one that: • won’t achieve the patient’s intended goal (if known) • serves no legitimate goal of medical practice

What is the meaning of futile treatment?
Futile treatment is treatment that has only a very low chance of achieving meaningful benefit for the patient in terms of: improving quality of life; sufficiently prolonging life of acceptable quality; or. bringing benefits that outweigh the burdens of treatment.May 2, 2016
What is a futile case?
Futile treatment. “An action, intervention or procedure that might be physiologically effective in a given case but cannot benefit the patient, no matter how often it is repeated.Oct 20, 2016
What is futile nursing care?
Futile care was defined as useless and inconclusive care, leading to the squandering of financial resources and patient/nurse discomfort, with both nursing and medical aspects.Mar 25, 2016
What is a futile state?
Medical futility means that the proposed therapy should not be performed because available data show that it will not improve the patient's medical condition. Medical futility remains ethically controversial for several reasons.
When should a medical treatment be considered futile?
“Futility means any treatment that, within a reasonable degree of medical certainty, is seen to be without benefit to the patient, as when the treatment at issue is seen as ineffective with regard to a clinical problem that it would ordinarily be used to treat.”
Is it ethical to provide futile treatment?
If a physician believes, after carefully onsidering the patient's medical status, values and goals, that a particular medical treatment is futile because it violates the principles of beneficence and justice, then the physician is ethically and professionally obligated to resist administering this treatment.
What is in the Hippocratic oath?
Hippocratic Oath: One of the oldest binding documents in history, the Oath written by Hippocrates is still held sacred by physicians: to treat the ill to the best of one's ability, to preserve a patient's privacy, to teach the secrets of medicine to the next generation, and so on.Jun 3, 2021
What is confidentiality in nursing?
As a nurse, midwife or nursing associate, you owe a duty of confidentiality to all those who are receiving care. This includes making sure that they are informed about their care and that information about them is shared appropriately.Jan 29, 2015
How is medical futility determined?
Who decides when a particular treatment is futile? Generally the term medical futility applies when, based on medical data and professional experience, a treating health care provider determines that an intervention is no longer beneficial.
What is the difference between withholding and withdrawing treatment?
Such decisions can essentially take one of two forms: withdrawing – the removal of a therapy that has been started in an attempt to sustain life but is not, or is no longer, effective – and withholding – the decision not to make further therapeutic interventions.Mar 4, 2005
What is medical abandonment?
Abandonment is considered a breach of duty and is defined as unilateral termination of the physician-patient relationship without providing adequate notice for the patient to obtain substitute medical care.Oct 9, 2021
Would you recommend or give life sustaining therapy when you judge that it's futile?
In surveying physicians, Medscape researchers asked, "Would you ever recommend or give life-sustaining therapy when you judged that it was futile?" Nearly 5300 physicians answered the question: 23.6% said yes, they would recommend or continue to give care they knew to be futile, while 37.0% said they would not.Nov 16, 2010
What is medical futility?
Medical futility: definition, determination, and disputes in critical care. Physicians may employ the concept of medical futility to justify a decision not to pursue certain treatments that may be requested or demanded by patients or surrogates. Medical futility means that the proposed therapy should not be performed because available data show ...
Is medical futility ethical?
Medical futility remains ethically controversial for several reasons. Some physicians summarily claim a treatment is futile without knowing the relevant outcome data. There is no unanimity regarding the statistical threshold for a treatment to be considered futile.
What are the responsibilities of a nurse?
The International Code of Ethics for Nurses states that nurses have four fundamental responsibilities—encouraging health, preventing disease, returning patients to health, and alleviating pain and distress.
What is the role of healthcare providers?
Healthcare providers, for their part, are obligated to act in the patient’s best interests. They must uphold their professional duty to relieve suffering and help maintain the patient’s dignity. But they’re not obligated professionally, legally, or ethically to offer futile interventions. Defining medical futility.
What is futility in medicine?
"Medical futility" refers to interventions that are unlikely to produce any significant benefit for the patient. Two kinds of medical futility are often distinguished: 1 Quantitative futility, where the likelihood that an intervention will benefit the patient is exceedingly poor, and 2 Qualitative futility, where the quality of benefit an intervention will produce is exceedingly poor.
What is medical futility?
What is "medical futility"? "Medical futility" refers to interventions that are unlikely to produce any significant benefit for the patient. Two kinds of medical futility are often distinguished: Quantitative futility, where the likelihood that an intervention will benefit the patient is exceedingly poor, and.
What is UW Dept of Bioethics and Humanities?
of Bioethics & Humanities is in the process of updating all Ethics in Medicine articles for attentiveness to the issues of equity, diversity, and inclusion. Please check back soon for updates!
What is qualitative futility?
Qualitative futility, where the quality of benefit an intervention will produce is exceedingly poor. Both quantitative and qualitative futility refer to the prospect that a specific treatment will benefit (not simply have a physiological effect) on the patient.
What is the ethical authority of a physician?
While physicians have the ethical authority to withhold or withdraw medically futile interventions, communicating with professional colleagues involved in a patient’s care, and with patients and family , greatly improves the experience and outcome for all.
In Brief
Confusion surrounds the concept of medical futility. Conflicts persist as to how to determine what's really futile in particular circumstances.
Agreeing on guidelines
Perhaps it's less important for nurses and healthcare organizations to agree upon an absolute definition and more meaningful to determine workable guidelines and a process for addressing medical futility.
Communicating conditions
Understanding medical futility isn't limited to the development of a model for medical futility. Equally important is crucial communication, which should occur early on in the patient's care, between the healthcare team, the patient, and the family.
REFERENCES
1. Angelucci P. Grasping the concept of medical futility. Nurs Manage. 2006;37 (2):12–14.
What is futile treatment?
What is already known on this topic 1 Futile treatment at the end of life is an entrenched problem in Western industrialised healthcare systems that can cause harm to patients, moral distress to clinicians and that wastes scarce health resources. 2 The empirical research on the drivers of futile treatment is limited, but suggests that patient and family request, concerns about legal risk, doctors' professional desire to cure patients and doctors' poor communication skills are all contributors. 3 Existing findings are inconsistent regarding the main drivers of futility.
What is objective futile treatment?
Objective Futile treatment, which by definition cannot benefit a patient, is undesirable. This research investigated why doctors believe that treatment that they consider to be futile is sometimes provided at the end of a patient's life.
What is multicentre ethics?
Multicentre ethics approval for all participating sites was obtained, and the research was approved by the human research ethics committees of the relevant universities. Participants were given the opportunity to review their transcript and request amendments. Due to the small size of the medical community from which the participants were drawn, extra care was taken with the use of direct quotes to ensure that no comment could be attributed to an individual.