First-line treatments for urinary tract infection include nitrofurantoin, fosfomycin, and trimethoprim-sulfamethoxazole (when resistance levels are <20%). These antibiotics have minimal collateral damage and resistance. In pregnancy, beta-lactams, nitrofurantoin, fosfomycin, and trimethoprim-sulfamethoxazole can be appropriate treatments.
Are antibiotics safe for UTI in pregnancy?
UTIs were thought to be common and high risk in pregnancy, which meant that antibiotics were viewed as essential in the presence of suspected symptoms. The dominant view about antibiotics was that their use was safe and of little concern in pregnancy. Women reported an emotional reaction to developing a UTI.
How do you treat an uti during pregnancy?
- Recognize that some symptoms of a UTI can seem common to a regular pregnancy, like urinating frequently and having a backache. ...
- Sometimes you might not have any symptoms from a UTI, so be sure to see your doctor regularly during pregnancy so you can be screened.
- Consider keeping a diary of how you’re feeling during your pregnancy. ...
Is nitrofurantoin safe during pregnancy?
Women might take nitrofurantoin in pregnancy to treat urinary tract infections. The safety of taking nitrofurantoin in pregnancy generally depends upon the stage of gestation. Historically, there has not been evidence indicating that the drug will harm the fetus during most phases of pregnancy.
What antibiotics can cause an uti?
- You underwent multiple UTI treatments in your lifetime
- If you have been using the same antibiotic for previous infections
- Stopped taking antibiotics and didn’t finish all the pills that your doctor prescribed you
- If you are guilty of keeping a stash of antibiotics and self-treating UTIs, cold, travel diarrhea, etc.
- You’ve been recently hospitalized
What antibiotics are used for UTI?
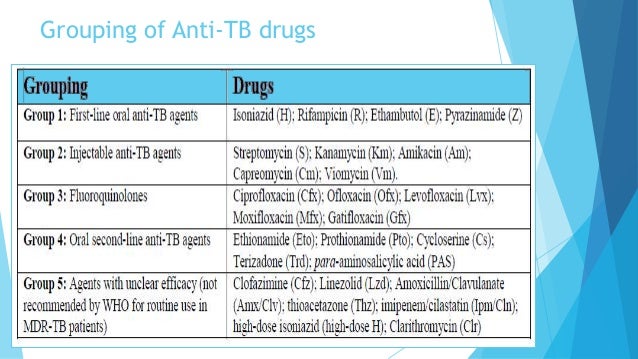
Other antibiotics used to treat UTI include: 1 Beta-lactams, including penicillins and cephalosporins ( amoxicillin, Augmentin, Keflex, Duricef, Ceftin, Lorabid, Rocephin, Cephalexin, Suprax and others). Many organisms have shown resistance to some of these drugs. 2 Trimethoprim-sulfamethoxazole combination antibiotic (Bactrim DS and Septra DS). Many organisms have shown resistance to some of these drugs. 3 Fluoroquinolones ( Cipro, Levaquin and Floxin). The risk of antibiotic resistance to this is developing. These should not be given to pregnant women or children. 4 Tetracyclines (Sumycin, Vibramycin or Minocin) are used for Mycoplasma or Chlamydia infections. These should not be given to pregnant women or children. 5 Aminoglycosides (gentamicin, amikacin and tobramycin) are usually used in combination with other antibiotics to treat severe UTIs. 6 Macrolides ( clarithromycin, azithromycin and erythromycin) are often used to treat urinary problems caused by sexually transmitted diseases. 7 Fosfomycin ( Monurol) is a synthetic phosphonic acid derivative and used for acute cystitis but not for more complicated UTIs.
What is the UTI in the urinary tract?
Urinary Tract Infection (UTI) A urinary tract infection (UTI) is an infection of the bladder, kidneys, ureters, or urethra. E. coli, a type of bacteria that lives in the bowel and near the anus, causes most UTIs. UTI symptoms include pain, abdominal pain, mild fever, urinary urgency and frequency.
What are the symptoms of a UTI in a child?
Urinary Tract Infections in Children. Urinary tract infections (UTIs) are very common in children. Symptoms and signs include fever and abdominal pain. Associated symptoms and signs include flank pain, vomiting , and blood in the urine. Treatment for a UTI involves antibiotic therapy.
Can pregnant women take fluoroquinolone?
Fluoroquinolones (Cipro, Levaquinand Floxin). The risk of antibiotic resistance to this is developing. These should not be given to pregnantwomen or children. Tetracyclines (Sumycin, Vibramycinor Minocin) are used for Mycoplasma or Chlamydiainfections.
How many pregnant women have UTI?
In this study, about 1 in 10 pregnant women had a diagnosis of a UTI just before or during pregnancy.
What is the CDC treating for two?
Through Treating for Two, CDC is working with its partners, other federal agencies, and the public to understand trends in medicine use among pregnant women and women of reproductive age, and to provide women and healthcare providers with information about the safety or risk of using specific medicines during pregnancy.
Can ACOG prescribe antibiotics to pregnant women?
Healthcare providers of various specialties should be familiar with ACOG’s recommendations about prescribing specific antibiotics to pregnant women and consider the possibility of early pregnancy when treating women of reproductive age.
Can you take antibiotics while pregnant?
Some antibiotic treatments for urinary tract infections (UTIs), such as nitrofurantoin and trimethoprim-sulfamethoxazole, have been linked to birth defects. The American College of Obstetricians and Gynecologists (ACOG) recommends avoiding these antibiotic treatments in early pregnancy if possible. A study from the Centers for Disease Control and Prevention (CDC) found that about 4 in 10 women with UTIs during early pregnancy filled a prescription for nitrofurantoin or trimethoprim-sulfamethoxazole. Healthcare providers of various specialties should be familiar with ACOG’s recommendations about prescribing specific antibiotics to pregnant women and consider the possibility of early pregnancy when treating women of reproductive age. To help determine treatment options, women should inform all of their healthcare providers if they are pregnant or are planning to become pregnant.
How to treat UTI while pregnant?
How do you treat a UTI when pregnant? It’s similar to how you treat a UTI when not pregnant — with a few key differences. A short-course of antibiotics is the standard treatment for asymptomatic and symptomatic urinary tract infections that occur during pregnancy. There are, however, two important contrasts in treating UTIs in pregnant women versus nonpregnant women. First, asymptomatic UTIs diagnosed during the first trimester are treated with antibiotics, whereas nonpregnant women’s infections are often not treated in this manner. (Outside of pregnancy, asymptomatic bacteriuria is usually not treated with antibiotics.) Also, the preferred antibiotic drugs used to treat UTI in pregnancy often differ than what would be used while not pregnant. For instance, the following antibiotics have not been associated with any birth defects, thus are likely safe to use at any point during pregnancy:
What are the signs of a UTI during pregnancy?
After all, research suggests that about 18 percent of UTIs that occur during pregnancy are symptomatic UTIs, meaning the telltale UTI signs and symptoms are present: Strong and frequent urge to use the bathroom. Burning while urinating. Regularly passing only small amounts of urine.
What is the chance of a woman having pyelonephritis?
Research published in the American Journal of Obstetrics & Gynecology notes that women diagnosed with acute pyelonephritis in pregnancy have a 10.3 percent chance of preterm delivery compared with the 7.9 percent chance among women without a kidney infection during pregnancy. RELATED: Common Types of Vaginal Infections.
How to tell if you have a UTI?
Typical Signs of a Symptomatic UTI 1 High-grade fever 2 Chills and rigors (sudden feeling of cold with shivering) 3 Headache 4 Nausea or vomiting 5 Lower back pain 6 Flank pain (often right side) 7 Possible reduced urine output
What causes painful urination during pregnancy?
UTIs occur when bacteria enters into the usually sterile urinary tract and multiplies, causing painful urination and other symptoms. Certain factors during pregnancy make this occurrence more likely to happen. Here’s what you need to know to keep you and your baby healthy.
Why is it so hard to empty your bladder while pregnant?
When you’re pregnant, the anatomy of your urinary tract actually changes. For instance, your kidneys become larger and your growing uterus can compress your ureters and bladder. Because of this compression, fully emptying your bladder during pregnancy becomes more difficult.
When does the UTI go up?
Your risk of UTI goes up beginning at week 6 of your pregnancy; the chances you’ll have a UTI vary by trimester.
How many pregnant women have cystitis?
Approximately 1–4 % of pregnant women experience acute cystitis and the incidence of asymptomatic bacteriuria during pregnancy ranges from 2–10 %. 1. Many factors may contribute to the development of UTIs during pregnancy. One important factor is ureteral dilatation, thought to occur due to hormonal effects and mechanical compression from ...
What antibiotics are used for bacteriuria?
It is recommended that all pregnant women who have confirmed asymptomatic bacteriuria are treated with antibiotics. The choice of antibiotic can be guided by the known sensitivities, in the following order of preference: 1,8 1 Amoxicillin (if susceptible): 250 mg three times a day 2 Nitrofurantoin: 50 mg four times a day (avoid at 36+ weeks) 3 Trimethoprim: 300 mg once a day (avoid in the first trimester) 4 Cephalexin: 500 mg twice a day (least preferred option)
How long should antibiotics be given?
All antibiotics should be given for seven days to ensure cure. A recent study found that a one day course of nitrofurantoin is less effective than a seven day course for treating asymptomatic bacteriuria in pregnant women. 9 A repeat culture one to two weeks after completing therapy is required to ensure eradication of bacteriuria. It is then recommended that urine cultures are repeated regularly until delivery. 1,5 Women who do not have bacteriuria in the first screen (i.e. at 12 to 16 weeks gestation) do not need to have repeat urine cultures. 7
How long does it take to cure cystitis?
A seven day treatment period is required to ensure eradication. Studies in non-pregnant women with acute cystitis show that treatment with antibiotics for three days is as effective as longer courses (e.g. seven to ten days), however, the risk of relapse is higher. 4 Recurrent infections may have serious consequences for pregnant women therefore a longer course of antibiotics is used to avoid the higher rate of relapse with short courses. 4 A follow up urine culture can be requested one to two weeks after the antibiotic course has been completed to ensure eradication.
Why is ureteral dilation important?
One important factor is ureteral dilatation, thought to occur due to hormonal effects and mechanical compression from the growing uterus. Ureteral dilation can cause bacteria to spread from the bladder to the kidneys, increasing the risk of pyelonephritis. 2.
When should a urine culture be done?
A urine culture should be used to screen for asymptomatic bacteriuria at 12 to 16 weeks gestation. 3,7 While some guidelines recommend a second urine culture to confirm bacteriuria prior to treatment, 7 in clinical practice it is common for only one culture to be done. 2.
What is the best medicine for cystitis?
Paracetamol can be used to relieve pain associated with acute cystitis. 5 Other measures to relieve symptoms such as increasing fluid intake, urinary alkalinisation products and cranberry products are not recommended because evidence of their effectiveness is lacking and some products may interact with antibiotic treatment. 1
What is UTI in pregnancy?
Urinary tract infections (UTIs) are common in pregnant women and pose a great therapeutic challenge, since the risk of serious complications in both the mother and her child is high. Pregnancy is a state associated with physiological, structural and functional urinary tract changes which promote ascending infections from the urethra. Unlike the general population, all pregnant women should be screened for bacteriuria with urine culture, and asymptomatic bacteriuria must be treated in every case that is diagnosed, as it is an important risk factor for pyelonephritis in this population. The antibiotic chosen should have a good maternal and fetal safety profile. In this paper, current principles of diagnosis and management of UTI in pregnancy are reviewed, and the main problems and controversies are identified and discussed.
What are the most common pathogens that cause infections during pregnancy?
The pathogens responsible for infections during pregnancy are similar to those in the general population. Most infections are caused by Enterobacteriaceae, commonly found in the gastrointestinal tract, with Escherichia coliresponsible for 63–85% of cases, and among the remaining: Klebsiella pneumoniae(∼8%), coagulase-negative Staphylococcus(up to 15%), S. aureus(up to 8%), and group B streptococci (GBS) (2–7%) [16, 17, 24–26].
Is bacteriuria asymptomatic in pregnancy?
According to recommendations developed by the IDSA (Infectious Diseases Society of America), significant bacteriuria in asymptomatic women is defined as bacterial monoculture in the quantity of ≥ 105colony-forming units (CFU) per ml in two consecutive mid-stream clean-catch urine specimens or ≥ 102CFU/ml in urine collected from single urinary bladder catheterization [76]. However, for practical and economic reasons the guidelines for routine screening in pregnancy accept a single urine culture taken between weeks 12 and 16, or at first prenatal visit (if later), although there is only an 80% probability that the woman has true bacteriuria (vs. 95% with the original criteria) [9, 77]. Due to this high rate of false positive results, in some centers women with a positive urine culture are asked to return within 1 week for the second testing, to avoid unnecessary treatment [11].
Can bacteriuria be acquired before pregnancy?
Many women acquire bacteriuria before pregnancy [18, 19] . A large retrospective analysis with logistic regression modeling, embracing 8037 women from North Carolina, revealed that the two strongest predictors of bacteriuria at prenatal care at prenatal care initiation were: UTI prior to prenatal care initiation (OR = 2.5, 95% CI: 0.6–9.8 for whites, and OR = 8.8, 95% CI: 3.8–20.3 for blacks) and a pre-pregnancy history of UTI (OR = 2.1, 95% CI: 1.4–3.2) [19]. In a second analysis, prior antenatal UTI was found to be the strongest predictor of pyelonephritis after 20 weeks’ gestation (OR = 5.3, 95% CI: 2.6–11.0) [20]. Other suggested risk factors for UTI during pregnancy are lower socioeconomic status, sexual activity, older age, multiparity, anatomical urinary tract abnormalities, sickle cell disease and diabetes, although the significance of some of them (age, parity or sickle cell trait) remains a matter of controversy [1, 10, 21–23].
Is nitrofurantoin safe during pregnancy?
Nitrofurantoin and trimethoprim/sulfamethoxazole should be avoided during the first trimester due to a possible risk of fetal defects, although the studies on that issue yield somewhat contradictory results [1, 51–53]. In the large American population-based National Birth Defects Prevention Study, maternal use of sulfonamides and nitrofurantoin (1 month before pregnancy to the end of the first trimester) was associated with more serious defects than any other antibacterial classes [51]. However, this study has been criticized for several significant limitations including recall bias (women were asked about antibiotic use after pregnancy and it was not confirmed by medical records), inability to determine whether the birth defect was due to the antibiotic itself, the infection for which the antibiotic was prescribed, or other confounding factors. Two years later, the Committee of Obstetrics Practice of the American College of Obstetricians and Gynecologists, summarizing the available data on the relationship between prenatal exposure to both antimicrobials and birth defects, concluded that: 1) “When selecting an antibiotic for a true infection during the first trimester of pregnancy (that is, during organogenesis), health care providers should consider and discuss with patients the benefits as well as the potential unknown risks of teratogenesis and maternal adverse reactions; 2) “Prescribing sulfonamides or nitrofurantoin in the first trimester is still considered appropriate when no other suitable alternative antibiotics are available”; 3) “Pregnant women should not be denied appropriate treatment for infections because untreated infections can commonly lead to serious maternal and fetal complications” [52]. Recently Nordeng et al. published the results from a large population-based cohort study using the Norwegian Prescription Database linked to data on all live births, stillbirths, and induced abortions after 12 weeks of gestation from the Medical Birth Registry of Norway [53]. Among 180 120 pregnancies between 2004 and 2008, 1334 women filled prescriptions for nitrofurantoin in the first trimester. The authors found that dispensing nitrofurantoin during the first trimester was not associated with increased risk of major malformations (OR = 0.79, 95% CI: 0.51–1.23) or higher rates of stillbirth, neonatal death, low birth weight, or preterm delivery.
Is UTI a risk factor for preterm birth?
The frequency of preterm deliveries in women with acute pyelonephritis is significantly higher than in women free of this complication, and pyelonephritis seems to be an important independent risk factor for delivery before 37 weeks’ gestation [2, 5, 47]. However, again, a substantial heterogeneity between these studies, together with many possible biases, makes it difficult to establish the overall contribution of UTI to preterm birth [48]. A rare but severe complication is the transmission of the infection onto the newborn baby [49]. Very often the transmitted infection originates from a heavily colonized birth canal, usually with GBS [26].
Is fluoroquinolone used during pregnancy?
The use of fluoroquinolones (FDA pregnancy category C) is essentially contraindicated throughout pregnancy, since fetal cartilage development disorders have been reported in experimental animals, although not in human studies [27, 60–63]. In the largest study so far, 200 pregnant women exposed to fluoroquinolones were compared to 200 women exposed to nonteratogenic, nonembryotoxic antimicrobials, matched by indication, duration of therapy (∼3 days), and trimester of exposure [60]. The rate of major congenital malformations did not differ between the group exposed to quinolones in the first trimester and the control group (2.2% vs. 2.6%; RR = 0.85; 95% CI: 0.21–3.49) and was within the expected normal range (1–5%). A systemic review of prospective, controlled studies showed that the use of fluoroquinolones during the first trimester of pregnancy does not appear to be associated with an increased risk of major malformations recognized after birth, stillbirths, preterm births or low birth weight [64]. Apparently more data are needed to establish safety of fluoroquinolones in pregnancy before they may be routinely prescribed. However, in some cases of complicated symptomatic UTI, resistant to other antibiotics, their benefits may outweigh the risks [60].
What is the diagnosis of UTI?
All UTI cases can be classified as either asymptomatic or symptomatic. An asymptomatic UTI is diagnosed based on urinalysis results. Careful sample collection is crucial given the external urethral opening position in women. The number of leukocytes is the key criterion utilized in UTI diagnosis; a count > 10 leukocytes/mm3suggests an infection. In pregnant patients the cut-off is higher, at > 20 leukocytes/mm3. Sample contamination by vaginal secretions containing mucus and lactic acid bacteria may result in erroneous diagnosis of multiple mucus threads and abundant bacterial growth in urine sediment. Sometimes the mucus even yields a mistaken diagnosis of proteinuria. Period, postpartum bleeding, or any other uterine bleeding may result in sample contamination with red blood cells. In such cases, a detailed history and a better-prepared repeat analysis is necessary. Urinalysis results not accompanied by the patient’s symptoms are not sufficient to initiate treatment. A urine culture can be used to confirm or disprove a hypothesis of an UTI. The culture sample should be collected in a sterile container to avoid contamination, preferably from first morning urine. The presence of ≥ 105colony forming units per millilitre (CFU/mL) confirms an infection, while an antibiogram will help verify the efficacy of a given treatment.
What is a UTI?
Urinary tract infection (UTI) is one of the most common infections afflicting women. UTI often accompanies vaginal infections and is frequently caused by pathogens originating in the digestive tract. The paper discusses the prevalence of UTI in various patient populations, including postmenopausal, pregnant, diabetic, epileptic, ...
Why are women more prone to UTIs than men?
Women are much more prone to UTIs than men, mainly due to the female lower urinary tract anatomy and its proximity to the reproductive organs.
Why do women get UTIs?
The main reasons behind the increased prevalence of urinary tract infections in peri- and postmenopausal women include hormonal changes (oestrogen insufficiency) and connective tissue aging (urinary incontinence, pelvic organ prolapse). Factors conducive to UTIs in the perimenopausal period include urinary incontinence (impeding proper hygiene), atrophy of vaginal mucous membranes (increasing the risk of vaginal infections that may spread into the urinary tract), and anterior vaginal prolapse (precluding complete voiding of the bladder). Prevalence of asymptomatic bacteriuria increases in the peri- and postmenopausal period, reaching levels of 4–19% as compared to 1.5% in premenopausal women [12]. In peri- and postmenopausal women, oestrogen deficiency may be conducive to both urinary incontinence and urinary tract infections. Topical vaginal (but not systemic) application of oestrogens was proven to significantly reduce the risk of bacteriuria (OR = 0.3; 95% CI: 0.13–0.68) [13]. The recommendation of topical oestrogen use in peri- and postmenopausal patients to prevent UTIs is also included in guidelines published by research associations [14].
How long does a urinary tract infection treatment last?
Outside of pregnancy, a 3-day treatment course is as effective as 5-day or 10-day courses. In older women , the treatment may continue for 3 to 6 days.
How often should you take a urine culture for cystitis?
In the case of cystitis in the patient’s history, repeat urine cultures should be taken every 1–2 months. Fluoroquinolones are contraindicated throughout the pregnancy, and co-trimoxazole should not be used in the first trimester. Conclusions. Urinary tract infection is one of the most common infections afflicting women.
Is diabetes mellitus a risk factor for UTIs?
Diabetes mellitus, uncontrolled in particular, is a risk factor for both urinary and reproductive tract infections (involving the vulva, vulvar vestibule, and/or vagina). Fourteen per cent of women with type 1 diabetes and 23% of women with type 2 diabetes are diagnosed with UTIs [18].
What is the first line of treatment for urinary tract infection?
First-line treatments for urinary tract infection include nitrofurantoin, fosfomycin, and trimethoprim-sulfamethoxazole (when resistance levels are <20%). These antibiotics have minimal collateral damage and resistance. In pregnancy, beta-lactams, nitrofurantoin , fosfomycin, and trimethoprim-sulfamethoxazole can be appropriate treatments.
What is the most common outpatient infection?
Urinary tract infections are the most common outpatient infections, but predicting the probability of urinary tract infections through symptoms and test results can be complex.
Can a urinary culture be used to detect bacteriuria?
Urine culture is the gold standard for detection of urinary tract infection. However, asymptomatic bacteriuria is common, particularly in older women, and should not be treated with antibiotics. Conversely, in symptomatic women, even growth as low as 10 2 colony-forming unit/mL could reflect infection.
Does positive urine test increase the chance of infection?
Positive testing may increase the probability of urinary tract infection , but initiation of treatment should take into account risk of urinary tract infection based on symptoms as well. In cases in which the probability of urinary tract infection is moderate or unclear, urine culture should be performed. Urine culture is the gold standard ...
Does a negative dipstick urinalysis rule out a urinary tract infection?
In patients with a high probability of urinary tract infection based on symptoms, negative dipstick urinalysis does not rule out urinary tract infection. Nitrites are likely more sensitive and specific than other dipstick components for urinary tract infection, particularly in the elderly.
