D9110 - Palliative (Emergency) Treatment of Dental Pain
- This is typically used when a patient is seen for an emergency dental appointment, and something is painful or uncomfortable.
- Palliative can be thought of as easing the symptoms without curing the underlying condition.
- This is not appropriate to use when the only service provided to the patient is writing of a prescription. ...
What is palliative care, and who can benefit from it?
Jul 31, 2019 · Palliative emergency medicine, defined as the integration of palliative care principles into emergency medicine practice, places the patient back at the center of care, eliciting the person’s own values, concerns, and decisions.
What is the difference between palliative care and hospice?
Attention in this article is focussed on medical treatment. In the care of the emergency event, however, and in all palliative care, management includes making the patient comfortable, thinking of the needs of other patients and relatives observing the event, explaining what is happening and is being done, involving other members of the team, and communicating reassurance to the …
Is palliative care the same thing as hospice?
Sep 03, 2016 · Definition of Palliative Care Palliative care is the relief of symptoms including pain that interferes with the quality of life. Whether patients have cancer or heart failure, they have already been undergoing noncurative symptom management in addition to …
What is the difference between euthanasia and palliative care?
May 01, 2020 · Training in palliative care for EM has in the past been limited; while most clinical staff are well versed in how to manage death following sudden catastrophic events such as cardiac arrest or trauma, there is less focus on managing patients who have chronic illness with limited life expectancy who present in crisis.

What is emergency palliative care?
Palliative care emergencies are emergencies in patients with an incurable disease that may lead to death or decreased quality of life.
How is palliative care given?
Where palliative care is given. Palliative care is most often given to the patient in the home as an outpatient, or during a short-term hospital admission. Even though the palliative care team is often based in a hospital or clinic, it's becoming more common for it to be based in the outpatient setting.May 10, 2019
What are palliative symptoms?
Palliative care – dealing with common symptomsCommon symptoms at end of life may include pain, constipation, nausea, breathlessness, fatigue and delirium.Relieving these symptoms is a key aim of palliative care.More items...•Feb 13, 2017
What is dental Code D9110?
Procedure code D9110 - Palliative (emergency) treatment of dental pain- minor procedure. Palliative treatment in conjunction with root canal therapy by the same dental office is included in the fee for the root canal and is not separately billable.Oct 1, 2012
What are the 3 forms of palliative care?
Areas where palliative care can help. Palliative treatments vary widely and often include: ... Social. You might find it hard to talk with your loved ones or caregivers about how you feel or what you are going through. ... Emotional. ... Spiritual. ... Mental. ... Financial. ... Physical. ... Palliative care after cancer treatment.More items...
What are the 5 stages of palliative care?
What are the five stages of palliative care?Stage 1: Creating a plan. This is when your initial care plan is created. ... Stage 2: Preparing emotionally. ... Stage 3: Early stage care. ... Stage four: Late stage care.
When does palliative care start?
Palliative care is available when you first learn you have a life-limiting (terminal) illness. You might be able to receive palliative care while you are still receiving other therapies to treat your condition. End of life care is a form of palliative care you receive when you're close to the end of life.
Can palliative care be done at home?
In Alberta, you have many options for where to get palliative and end-of-life care—your home, a hospital, a continuing care centre, or a hospice. Talk to your family and your health care team about what's important to you and where you'd like to be at this time in your illness.
What is the most common symptom experienced in palliative care?
Pain and difficulty in breathing are two of the most frequent and serious symptoms experienced by patients in need of palliative care.Aug 5, 2020
What is dental palliative?
Palliative care is typically known to be something done to relieve pain or alleviate a problem without dealing with the underlying cause. D9110 palliative (emergency) treatment of dental pain - minor procedure. This is typically reported on a per-visit basis for emergency treatment of dental pain.
How long does a sedative filling last?
If we used anesthetic, avoid or be very careful chewing or eating hot foods until the numbness has worn off completely so that you do not bite or burn yourself. The numbing in the upper jaw will last approximately 1 hour, and the numbing in the lower jaw will last up to 4 hours.Jun 18, 2020
Can you bill D0140 and D9110 together?
D0140 is a stand-alone code and may always be reported in conjunction with D9110.
What are the emergency situations in palliative care?
Emergencies in palliative care also include sudden severe exacerbation of symptoms. Therefore, onset of severe pain, exacerbation of breathlessness, and worsening of other symptoms are also discussed with their appropriate treatment.
What are the five groups of events that are considered emergencies in palliative care?
Five groups of events are here considered as emergencies in palliative care: haemorrhage, convulsions, fractures, spinal cord compression and acute confusion . Incidence, causes and management of these form the major part of this article. Emergencies in palliative care also include sudden severe exacerbation of symptoms. Therefore, onset of severe pain, exacerbation of breathlessness, and worsening of other symptoms are also discussed with their appropriate treatment. A small armamentarium of appropriate medications is thus shown to cover treatment of the various emergencies that may arise. As palliative care deals with patients who are suffering from progressive fatal conditions, death is the expected end. Nevertheless, however well the family are prepared, death often appears for them as an emergency. Comment is made regarding this family emergency in the care of terminally ill people. Attention in this article is focussed on medical treatment. In the care of the emergency event, however, and in all palliative care, management includes making the patient comfortable, thinking of the needs of other patients and relatives observing the event, explaining what is happening and is being done, involving other members of the team, and communicating reassurance to the patient and the relatives as well as to other observers.
What is a small armamentarium?
A small armamentarium of appropriate medications is thus shown to cover treatment of the various emergencies that may arise. As palliative care deals with patients who are suffering from progressive fatal conditions, death is the expected end.
What is EM in medical terms?
cardiac arrest. Emergency medicine (EM) is the front door for people in crisis and this remains true for those of all ages and for crises that are medical, psychological and social. We know that people use more healthcare including unscheduled care in their last years of life 1 so it is predictable that patients with limited life expectancy will ...
What is EM in healthcare?
Emergency medicine (EM) is the front door for people in crisis and this remains true for those of all ages and for crises that are medical, psychological and social. We know that people use more healthcare including unscheduled care in their last years of life 1 so it is predictable that patients with limited life expectancy will present to the ED in crisis.
What are the barriers to good care in Mughal 7?
Staff needs must be considered in any learning intervention planned. Mughal 7 also found that the environment of the ED, and the increased resources needed to provide end of life care, including an appropriate place and time for communication, were barriers to good care.
What did Mughal 7 discover about nurses?
Mughal 7 in the systematic review of attitudes and responses of nurses in providing end of life care in the ED, discovered that two distinct emotional responses. Nurses described doing their best out of a sense of duty, or avoiding the situation due to a sense of overwhelming emotional burden.
What is palliative care?
The WHO defines Palliative Care as “an approach that improves the quality of life ofpatients and their families facing the problems associated with life-threatening illness,through the prevention and relief of suffering by means of early identification andimpeccable assessment and treatment of pain and other problems, physical, psycho-social and spiritual.”21A patient does not need to be at the end of their life to be acandidate for palliative care.
Why are opioids used in palliative care?
Opioids are a mainstay treatment for dyspnea in palliative care because they diminishrespiratory drive in response to hypoxia and hypercapnia. A Cochrane Review ofopioids for dyspnea supports the use of oral and parenteral opioids for dyspnea inadvanced disease.42Opioids have the added benefit of treating pain and anxiety,which are contributors to suffering during periods of breathlessness.43A peripheralmechanism acting on lung parenchyma also exists, inhibiting the bronchoconstrictive
What is the best treatment for dyspnea at the end of life?
The most commonly used therapies for dyspnea at the end of life are oxygen, opioids,and noninvasive positive pressure ventilation. A “distress protocol” (DP) for acute res-piratory emergencies in terminally ill patients has also been proposed.
What are the symptoms of end of life?
End-of-life symptoms can be extremely distressing and at times unbearable. Respira-tory distress, intractable pain, and severe hemorrhage are some of the most trauma-tizing symptoms for patients and their families, and unfortunately, are very common atthe end of life. Palliative sedation is defined as using medications to lessen patientconsciousness for the purpose of limiting intractable and intolerable suffering.47It ison the spectrum of palliative and hospice care and is an appropriate therapy toconsider in very specific circumstances.
What is hospice care?
Hospice care is care focused on symptom relief at the end of life and is mostcommonly provided for patients with a life expectancy of 6 months or less. Accordingto the National Hospice and Palliative Care Organization, hospice care is defined as “ateam-oriented approach to expert medical care, pain management, and emotionaland spiritual support expressly tailored to the patient’s needs and wishes. Supportis provided to the patient’s loved ones as well.”23The Medicare Hospice Benefits booklet (updated in January 2015) explains hospicefurther: “When you choose hospice care, you’ve decided that you no longer want careto cure your terminal illness and related conditions, and/or your doctor has determinedthat efforts to cure your illness aren’t working.” Once hospice care is chosen, Medi-care ceases to pay for a multitude of health care related costs, including care in anemergency room (unless visit is unrelated to the terminal illness or related condition;
What is the end of life?
An obstacle when discussing issues surrounding the “end of life” is the lack of acoherent, widely accepted definition of this term. It can be defined by diagnosis,prognostic criteria, symptom expression, hospice eligibility, and other factors. Lorenzand colleagues22propose that “the broadest approach to ‘end-of-life’ refers to a chro-nologically indefinite part of life when patients and their caregivers are struggling withthe implications ( eg, symptoms, practical support needs) of an advanced chronicillness.” Most commonly, the terms “end-of-life care” and “hospice care” areinterchangeable.
What is the POLST program?
The National POLST Paradigm is an approach to advanced care planning thatprovides patients and their families an opportunity to guide EM personnel actions .A POLST is a medium by which detailed plan about end-of-life care can be commu-nicated. Essentially, it gives specific and actionable details of the care that the patientwould or would not like to receive at the end of life. POLST complements advancedirectives and is not meant to replace it. The POLST form is filled out by a physicianafter a conversation with patient and their family and is meant to guide treatmentthat the patient wants to have carried out.20There is substantial variation among different states in the United States regardingPOLST. As of 2015, there are only 5 states that do not have some form of POLST:Alabama, Alaska, Arkansas, Nebraska, and South Dakota. Not only does the nameof the program vary (ie, POLST, MOLST, MOST, TPOPP, LaPOST, POST, COLST),but the structure of each program has a lot of variation as well. The POLST website,www.polst.orgis the primary resource to find out more about POLST in each individualstate.
How many people walk after palliative radiotherapy?
After palliative radiotherapy, 70% of patients who were ambulatory at the start of treatment retain their ability to walk and 35% of paraparetic patients regain their ability to walk, while only 5% of completely paraplegic patients do so.
How long does it take for lung cancer to heal from radiotherapy?
In non-small cell lung cancer palliative radiotherapy gives symptomatic improvement in 70% of patients, with a median duration of palliation of three months. Up to 17% of patients may survive for a year. If radiotherapy is contraindicated or being awaited corticosteroids alone (dexamethasone 16 mg/day) may give relief.
What are the factors that cause hypercalcaemia?
The pathology of hypercalcaemia is mediated by factors such as parathyroid related protein, prostaglandins, and local interaction by cytokines such as interleukin 1 and tumour necrosis factor. Bone metastases are commonly but not invariably present.
What causes cord damage?
In 85% of cases cord damage arises from extension of a vertebral body metastasis into the epidural space, but other mechanisms of damage include vertebral collapse, direct spread of tumour through the intervertebral foramen (usually in lymphoma or testicular tumour), and interruption of the vascular supply.
How long does it take for normocalcaemia to go away after bisphosphonate?
Always consider treating the underlying malignancy to prevent recurrence of symptoms, since the median duration of normocalcaemia after bisphosphonate infusion is only three weeks.
What is rapid assessment?
The concept of rapid assessment, evaluation, and management of symptoms due to malignancy is generally accepted. Inherent in this concept is rapid reversal of what is reversible. Some acute events in malignancy have to be treated as an emergency if a favourable outcome is to be achieved. As in any emergency, the assessment must be as prompt ...
What does a plain radiology examination reveal?
In patients unfit to undergo more detailed investigations, plain radiology can reveal erosion of the pedicles, vertebral collapse, and, occasionally, a large paravertebral mass.
How to monitor what gets done?
The only way to monitor what gets done is with daily stats especially for your weak areas. For example, one employee should be specifically responsible for calls to patients who are unscheduled, overdue for re-care or need reactivation. Other staff can and should help in coordination with the accountable employee.
What is D9110 dental?
D9110 - Palliative (Emergency) Treatment of Dental Pain. This is typically used when a patient is seen for an emergency dental appointment, and something is painful or uncomfortable. Palliative can be thought of as easing the symptoms without curing the underlying condition.
What do practice owners lack in knowledge?
What most practice owners are lack in knowledge is not how to book an appointment, but rather how to be an effective leader. The best systems in the world are useless if the staff do not comply. Good leaders know how to get staff to willingly follow through and comply.
Does palliative care include x-rays?
Palliative treatment does not include diagnostic x-rays. Although not stated in the CDT code, a narrative is helpful in determining the nature of the treatment, and documenting that it is congruent with CDT descriptor. Examples of palliative treatment: Smoothing of a sharp edge on a broken tooth or restoration.
What is treatment in medical terms?
treatment. 1. the management and care of a patient; see also care. 2. the combating of a disease or disorder; called also therapy. Schematic of the treatment planning process using occupational therapy as an example.
What is conservative treatment?
conservative treatment treatment designed to avoid radical medical therapeutic measures or operative procedures. empiric treatment treatment by means that experience has proved to be beneficial. expectant treatment treatment directed toward relief of untoward symptoms, leaving the cure of the disease to natural forces.
Why did Neanderthals use toothpicks?
Neanderthals used 'toothpicks to alleviate pain of gum disease' . "Although studies with a control group are missing, the improvement in symptoms should push the use of cannabis in the practice of oncology palliative treatment ," the report concluded. Study: Cannabis beneficial to cancer patients.
What is rape trauma treatment?
rape-trauma treatment in the nursing interventions classification, a nursing intervention defined as the provision of emotional and physical support immediately following a reported rape. rational treatment that based upon knowledge of disease and the action of the remedies given. refusal of treatment see under refusal.
What is a T in the OMAHA system?
t's and procedures in the omaha system, a term used at the first level of the intervention scheme defined as technical nursing activities directed toward preventing signs and symptoms, identifying risk factors and early signs and symptoms, and decreasing or alleviating signs and symptoms.
What is extraordinary treatment?
extraordinary treatment a type of treatment that is usually highly invasive and might be considered burdensome to the patient; the effort to decide what is extraordinary raises numerous ethical questions.
What is substance use treatment?
substance use treatment in the nursing interventions classification, a nursing intervention defined as supportive care of patient/family members with physical and psychosocial problems associated with the use of alcohol or drugs. See also substance abuse.
How to deal with palliative care?
When dealing with an emergency in palliative care: 1 try to stay calm 2 call for help 3 clearly explain what's happening to the patient and any family, friends or carers who are there 4 tell any family or friends who are not there about the emergency, if appropriate.
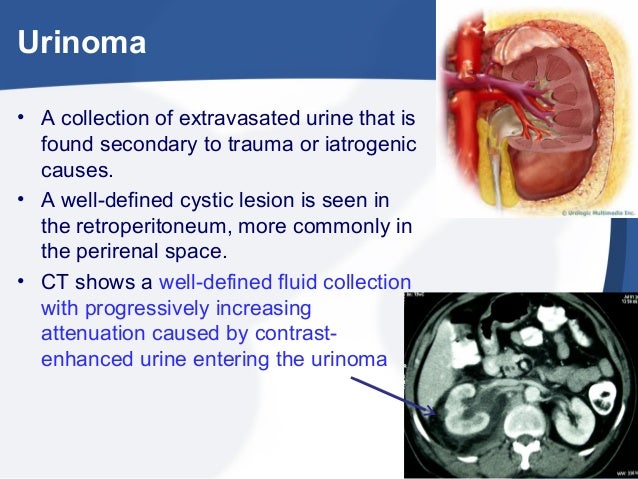
What are clinical emergencies?
Clinical emergencies can happen suddenly in palliative and end of life care. Without urgent medical attention, they can affect a patient's health and quality of life. They can also be very distressing for patients and those around them.
Why do people with advanced disease have a higher risk of other medical emergencies?
This may be because the effects of the disease mean their body is less able to respond to stress and illness. Other symptoms that may not need medical treatment but do need urgent care include: spiritual distress.