Why should psychologists be culturally competent?
- Is cultural competency better conceptualized as a concrete skill that can be learned by anyone or as a complex process that depends on social interactions?
- Can a theoretical model be devised that explains cultural competency and why it works?
- Why do research findings on the effects of culturally competent interventions show so much variability?
Why is cultural sensitivity training important for all of US?
There are many reasons to consider sensitivity training in the organization and the most important reason is that it helps in raising awareness of the cultural differences among the employees. They are trained to become more empathetic and understanding towards everyone working in the company.
Why positive thinking is very important to survive cancer?
Positive Thinking With Cancer – Ingrid’s Story and Some Tips You Can Try
- Before Positive Thinking: Pessimism and Cancer. Until her diagnosis Ingrid had been a pessimist; she would never have categorized herself as someone who maintained positive thinking through cancer.
- Positive Thinking Influenced Her Cancer: The Pursuit of Happiness. ...
- One Small Practice Inspired A Shift To Positive Thinking. ...
Why being proactive is so important?
The Importance of Being Proactive
- Lack of Prioritization /Misprioritization. A lot of us have probably experienced a time when we had several projects due within a short timeframe.
- Procrastination. This is another big issue that most people struggle with it. ...
- Time Management. This is sort of like an overarching theme with the first 2 points. ...
- Having a Reactive Mindset. ...
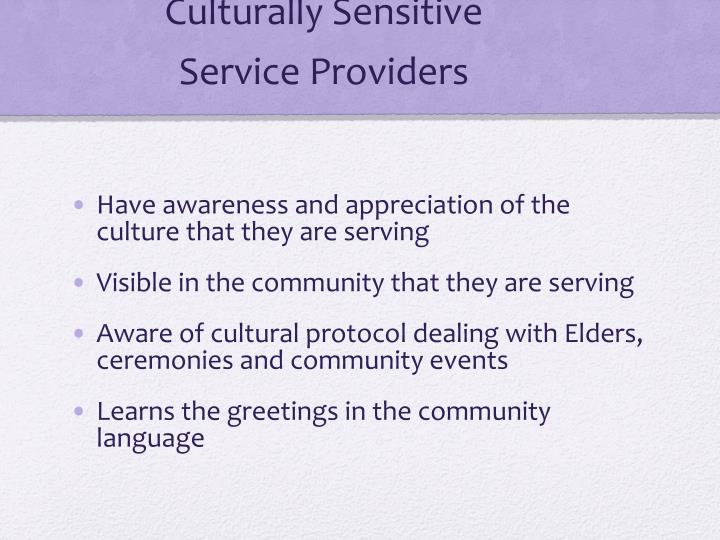
What is meant by culturally sensitive care?
Culturally sensitive health care has been described as care that reflects “the ability to be appropriately responsive to the attitudes, feelings, or circumstances of groups of people that share a common and distinctive racial, national, religious, linguistic, or cultural heritage” (DHHS, OMH, 2001, p.
What is an example of being culturally sensitive?
Example: People who seamlessly interact with others from different cultures by following the norms of that culture. They feel that they can respect their own values while adapting to the values of other cultures they interact with. They use empathy effectively.
What is culturally responsive treatment?
Culturally responsive therapy refers to a counseling relationship in which a client and a therapist are of different ethnicities, cultures, races, and backgrounds and the therapist (1) evidences awareness of the significance of both his and the client's cultural stories, (2) has spe- cific knowledge of the client's ...
How can a therapist be culturally sensitive?
Cultural Competence A culturally competent therapist should recognize and respect the beliefs, perspectives, and values of clients from a particular race, ethnicity, or region. A culturally sensitive therapist should be confident in their knowledge and skills.
What 4 factors affect cultural sensitivity?
Certain factors can affect cultural sensitivity. These factors include religion, ethnicity(race), national origin(language), or gender.
Why is it important to be culturally sensitive?
Cultural sensitivity is important because it allows us to effectively function in other cultures, allows us to respect and value other cultures, and can reduce cultural barriers between professionals and their patients.
How do you provide culturally competent therapy?
What Would Make Therapists More Culturally Competent?Stop saying that people of color do not seek mental health services. ... Address race in therapy sessions. ... Don't rely on a translator. ... Update the therapeutic method to a person's culture.
What are some culturally sensitive considerations in assessment?
different expectations of required skills, based on different experiences with assessment. different pedagogic paradigms, leading to different understandings of assessment. lack of clarity about the target of the course and the intended learning outcomes. communication style and language skill differences.
How do you ask a culturally sensitive question?
10 Questions to Ask a Client with a Diverse Cultural BackgroundWhat was your experience growing up in your family, and in what ways has this impacted your view of family and parenting today? ... What country are you originally from, and why did you move to the U.S.?More items...
What is the most important aspect of culturally sensitive human services practice?
Displaying empathy and compassion by fostering mutual respect between the worker and the client is the foundation of any Human Services practice. As such, cultural competence is an integral component in this process.
What is culturally responsive mental health?
Cultivating culturally responsive mental health care means fostering an environment where clients are fully seen in all aspects of their identity through a holistic and anti-oppressive approach to therapy.
Why are cultural issues important in psychotherapy?
Acknowledging the role of culture in psychotherapy is important because it helps to frame specific expectations and customs within the psychotherapy experience. There are also expansive ways and approaches in psychotherapy that take into account varying cultural ways of being and understandings of health and healing.
What are examples of cultural issues?
These are some of the most common cultural differences that can cause issues in the workplace.Religion. ... Ethnicity. ... Sexual Orientation and Gender Identity. ... Education. ... Generation. ... Cultural Behavior. ... Educational Clash. ... Ensure Effective Communication.More items...
What is cultural sensitivity in the workplace?
Cultural sensitivity is a set of skills that enables us to learn about and understand people who are different from ourselves, thereby becoming better able to serve them within their own communities.
How can I be more culturally sensitive in my classroom?
To incorporate cultural awareness into your classroom curriculum, you should:Express interest in the ethnic background of your students. ... Redirect your role in the classroom from instructor to facilitator. ... Maintain a strict level of sensitivity to language concerns. ... Maintain high expectations for student performance.More items...•
What are some examples of cultural competence?
For example, educators who respect diversity and are culturally competent:have an understanding of, and honour, the histories, cultures, languages, traditions, child rearing practices.value children's different capacities and abilities.respect differences in families' home lives.More items...•
Why is culturally sensitive care important?
Providing culturally sensitive care is an important component of patient centered-care. Nurses must strive to enhance their ability to provide patient-centered care by reflecting on how their and the patient’s culture’s, values, and beliefs impact the nurse-patient relationship. The nurse also must understand how bio-psychosocial needs ...
What are some strategies I can use to reflect on my own cultural beliefs and values?
You are encouraged to reflect continually on your and your patients’ cultural beliefs and values to determine if or how they impact the care you provide. Such reflection assist in providing patient-centred, culturally sensitive care.
What is patient centered care?
Partnering with patients and providing culturally sensitive care are important components of patient centered-care. You are accountable for discussing with your patients, your and your patient’s roles in achieving the care plan’s desired goal. You also must ensure you are sharing nursing knowledge with patients and promoting the best care possible.
What is therapeutic nurse-patient relationship?
A therapeutic nurse-patient relationship is based on meaningful communication. When communication barriers exist, you are responsible for using communication strategies and skills so the patient is an informed partner in the care provision. Interpreters are essential when a nurse-patient language barrier exists.
What is the nurse's commitment to patient-centred care?
The nurse’s commitment to patient-centred care as outlined in the practice standard, Therapeutic Nurse-Client Relationship, Revised 2006, outlines ways of meeting the patient’s needs within the hospital setting limits. The nurse meets the practice standard, Professional Standards, Revised 2002 by collaborating with their manager and other colleagues, and determining how to fulfill the patient’s needs without exposing other patients to discomfort or risk.
What is the best way to achieve common understanding?
Achieving a common understanding requires considering how the patient perceives you or the situation and making attempts to correct any misperceptions.
Do interpreters have to maintain confidentiality?
You are obliged to maintain confidentiality and protect personal health information as outlined in the practice standard Confidentiality and Privacy: Personal Health Information. Interpreters, by virtue of their role, gain access to personal health information and also are bound by confidentiality. To help the patient feel comfortable with the interpreter, you should inform the patient that confidential information is shared only within the health care team.
What is culturally sensitive care?
Culturally sensitive health care has been described as care that reflects “the ability to be appropriately responsive to the attitudes, feelings, or circumstances of groups of people that share a common and distinctive racial, national, religious, linguistic, or cultural heritage ” (DHHS, OMH, 2001, p. 131). Culturally sensitive health care has also been described as care in which health care providers offer services in a manner that is relevant to patients’ needs and expectations (Majumdar, Browne, Roberts, & Carpio, 2004). Studies have found that patients’ satisfaction with their health care providers is positively associated with various physician behaviors such as taking time to provide patients with health care information and showing personal interest in patients (Ware, Davies-Avery, & Stewart, 1978), engaging in behaviors that show sensitivity and caring (Hallstrom & Elander, 200; Pascoe, 1983), and showing empathy, warmth, genuineness, support, and respect in interactions with patients (Beach, Saha, & Cooper, 2006; DiMatteo, Hays, & Prince, 1986).
How does cultural sensitivity affect health outcomes?
For example, research has shown that effective patient-provider communication, which is often influenced by the patient's and/or the provider's culture related language, is linked to patient satisfaction , medication adherence, and health outcomes (Betancourt et al., 2005; Stewart et al., 1999; Williams & Rucker, 2000). Additionally, in a study investigating language concordance between physicians and their patients as a factor in medication compliance among patients with asthma, it was found that patients in language discordant patient-provider dyads were more likely than patients in language concordant patient-provider dyads to (a) be medication nonadherent, (b) miss appointments, and (c) make emergency room visits (Manson, 1988).
What is the patient satisfaction questionnaire?
The Patient Satisfaction Questionnaire Short-Form(PSQ-18) is an 18-item short-form version of the 50-item Patient Satisfaction Questionnaire III (PSQ-III). The PSQ-18 measures patient satisfaction over seven dimensions: General Satisfaction, Technical Quality, Interpersonal Manner, Communication, Financial Aspect, Time Spent with Doctor, and Accessibility and Convenience. The PSQ-18 has been reported to have excellent internal consistency that exceeded .90 among samples that included various racial groups (Marshall & Hays, 1994). All items on the scale are rated on a 5-point Likert-type scale where 1 = “Strongly Agree” to 5 = “Strongly Disagree.” There is no total score. However, the 10 items in the technical quality, interpersonal manner, communication, and time with doctor subscales can be averaged to produce a measure of satisfaction with physician care (Marshall & Hays, 1994). The Satisfaction with Physician Care score of the PSQ-18 was used in the present study. Higher scores indicate greater patient satisfaction with provider care received. A sample item from the PSQ-18 is: “I'm very satisfied with the medical care I receive.”
How to recruit patients for a study?
The following two methods were used to recruit patients for the larger study: (a) a health care clinic office staff mailing method, and (b) an advertisement recruitment method. In the first of these methods, patients who met the participant inclusion criteria were identified by the health care clinic representative at each of the two community-based primary health care clinics participating in this study. These professionals mailed an invitation packet to each of the patients at their clinic who met the participation criteria. The invitation packet consisted of the following: (a) a cover letter that detailed the research purpose, participation instructions, and precautions taken to ensure patients’ confidentiality, (b) two copies of an Informed Consent Form (ICF), (c) a Demographic Data Questionnaire (DDQ), (d) a payment release form, and (e) a stamped pre-addressed envelope for returning the signed ICF and the completed DDQ to the researchers.
What is patient centered care?
Patient-centered culturally sensitive health care has the following specific characteristics: (a) it emphasizes displaying patient-desired, modifiable provider and staff behaviors and attitudes, implementing health care center policies, and displaying physical health care center environment characteristics and policies that culturally diverse patients identify as indicators of respect for their culture and that enable these patients to feel comfortable with, trusting of, and respected by their health care providers and office staff; (b) it conceptualizes the patient-provider relationship as a partnership that emerges from patient centeredness; and (c) it is patient empowerment oriented (Tucker, Mirsu-Paun, van den Berg et al., 2007). This care is unique in that it is based on views of culturally diverse patients rather than the views of health care professionals (e.g., psychologists, physicians, and health care site administrators) as to the health care provider and staff behaviors and attitudes and the health care characteristics and policies that convey cultural sensitivity. Empowering patients to share their views concerning culturally sensitive health care is a manifestation of patient-centeredness. Health care providers and staff can be responsive to such views of patients through engaging in behaviors and attitudes and fostering clinic characteristics and policies identified as important by culturally diverse patients. This patient-provider partnership approach to health care can enable culturally diverse patients to experience patient-centered culturally sensitive health care. Some health researchers have called for such care in response to findings indicating that patient-centered culturally sensitive health is associated with positive health behaviors and outcomes for both minority and majority patients (Davis et al., 2005; Safran, 2004). Other health researchers have asserted that provider cultural sensitivity and cultural competence are negatively associated with race/ethnicity-related health disparities (Betancourt, Green, Carrillo, & Park, 2005).
Is culturally sensitive health promotion effective?
There is some indication that perceived cultural sensitivity of health promoting interventions is associated with the effectiveness of these interventions. For example, culturally sensitive health promotion programs have been found to be effective when implemented with adults who have low levels of literacy (Winkleby, Howard-Pitney, & Albright, 1997) and working-class, multiethnic workers (Sorensen et al., 2005). Culturally sensitive health promotion programs have also been effective in helping women living in a low-income community quit smoking (O'Loughlin, Renaud, & Paradis, 1996).
Why is culturally responsive evaluation important?
To provide culturally responsive evaluation and treatment planning, counselors and programs must understand and incorporate relevant cultural factors into the process while avoiding a stereotypical or “one-size-fits-all” approach to treatment. Cultural responsiveness in planning and evaluation entails being open minded, asking the right questions, selecting appropriate screening and assessment instruments, and choosing effective treatment providers and modalities for each client. Moreover, it involves identifying culturally relevant concerns and issues that should be addressed to improve the client's recovery process.
What is the chapter of cultural competence?
Using Sue's (2001) multidimensional model for developing cultural competence, this chapter focuses on clinical and programmatic decisions and skills that are important in evaluation and treatment planning processes. The chapter is organized around nine steps to be incorporated by clinicians, supported in clinical supervision, and endorsed by administrators.
What is a culturagram?
The culturagram is an assessment tool that helps clinicians understand culturally diverse clients and their families ( Congress 1994, 2004; Congress and Kung 2005 ). It examines 10 areas of inquiry, which should include not only questions specific to clients' life experiences, but also questions specific to their family histories. This diagram can guide an interview, counseling, or clinical supervision session to elicit culturally relevant multigenerational information unique to the client and the client's family. Give a copy of the diagram to the client or family for use as an interactive tool in the session. Throughout the interview, the client, family members, and/or the counselor can write brief responses in each box to highlight the unique attributes of the client's history in the family context. This diagram has been adapted for clients with co-occurring mental and substance use disorders; sample questions follow.
What is treatment planning?
Treatment planning is a dynamic process that evolves along with an understanding of the clients' histories and treatment needs. Foremost, counselors should be mindful of each client's linguistic requirements and the availability of interpreters (for more detail on interpreters, see Chapter 4 ). Counselors should be flexible in designing treatment plans to meet client needs and, when appropriate, should draw upon the institutions and resources of clients' cultural communities. Culturally responsive treatment planning is achieved through active listening and should consider client values, beliefs, and expectations. Client health beliefs and treatment preferences (e.g., purification ceremonies for Native American clients) should be incorporated in addressing specific presenting problems. Some people seek help for psychological concerns and substance abuse from alternative sources (e.g., clergy, elders, social supports). Others prefer treatment programs that use principles and approaches specific to their cultures. Counselors can suggest appropriate traditional treatment resources to supplement clinical treatment activities.
What are some ways to build a therapeutic relationship?
It is up to counselors and other staff members to bridge the gap. Handshakes, facial expressions, greetings, and small talk are simple gestures that establish a first impression and begin building the therapeutic relationship. Involving one's whole being in a greeting—thought, body, attitude, and spirit—is most engaging.
Why do some clients resist the evaluation process?
Some clients may view the initial interview and evaluation as intrusive if too much information is requested or if the content is a source of family dishonor or shame. Other clients may resist or distrust the process based on a long history of racism and oppression. Still others feel inhibited from actively participating because they view the counselor as the authority or sole expert.
Do clients see their presenting problems as problems?
Some clients do not see their presenting physical, psychological, and/or behavioral difficulties as problems. Instead, they may view their presenting difficulties as the result of stress or another issue, thus defining or labeling the presenting problem as something other than a physical or mental disorder. In such cases, word questions about the following topics using the client's terminology, rather than using the word “problem.” Asking questions about the following topics can help you explore how a client may view his or her behavioral health concerns:
Why is culturally competent healthcare important?
Culturally competent healthcare organizations and practitioners are better able to connect with patients to alleviate mistrust and create shared understanding (using professional mental health interpreters when appropriate). That shared understanding is the first step toward successful diagnosis and treatment of mental illness.
What is culturally competent mental health management?
Culturally competent mental health management begins with policies and procedures that address the needs of diverse populations, including hiring diverse staff and creating space for training and development. With a strong commitment to culturally sensitive healthcare, mental health providers can deliver better diagnoses and outcomes for patients with mental illness.
How does culture affect mental health?
How culture affects mental health. Culture impacts every mental health patient— and every mental health practitioner. Culture is a key factor that we all bring to every interaction, and it can be especially influential in times of emotional distress. Culture, including beliefs, values, norms, and behaviors, affects how we experience ...
What are cultural meanings of mental illness?
In a clinical setting, cultural meanings of mental illness can account for whether and how a patient: Seeks or avoids treatment. Perceives and expresses symptoms. Copes with stress. Adheres to treatment plans. Attaches stigma to mental illness.
What are some terms that are acceptable to a psychiatric patient?
Don’t push individuals to accept a psychiatric diagnosis—build trust over time and use terms that are acceptable to them, including: "stress," "nerves," "sadness," "worries," etc.
What to do if a language concordant provider is not possible?
If a language concordant provider is not possible, be sure a professional interpreter is used when there is a language barrier. Don’t rely on family members to interpret.
Why Does Social Distance Exist?
A lack of cultural sensitivity has resulted in “embodied inequality.” External link: open_in_new Epidemiologist Nancy Krieger explains that people who feel marginalized or at risk of discrimination may experience poorer health outcomes throughout their lifespans, through no fault of their own.
What Is Cultural Sensitivity and How Can It Help?
Cultural sensitivity External link: open_in_new requires a set of skills for affirming diversity and embracing the values of people from different social or cultural backgrounds.
How Can Providers Develop Strategies for Cultural Sensitivity?
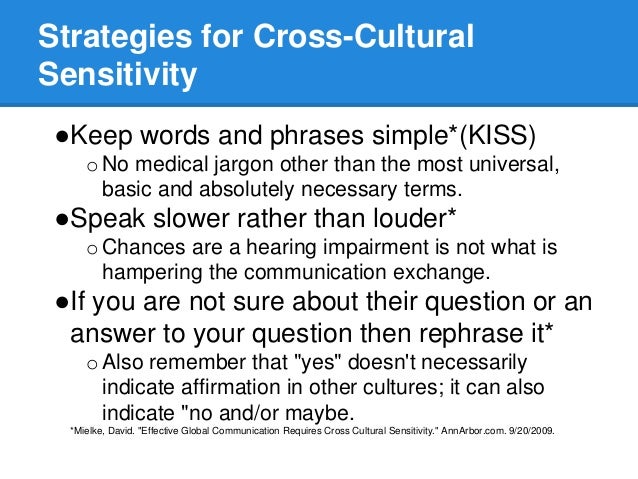
When the culture of an organization is built on principles of diversity, inclusion and affirmation, it’s easier to attract employees and clients who value these traits. Service providers and caregivers can actively engage in behaviors that show clients they are valued, heard and understood.
Where To Learn More About Cultural Sensitivity
The Cleveland Clinic Diversity Toolkit [PDF] (3.7 MB) External link: open_in_new is an in-depth guide to hundreds of cultural, religious and ethnic identities. This resource includes a guide to patient care and cultural communication and a glossary of helpful terms.
How to move towards cultural competence?
To move towards cultural competence, health care providers and other program staff should understand the ethnic and cultural needs of the populations they serve. Providing effective care involves taking the time and effort to learn from patients what is important to them in the experience of illness and treatment. According to medical anthropologist Arthur Kleinman, finding out “what is at stake” for the individual will provide crucial information to use in communication and in tailoring a treatment plan (Kleinman & Benson, 2006). Culture does matter in the clinic, and providers must remember that they too bring a cultural perspective to the patient-provider relationship. Increasing staff knowledge of the cultural and ethnic backgrounds of populations served is one important aspect of the CLAS standards.
What is cultural competence?
Cultural competence is an essential element of quality health care and can help improve health outcomes, increase clinic efficiency, and produce greater patient satisfaction (Brach & Fraser, 2000). Although there is no universally accepted definition of cultural competence, it may generally be understood to be a set of attitudes, skills, behaviors, and policies that enable organizations and staff to work effectively in cross-cultural situations. Furthermore, it reflects the ability to acquire and use knowledge of the health-related beliefs, attitudes, practices, and communication patterns of patients and their families in order to improve services, strengthen programs, increase community participation, and close the gaps in health status among diverse population groups (U.S. Office of Minority Health, 2006). Linguistically appropriate services are a key component of culturally competent health systems. In 2001, the U.S. Office of Minority Health issued Culturally and Linguistically Appropriate Service (CLAS) standards to help health care organizations move toward cultural competence (see Appendix C). Several of these standards are federal mandates supported by Title VI of the Civil Rights Act (1964), which prohibits discrimination on the basis of national origin and language. In summary, these standards aim to ensure that all federally funded health facilities provide services in a language understood by patients.
Why is it important to recognize your own beliefs and biases?
Further, providers must recognize their own beliefs and biases, as these may inadvertently be communicated to patients and families. Awareness of one’s own verbal and nonverbal communication styles will help avoid social gaffes that may offend others and adversely affect the relationship. Good patient-provider relationships are built on trust and respect; therefore, providers wishing to care effectively for their patients should heighten their sensitivities to both differences and similarities and use knowledge to guide their practice (Lipson & Dibble, 2005).
What are some culturally sensitive healthcare tips?
11 Tips for Providing Culturally Sensitive Healthcare. “You must not lose faith in humanity. Humanity is an ocean; if a few drops of the ocean are dirty, the ocean does not become dirty.” —Mahatma Gandhi. At this particular moment in time, a broad range of cultural conflicts are playing out on a daily basis.
Why is it important to create an environment that provides a safe platform for our patients and our fellow professionals?
It is crucial that as healthcare professionals we continue to set an example for our colleagues around the world by displaying our commitment to professional respect, diversity, acceptance, non-confrontational communication, and human values.
How to foster a respectful environment?
Respectful words and patient-first language help foster a respectful environment. While some patients may appreciate jokes, others may find them offensive or confusing. Build rapport with your patients and get to know their own personal communication style.
What is the goal of communication, rehabilitation, medical, and public health services?
Communication, rehabilitation, medical, and public health services share the same goal—improving the quality of life. But how can someone’s quality of life be improved if they do not feel heard or respected, or if they feel that their human rights have been violated?
How to reduce communication breakdown?
Listen to patient feedback . A clear understanding of the information from both sides is crucial in reducing communication breakdown. Your patients’ feedback about what they understand is vital. Ask them to repeat your instructions, invite them to tell you about their concerns, and listen carefully to their feedback.
