What is the most effective treatment?
Life Sustaining Treatment Ethical Issues in Pediatric Anesthesiology. Physician orders for life-sustaining treatment (POLST) were designed in part... Withholding and Withdrawing Life-Sustaining Therapies. Rohtesh S. Mehta, ... ... Life-sustaining …
What do you need to sustain life?
Life-sustaining treatment refers to medical treatments that are used to prolong life by supporting an essential body function, such as the hear t beating, breathing or …
What is necessary to sustain life?
A life-sustaining treatment, also referred to as a life-sustaining procedure or life-prolonging procedure, is a treatment utilized to prolong or sustain life without reversing the underlying medical condition. According to Oxford Medicine, some examples of procedures or treatments may include, but are not limited to the use of antibiotics, ...
What are some life sustaining processes?
Mar 11, 2014 · As straightforward as the foregoing analysis may seem, in real life it turns out to be very difficult to withhold or withdraw a life-sustaining treatment. Many health care providers believe that any omission of a life-sustaining treatment is tantamount to euthanasia or at least assistance in the patient’s suicide. And health professionals are not the only ones to reason in …
What are examples of life sustaining treatment?
Patients may consider many life-sustaining treatments; in addition to cardiopulmonary resuscitation (CPR), options include elective intubation, mechanical ventilation, surgery, dialysis, blood transfusions, artificial nutrition and hydration, diagnostic tests, antibiotics, other medications and treatments, as well as ...Oct 1, 2000
What criteria would you use to determine whether to terminate life sustaining treatment?
When is it justifiable to discontinue life-sustaining treatments? If the patient has the ability to make decisions, fully understands the consequences of their decision, and states they no longer want a treatment, it is justifiable to withdraw the treatment.
Which of the following is an example of a life sustaining measure?
Examples of life sustaining measures include artificial nutrition and hydration, cardiopulmonary resuscitation (CPR) and mechanical ventilation. Depending on the circumstances, dialysis treatments may also be considered life sustaining.
What are life sustaining needs?
Definition of life-sustaining : helping someone or something to stay alive : supporting or extending life life-sustaining medical treatment The storm brought life-sustaining rain/water to the farms.
Can doctors turn off life support without family consent California?
The California Heath Care Decisions law recognizes the right of an adult person to instruct a physician to withhold or withdraw life sustaining treatment because adults have a fundamental right to control decisions relating to the rendering of their own medical care, including the decision to have life-sustaining ...Aug 19, 2021
What is the difference between withholding and withdrawing life sustaining treatment?
Such decisions can essentially take one of two forms: withdrawing – the removal of a therapy that has been started in an attempt to sustain life but is not, or is no longer, effective – and withholding – the decision not to make further therapeutic interventions.Mar 4, 2005
What means life sustaining?
life–sustaining. /ˈlaɪfsəˌsteɪnɪŋ/ adjective. Britannica Dictionary definition of LIFE–SUSTAINING. : helping someone or something to stay alive : supporting or extending life.
Is oxygen considered a life saving measure?
The trial showed that oxygen provided no benefit over room air administered by nasal cannula in non-hypoxic patients. The concern with this trial is that people have taken the findings to mean that oxygen provides no benefit to patients when compared with administration of nothing, which is incorrect.
Which legally allows parents to withhold life sustaining treatment from a terminally ill child?
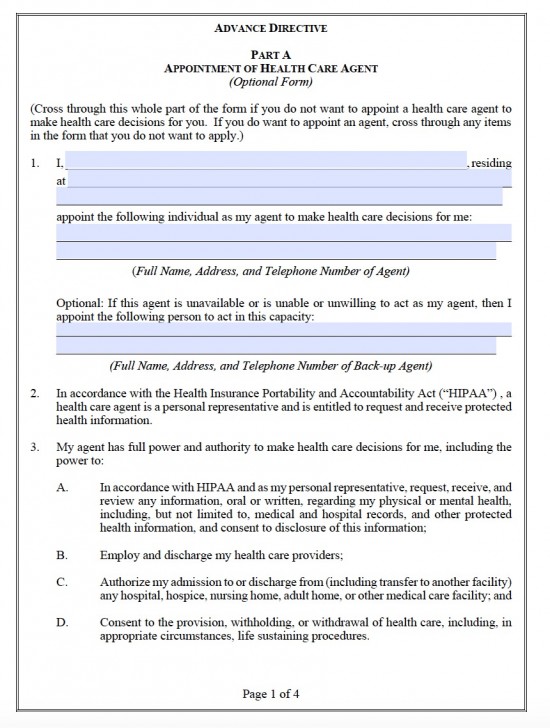
ADVANCE DIRECTIVES An advance directive is a general term that refers to one of two legal documents used to speak for the patient in the event that they cannot make decisions for themselves. Those two legal documents are 1) a living will or 2) the durable power of attorney.Apr 2, 2004
What is life saving treatment?
A life-sustaining treatment, also referred to as a life-sustaining procedure or life-prolonging procedure, is a treatment utilized to prolong or sustain life without reversing the underlying medical condition.
Do patients have the right to refuse life sustaining treatment?
Under federal law, the Patient Self-Determination Act (PSDA) guarantees the right to refuse life sustaining treatment at the end of life.Apr 16, 2015
Is life sustaining therapy needed when it's futile?
The law has long recognised that providing continued life-sustaining treatment to very sick and critically ill patients may be futile. The courts have consistently rejected an absolutist approach to care and treatment that requires doctors and nurses to continue with futile treatment right up to the point of death.May 23, 2013
How to treat a heart attack?
What is Life-sustaining treatment? 1 Chest compressions (repeatedly pushing very firmly on the chest in an attempt to pump blood around the body) 2 Defibrillation (using electric shocks to correct irregularities in the heart’s rhythm) 3 Artificially inflating the lungs (by inserting a tube into the windpipe or by placing an oxygen mask over the mouth and nose, to push air into the lungs) 4 Intravenous medication (administering medications such as adrenaline into a vein to improve heart muscle contraction and blood pressure)
What does CPR stand for in medical terms?
CPR stands for cardiopulmonary resuscitation. It is an emergency attempt to restart a person’s heart and/or breathing if they have a cardiac arrest. CPR is used to keep the person alive while the cause of the cardiac arrest is found and treated if possible. CPR can include:
What is CPR in a heart?
CPR can include: Chest compressions (repeatedly pushing very firmly on the chest in an attempt to pump blood around the body) Defibrillation (using electric shocks to correct irregularities in the heart’s rhythm)
What is mechanical ventilation?
Receiving mechanical or artificial ventilation means being put on a ventilator machine that helps you to breathe if you cannot do so on your own. Ventilators are also known as respirators or life-support machines.
What to do if you can't swallow?
If you cannot swallow, you may be given a liquid that contains the nutrition or hydration that you need. This can be given through an intravenous drip (directly into a vein), a tube through the nose or a tube directly into the stomach (sometimes known as a PEG feed).
Can antibiotics be given through a vein?
Antibiotics can be given through an intravenous drip (directly into a vein) or by mouth as a tablet or liquid.
What to do when you are near the end of your life?
Making the Decision for Yourself. If you are near the end of your life or you have an illness that will not improve, you can choose what kind of treatment you want to receive. You should know that the illness or the injury is the main cause of the end of life, not the removal of life support equipment. Talk to your providers to learn about life ...
How to get a DNR?
To make sure your wishes are followed: 1 Talk to your providers about your choices. 2 Write your decisions in an advance health care directive. 3 Find out about a do-not-resuscitate (DNR) order. 4 Ask someone to be your health care agent or proxy. Be sure this person knows your wishes and if you make any changes in your health care choices.
What is expand section?
Expand Section. Treatments to extend life can include the use of machines. This equipment does the work of the body organ, such as: A machine to help with breathing ( ventilator) A machine to help your kidneys ( dialysis) A tube into your stomach to provide food ( nasogastric or gastrostomy tube)
What is the law for EMTs?
By law, EMTs and other emergency medical professionals are required to carry out certain life-sustaining treatments, such as cardiopulmonary resuscitation (CPR) if someone’s heart or breathing stops. If you don't want to receive these treatments, you need to have either a POLST or a DNR stating so. (Both a POLST and a DNR are medical orders that EMTs and other emergency medical professionals must honor.)
What is CPR in medical terms?
Cardiopulmonary resuscitation (CPR): If you have no pulse and are not breathing, you can choose to have emergency medical professionals attempt resuscitation or not attempt resuscitation. Medical interventions: If you have a pulse and/or are breathing, you can choose to receive:
Where to store a POLST?
If you’re in a home setting, the POLST form should be stored somewhere that emergency medical personnel will easily see it, such as on your refrigerator, by your bed, or by your front door. If they do not see the POLST form or cannot find the form, they will go about their normal procedures. If you’re in a medical setting, the doctor managing your care must have the original copy of the POLST attached to your medical file or chart.
What is a TPOPP?
TPOPP (Transportable Physician Orders for Patient Preferences) The forms differ in name and structure depending on where you live, but are conceptually the same across all states. Helpful Tip: POLST forms are often printed on brightly colored paper so that they’re easy to see and find.
What is the meaning of "quality of life"?
To maintain life for a period, while the decision maker/family struggles with end-of-life decisions. When there is no clear decision maker, and the family cannot reach a consensus. When the quality of life is good, as defined by the patient. Potential reasons to withhold or withdraw artificial hydration or nutrition.
How many people survive CPR?
Performing CPR on hospitalized patients is usually ineffective, with only 6 to 17 percent of patients surviving to discharge; many survivors die during the next few months or have a poor quality of life. Patients with malignancy, sepsis, pneumonia or renal failure have even lower survival rates.
Who is Richard Ackerman?
ACKERMANN, M.D., is professor of family medicine at the Mercer University School of Medicine, Macon, Ga. He is director of the family practice residency program at the Medical Center of Central Georgia, Macon. Dr. Ackermann earned his medical degree from Duke University School of Medicine, Durham, N.C., and completed a residency in family practice at Naval Hospital, Charleston, S.C.
How to improve end of life care?
Most states now have initiatives to improve end-of-life care by using forms that put a person’s goals and preferences into medical orders that a clinician must follow. These forms are different from advance directives and are most appropriate for individuals who are seriously ill.
What are the symptoms of end of life?
End of Life Symptoms 1 Loss of appetite (anorexia) is an almost universal symptom in individuals who are dying. Appetite stimulants and tube-feeding do not prolong survival and should not be used. Ice chips, ice pops, moist swabs, or artificial saliva can help prevent the mouth from becoming dry and cracked. 2 Breathlessness (also known as dyspnea) at the end of life is common and often distressing. Individuals can feel breathless even if their breathing and oxygen levels are normal. Moving cool air across the face from a window or with a fan can be helpful. Oxygen therapy and, in some cases, medications can also help. 3 Terminal respiratory secretions (known as a“death rattle”) are a sign that death is close. These sounds are caused by fluid that collects in the back of the throat and windpipe in individuals who no longer have a swallowing or cough reflex. Repositioning and elevating the head of the bed can be helpful. Gentle suctioning and medications to dry up secretions may also be used.
What is palliative care?
Palliative care is specialized medical care that focuses on relieving pain and other symptoms of illness. Palliative care is appropriate for any person with a serious illness, regardless of the stage of the disease or how long the person is expected to live.
What is hospice care?
Hospice care is specialized care for people who are believed to have a life expectancy of 6 months or less. Accepting hospice care means shifting from the use of medical treatments to prolong life as much as possible toward a focus on treating symptoms and improving quality of whatever life remains for a person. Hospice care can be provided at a person’s home, or at a nursing home or inpatient hospice facility. The care is provided by a team that includes a physician or nurse practitioner, nurse, home health aide, social worker, chaplain, and volunteer. Although these team members provide regular visits and 24/7 phone availability, the majority of care for people receiving hospice care is provided by family, friends, or care teams at a facility.
Why is it important to have advance directives?
Because many illnesses and complications cannot be anticipated, it is extremely important to have advance directives. Timely completion of these documents can help prevent unwanted burdensome treatments at the end of life. It is also important to discuss your advance directives with your family or friends.
What are the symptoms of a dying person?
These include loss of appetite, breathlessness, and/or loud respiration/breathing. There are several non-medical strategies to ease someone’s discomfort at the end of life.
Can you drink and eat when you are sick?
Decreased eating and drinking is common among people who are seriously ill and near the end of life. This can be extremely distressing for families or caregivers, who may want to provide food and water artificially, such as through intravenous lines or a feeding tube. Although food and drink should always be offered by mouth to a person who is seriously ill or dying, artificial feeding and hydration may cause discomfort to someone whose body is no longer processing food and liquids normally.
