What is the first line conservative treatment for hemorrhoids?
First-line conservative treatment of hemorrhoids consists of a high-fiber diet (25 to 35 g per day), fiber supplementation, increased water intake, warm water (sitz) baths, and stool softeners. 7, 11 – 13 Giving patients a chart with the fiber content of common foods may help them increase their fiber intake.
Can hemorrhoids be treated individually?
Hemorrhoids are a common reason for office visits. Each patient is unique, and with a range of treatments available, treatment can be individualized. This article reviews the diagnosis and decision-making process for individualized treatment. Hemorrhoids account for more than 3.5 million office visits annually.
What are the treatment options for haemorrhoidal disease?
Over the counter topical preparations that contain a combination of local anaesthetics, corticosteroids, astringents, and antiseptics are available, and these can alleviate symptoms of pruritus and discomfort in haemorrhoidal disease.
What are the minimally invasive treatments for internal hemorrhoids?
Minimally invasive procedures 1 Rubber band ligation. Your doctor places one or two tiny rubber bands around the base of an internal hemorrhoid to cut off its circulation. ... 2 Injection (sclerotherapy). Your doctor injects a chemical solution into the hemorrhoid tissue to shrink it. ... 3 Coagulation (infrared, laser or bipolar). ...

Which treatment is best for hemorrhoids?
Apply an over-the-counter hemorrhoid cream or suppository containing hydrocortisone, or use pads containing witch hazel or a numbing agent. Soak regularly in a warm bath or sitz bath. Soak your anal area in plain warm water for 10 to 15 minutes two to three times a day.
What is the safest hemorrhoid surgery?
In patients with high-grade, symptomatic hemorrhoids, surgical hemorrhoidectomy is the most effective modality with the lowest recurrence rates, although it causes more pain than conservative methods.
Can hemorrhoids cured without surgery?
Hemorrhoids often get better without surgery or even procedures your doctor can do in the office. Start with over-the-counter products and lifestyle changes. (If you're pregnant, you should talk to your doctor before you try any medicine or change your diet.)
How do you permanently remove a hemorrhoid?
Surgery to remove hemorrhoids is called hemorrhoidectomy. The doctor makes small cuts around the anus to slice them away. You may get local anesthesia (the area being operated on is numb, and you're awake though relaxed) or general anesthesia (you're put to sleep).
What size hemorrhoids need surgery?
If someone has grade 3 or grade 4 hemorrhoids, doctors often recommend surgery. A general or local anesthetic is usually needed for this. You then have to stay in the hospital for a few days, and stay off work for some time too.
Is there an alternative to hemorrhoid surgery?
The non-surgical treatments for hemorrhoids include rubber band ligation (RBL), injection sclerotherapy (IS), infrared coagulation (IRC), anal stretch, cryosurgery, laser hemorroidectomy.
What foods trigger hemorrhoids?
What should I avoid eating if I have hemorrhoids?cheese.chips.fast food.ice cream.meat.prepared foods, such as some frozen and snack foods.processed foods, such as hot dogs and some microwavable dinners.
What is a Stage 3 hemorrhoid?
Grade 3 - Hemorrhoid protrudes through the anus during straining or evacuation but needs to be manually returned to position. Grade 4 - Hemorrhoid remains prolapsed outside of the anus. Grade 3 hemorrhoids are internal hemorrhoids which prolapse, but do not go back inside the anus until the patient pushes them back in.
Why won't my hemorrhoid go away?
If you have hemorrhoids that won't go away, see your doctor. They can recommend a variety of treatments, ranging from diet and lifestyle changes to procedures. It's important you see your doctor if: You're experiencing discomfort in your anal area or have bleeding during bowel movements.
When do hemorrhoids need surgery?
Surgery for hemorrhoids is usually only performed for severe cases, such as when home remedies aren't working, emergencies (such as extreme bleeding), or when they become so bothersome or painful that they impact your lifestyle.
When does a hemorrhoid need to be removed?
Acutely swollen and tender thrombosed external hemorrhoids can be surgically removed during the first 72 hours after onset. After 72 hours, the discomfort of the procedure often exceeds the relief provided by the surgery.
Is hemorrhoid surgery very painful?
Hemorrhoidectomy surgery may be painful, but different procedures to remove less serious hemorrhoids may be painless. Hemorrhoids, commonly known as piles, are engorged veins located around the anus or in the lower rectum. Hemorrhoids occur as a result of excessive straining, usually during defecation.
How many patients require no surgery for hemorrhoids?
Studies have shown that more than 80 percent of patients will require no surgical intervention for hemorrhoidal disease (internal or external) if conservative measures are followed appropriately, which is why we begin there.
What is the name of the disease that causes bleeding and swelling of the internal hemorrhoids?
Pregnancy. Diarrhea. Chronic or repeated swelling of internal hemorrhoids is classified as hemorrhoidal disease, and symptoms include anal itching, painless bright red bleeding, prolapsing or bulging of the hemorrhoidal tissue, and pain due to thrombosis or a blood clot.
What is the difference between a grade 2 and grade 3 hemorrhoids?
Grade 2 hemorrhoids reduce spontaneously. Grade 3 internal hemorrhoids fill the anoscope and prolapse outside of the anal canal while straining or defecating. Manual reduction is required. This means the hemorrhoids fall below the dentate line and pain may be present.
Why do my internal hemorrhoids not have nerve endings?
Internal hemorrhoids do not contain nerve endings because they are above the dentate line, a line that divides the upper two thirds and lower third of the anal canal. But they can become swollen and cause uncomfortably and sometimes painful symptoms. Swelling can be caused by: Excessive straining. Hard, formed stools.
Why does my hemroid swell?
Swelling can be caused by: Chronic or repeated swelling of internal hemorrhoids is classified as hemorrhoidal disease, and symptoms include anal itching, painless bright red bleeding, prolapsing or bulging of the hemorrhoidal tissue, and pain due to thrombosis or a blood clot.
How many people have internal hemorrhoids?
Internal hemorrhoidal disease affects about 10 million people per year in the United States, or about 4.4 percent of the population, according to recent studies. It is typically diagnosed during an anoscope exam, which is performed in the doctor’s office, or via colonoscopy, which is performed in a procedure room under light sedation.
What foods are good for a patient with a bowel problem?
Foods rich in fiber include avocados, beans, fruits (apples, bananas, and pears), and vegetables (peas, broccoli). If the patient does not get enough fiber, it is important to consider dietary changes and add a supplement.
What is the best way to treat a recurring hemorrhoids?
The surgery can be done with local anesthesia combined with sedation, spinal anesthesia or general anesthesia. Hemorrhoidectomy is the most effective and complete way to treat severe or recurring hemorrhoids.
How to treat hemorrhoids?
You can use acetaminophen (Tylenol, others), aspirin or ibuprofen (Advil, Motrin IB, others) temporarily to help relieve your discomfort. With these treatments, hemorrhoid symptoms often go away within a week.
How to remove a hemorrhoid with a rubber band?
To remove a hemorrhoid using rubber band ligation, your doctor inserts a small tool called a ligator through a lighted tube (scope) in the anal canal and grasps the hemorrhoid with forceps. Sliding the ligator's cylinder upward releases rubber bands around the base of the hemorrhoid.
How to treat hemorrhoids in the anal area?
Use topical treatments. Apply an over-the-counter hemorrhoid cream or suppository containing hydrocortisone, or use pads containing witch hazel or a numbing agent. Soak regularly in a warm bath or sitz bath. Soak your anal area in plain warm water for 10 to 15 minutes two to three times a day.
How long does it take for a hemorrhoid band to fall off?
The hemorrhoid withers and falls off within a week. Hemorrhoid banding can be uncomfortable and cause bleeding, which might begin two to four days after the procedure but is rarely severe.
What is the procedure called when you have to remove a hemorrhoids?
This procedure, called stapled hemorrhoidopexy, blocks blood flow to hemorrhoidal tissue. It is typically used only for internal hemorrhoids. Stapling generally involves less pain than hemorrhoidectomy and allows for earlier return to regular activities.
What to do if you have a hemroid?
Medications. If your hemorrhoids produce only mild discomfort, your doctor might suggest over-the-counter creams, ointments, suppositories or pads. These products contain ingredients such as witch hazel, or hydrocortisone and lidocaine, which can temporarily relieve pain and itching.
How to prevent hemorrhoids?
You can help prevent hemorrhoids by. eating foods that are high in fiber. drinking water or other nonalcoholic liquids each day as recommended by your health care professional. not straining during bowel movements. not sitting on the toilet for long periods of time. avoiding regular heavy lifting.
How to treat hemorrhoids at home?
You can most often treat your hemorrhoids at home by. eating foods that are high in fiber. taking a stool softener or a fiber supplement such as psyllium. NIH external link. (Metamucil) or methylcellulose (Citrucel) drinking water or other nonalcoholic liquids each day as recommended by your health care professional.
What is the procedure to remove internal hemorrhoids?
Hemorrhoid stapling. A doctor, most often a surgeon, may use a special stapling tool to remove internal hemorrhoid tissue and pull a prolapsing internal hemorrhoid back into the anus. Your doctor will give you anesthesia for this treatment. Sometimes complications of hemorrhoids also require treatment.
How long does it take for a prolapsed hemorrhoid to go away?
Most often, doctors recommend using over-the-counter products for 1 week. You should follow up with your doctor if the products. do not relieve your symptoms after 1 week. cause side effects such dry skin around your anus or a rash. Most prolapsed internal hemorrhoids go away without at-home treatment.
What is the procedure used to treat bleeding or prolapsing internal hemorrhoids?
Office treatments include the following: Rubber band ligation. Rubber band ligation is a procedure that doctors use to treat bleeding or prolapsing internal hemorrhoids. A doctor places a special rubber band around the base of the hemorrhoid. The band cuts off the blood supply.
How does infrared light affect hemorrhoids?
The scar tissue cuts off the blood supply, often shrinking the hemorrhoid. Infrared photocoagulation. A doctor uses a tool that directs infrared light at an internal hemorrhoid. Heat created by the infrared light causes scar tissue to form , which cuts off the blood supply, often shrinking the hemorrhoid.
How to treat a swollen rectum?
sitting in a tub of warm water, called a sitz bath, several times a day to help relieve pain. Applying over-the-counter hemorrhoid creams or ointments or using suppositories—a medicine you insert into your rectum —may relieve mild pain, swelling, and itching of external hemorrhoids.
What should be considered when choosing a treatment for hemorrhoids?
In choosing the treatment for hemorrhoids, one should consider the disease grade and severity, its impact on the quality of life, the degree of pain it causes, the patient’s likelihood of adhering to treatment, and the patient’s personal preference.
Which is the most effective modality for symptomatic hemorrhoids?
In patients with high-grade, symptomatic hemorrhoids, surgical hemorrhoidectomy is the most effective modality with the lowest recurrence rates, although it causes more pain than conservative methods. © 2019 The Cleveland Clinic Foundation. All Rights Reserved.
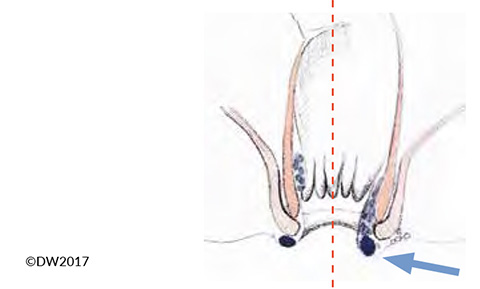
How is the prolapsing part of the internal hemorrhoidal cushion moved?
In this procedure, the prolapsing part of the internal hemorrhoidal cushion is moved upward by stapling the rectal mucosa just above the hemorrhoid ( Figure 4 ). This is not an option for patients with thrombosed internal hemorrhoids or with external hemorrhoids.
What are the factors that contribute to hemorrhoids?
Aspects of modern life that may promote hemorrhoids include increased consumption of processed foods, a sedentary lifestyle, and using cell phones while defecating, which translates to much more time spent on the toilet.
What is the grade of hemorrhoids?
Hemorrhoids are graded on a scale of I (least severe) through IV (most severe). Office-based treatments are effective for grades I, II, and some grade III hemorrhoids. Surgical excision is the standard for high-grade hemorrhoids.
What is conservative stool?
Conservative measures are aimed at softening the stool, relieving pain, and correcting bad toileting habits. In most cases, the primary precipitating factor is lifestyle, and unless patients change it, they are more likely to have recurrent symptoms in the long term.
What does it mean when you have red blood on your stool?
Typically, the presenting symptom is painless rectal bleeding associated with bowel movements , usually appearing as bright red blood on the toilet paper or coating the stool. Severe itching and anal discomfort are also common, especially with chronic hemorrhoids.
