
Congestive heart failure and AF share common mechanisms, including myocardial fibrosis and dysregulation of intracellular calcium and neuroendocrine function. Pharmacological treatments including beta-blockers, digoxin, angiotensin-converting enzyme inhibitors and angiotensin receptor blockers can be useful in treating both of these conditions.
Full Answer
What are the treatment options for congestive heart failure?
Treatment options for CHF include changes to diet and lifestyle, medications, implantable cardioverter-defibrillator, and in serious situations, a heart transplant. Summary of Afib Vs.
What are the treatment options for AFIB and CHF?
Treatment options for Afib include AV node ablation, medication, and synchronized cardioversion. Treatment options for CHF include changes to diet and lifestyle, medications, implantable cardioverter-defibrillator, and in serious situations, a heart transplant. Summary of Afib Vs.
Does atrial fibrillation lead to congestive heart failure?
Considering overall heart health, there are often other heart issues that go along with atrial fibrillation. A common condition those living with AFib often face is congestive heart failure, commonly known as CHF. CHF often refers to a weak heart but can also signify a stiff heart, meaning it doesn’t pump blood efficiently throughout the body.
What is the primary management of atrial fibrillation (AFIB) (AF)?
In patients with AF and HF, the primary management is optimizing HF management with guideline-directed medical therapy and device therapy such as implantable cardioverter-defibrillator with or without CRT based on guideline recommendations.
How is heart failure and atrial fibrillation treated?
Treatments for atrial fibrillation include medicines to control heart rate and reduce the risk of stroke, and procedures to restore normal heart rhythm. It may be possible for you to be treated by a GP, or you may be referred to a heart specialist (a cardiologist).
Is atrial fibrillation related to congestive heart failure?
Atrial fibrillation and congestive heart failure are morbid conditions that share common risk factors and frequently coexist. Each condition predisposes to the other, and the concomitant presence of the two identifies individuals at increased risk for mortality.
How long can you live with AFib and congestive heart failure?
Although there have been recent improvements in congestive heart failure treatment, researchers say the prognosis for people with the disease is still bleak, with about 50% having an average life expectancy of less than five years.
What treatment is used for congestive heart failure?
Medicines are the main treatment for heart failure, but for some people surgery may help. Operations that can help with heart failure include: heart valve surgery. a coronary angioplasty or bypass.
What is the most common treatment for atrial fibrillation?
Heart rate medicines: The most common way to treat atrial fibrillation is with drugs that control your heartbeat....Potassium channel blockers, which slow the electrical signals that cause AFib:Amiodarone (Cordarone, Nexterone Pacerone),Dofetilide (Tikosyn)Sotalol (Betapace, Sorine, Sotylize)
What is life expectancy with atrial fibrillation?
Of 71 patients with paroxysmal or persistent atrial fibrillation, 22 had progression to permanent atrial fibrillation. Overall survival of the 76 patients with lone atrial fibrillation was 92% and 68% at 15 and 30 years, respectively, similar to 86% and 57% survival for the age- and sex-matched Minnesota population.
Is congestive heart failure a death sentence?
Although it can be a severe disease, heart failure is not a death sentence, and treatment is now better than ever. When this happens, blood and fluid may back up into the lungs (congestive heart failure), and some parts of the body don't get enough oxygen-rich blood to work normally.
Can you recover from congestive heart failure?
Like so many diagnoses, the words pack an emotional wallop: Congestive heart failure. While the phrase may sound like a death sentence, the good news is that many people whose hearts are considered to be failing can make a virtually complete recovery.
Can the heart repair itself after congestive heart failure?
The heart is unable to regenerate heart muscle after a heart attack and lost cardiac muscle is replaced by scar tissue. Scar tissue does not contribute to cardiac contractile force and the remaining viable cardiac muscle is thus subject to a greater hemodynamic burden.
What is the first line treatment for congestive heart failure?
Loop diuretics should be used as first-line agents, with thiazides added for refractory fluid overload. Diuretic treatment should be combined with a low-salt diet,8 a β-blocker, and an ACE inhibitor. The practitioner should begin with oral furosemide, 20 to 40 mg once daily.
How do they remove fluid from congestive heart failure?
During pericardiocentesis, a doctor inserts a needle through the chest wall and into the tissue around the heart. Once the needle is inside the pericardium, the doctor inserts a long, thin tube called a catheter. The doctor uses the catheter to drain excess fluid. The catheter may come right out after the procedure.
What is the first drug of choice for congestive heart failure?
Digoxin has been the traditional first drug of choice for CHF, but with protracted controversy about its efficacy and safety. It is hope that new agents as vesnarione, and ibopamine may improve contractility without having adverse consequences.
What are the best medications for sinusitis?
Pharmacological treatments including beta-blockers, digoxin, angiotensin-converting enzyme inhibitors and angiotensin receptor blockers can be useful in treating both of these conditions. Antiarrhythmic medications intended to achieve and maintain sinus rhythm may be beneficial in some patients with AF and CHF.
Is AF a congestive heart failure?
Atrial fibrillation (AF) and congestive heart failure (CHF) are commonly encountered together, and either condition predisposes to the other. Risk factors for AF and CHF include age, hypertension, valve disease, and myocardial infarction, as well as a variety of medical conditions and genetic variants. Congestive heart failure and AF share common ...
How does atrial fibrillation affect the heart?
In an analysis of Framingham Heart Study, atrial fibrillation (AF) and congestive heart failure (CHF) have been found to be associated with each other, and the presence of either one increases the risk of developing the other and also increases the mortality risk associated with the other. 1 Both the incidence and the prevalence of AF are increasing, even after adjustment for aging of the population, 2, 3 and the prevalence of CHF is increasing primarily as a result of improved survival after its onset due to improved treatment. 4 Both AF and CHF are modern epidemics in cardiovascular disease. 5 In the ATRIA (Anticoagulation and Risk Factors In Atrial Fibrillation) study, 2.3 million adults in the United State were estimated in 1996 to suffer from AF and the number is expected to increase to 5.6 million in 2050. 6 The lifetime risk of developing AF after age 40 is 26% for men and 23% for women, 7 and its presence increases the risk of stroke, 8 dementia, 9 and death. 8 CHF afflicts 5.3 million adult Americans, 10 with a lifetime risk after age 40 of more than 20%. 11 The burden of health-care expenditure related to these two conditions is profound, with CHF alone accounting for almost $35 billion. 10
Does statin help with AF?
Statins have also been reported in some studies to reduce the incidence of AF, 81 although the mechanism for this effect is not clear and may relate to antioxidant and anti-inflammatory properties, which might exert a stabilizing effect on the cardiac membrane and prevent atrial remodeling.
It can be the primary cause of congestive heart failure
Sometimes people are first diagnosed with atrial fibrillation, they don’t necessarily feel their heart beating fast or irregular, they only notice an increasing shortness of breath. So, when they are finally diagnosed, their heart may have had this rapid heart beat for a few weeks or even months at a time.
It can be secondary to congestive heart failure
Having a weak or stiff heart can cause elevated pressure in your heart, not only on the top chambers of the heart but on the bottom chambers as well. Over time, this ends up dilating the upper chambers and leads to signs of atrial fibrillation. In this scenario the AFib is secondary to the CHF.
What happens when your heart rate increases?
The increase in resting heart rate shortens diastolic filling time that may result in a reduction in cardiac output. The irregular ventricular response results in a 25% reduction in cardiac output 5, 6 because filling during long cycles does not sufficiently compensate for the reduced filling in short cycles.
What is AV node ablation?
AV node ablation was the original interventional procedure for patients with medically refractory AF with or without HF; for many years, AV node ablation with RV apical pacing was used in this population with good reported outcomes.
Is AF a coexisting condition?
It is also apparent that, in many patients, AF causes symptomatic deterioration and may be associated with increased mortality. The difficulty is in identifying those patients in whom AF is simply a coexisting condition and those in whom AF is a major contributor to quality of life, ventricular function, and long-term mortality. Although clinical trials are no doubt the gold standard for evaluating treatments and strategies for treatment of AF in HFrEF patients, they can never fully address the need for an individualized approach. For patients who deteriorate early after the onset of AF despite adequate rate control, it is logical that an aggressive approach to rhythm control would be warranted. For those in whom the relationship between AF and symptoms of HF is less clear, a trial of sinus rhythm by performing cardioversion with or without concomitant antiarrhythmic therapy may help to assess whether the patient feels better and whether structural parameters like EF improve. For all patients, oral anticoagulation, lifestyle modifications, and optimization of guideline-directed medical therapy are a must. Rate control should also be broadly applied, even if rhythm control is the final goal. Although RACE II has suggested that lenient rate control may be as good as stricter rate control, 124 there were very few patients in that study with HFrEF and trials like AF-CHF used much stricter definitions of rate control. Therefore, guidelines continue to suggest that stricter rate control in HF patients, particularly those with reduced EF, is preferred. 40, 41 Finally, interventional approaches should be considered in HFrEF patients. Catheter ablation is an emerging and potentially promising therapy for HF patients in whom lasting rhythm control is desired. Ablation may reduce the morbidity associated with long-term treatment with antiarrhythmic agents such as amiodarone. AV nodal ablation with resynchronization therapy should also not be overlooked, particularly for patients who may not be good candidates for catheter ablation (large left atrium, older age, multiple comorbidities) and in whom strict rate control may not be achieved through pharmacological treatment alone. With the imminent release of several clinical trial results in the near future, we can look forward to a further refinement in how we approach the treatment of patients with HF and concomitant AF.
How does heart failure lead to AFIB?
How Heart Failure Leads to AFib. It works in the other direction, too. Your heart's rhythm is controlled by electrical signals. For those signals to work well, they need healthy heart tissue. But heart failure can actually stretch your atria and cause tissue in your heart to thicken and scar.
What does AFIB do to your heart?
You need your heart to do one job and do it really well: pump blood throughout your body. For that, it needs a regular rhythm and strong, healthy muscle. But if you have AFib, your heart's upper chambers -- the atria -- are out of sync. They don't have that nice steady rhythm.
Why do my chances of heart failure go up?
Your odds for heart failure and AFib go up if you have other heart conditions, such as: Coronary artery disease, where plaque builds up in your heart's arteries and leads to less blood flow. Cardiomyopathy, which is damage to your heart muscle. Heart valve problems, such as a leaky valve or a valve that doesn't fully open.
What are the risks of heart disease?
Other health conditions. Other health issues can also raise your risk, such as: 1 Diabetes, since it increases your odds for coronary artery disease and high blood pressure 2 High blood pressure, which over time can weaken, stiffen, and thicken your heart tissue 3 Obesity, as it often leads to higher blood pressure and raises your chances of having diabetes 4 Overactive thyroid, because too much thyroid hormone can make your heart beat faster than normal 5 Sleep apnea, which can lead to lower oxygen levels while you sleep and affect your heart's rhythm
What are the chances of getting AFIB?
Age. The older you are, the greater the chances you'll get AFib or heart failure. Most people who have both conditions are older adults. Genes. There's still a lot of research to be done here, but certain differences in your genes may affect how likely it is that you end up with heart failure or AFib. Gender.
What causes a person's heart to swell?
Myocarditis, where the muscles of your heart get swollen and irritated. Other health conditions. Other health issues can also raise your risk, such as: Diabetes, since it increases your odds for coronary artery disease and high blood pressure.
Why does high blood pressure cause heart disease?
High blood pressure, which over time can weaken, stiffen, and thicken your heart tissue. Obesity, as it often leads to higher blood pressure and raises your chances of having diabetes. Overactive thyroid, because too much thyroid hormone can make your heart beat faster than normal.
What are the treatment options for AFIB?
Treatment. Treatment options for Afib include AV node ablation, medication, and synchronized cardioversion. Treatment options for CHF include changes to diet and lifestyle, medications, implantable cardio verter-defibrillator, and in serious situations, a heart transplant.
What causes congestive heart failure?
Congestive Heart Failure can be caused by diabetes and other disorders that lead to damage to the heart muscle. Hypertension, coronary artery disease and having a heart attack can all lead to Congestive Heart Failure. Various cardiomyopathies, congenital heart defects, and valve disease can also be a cause of CHF.
What is CHF in a heart?
CHF is Congestive Heart Failure where the hearts’ inability to pump properly causes fluid to accumulate in the body. Both Afib and CHF can sometimes be treated with medication and can both be caused by hypertension and coronary artery disease. Author. Recent Posts.
How do you know if you have atrial fibrillation?
Symptoms of atrial fibrillation include having difficulty in breathing, heart palpitations, a feeling of weakness and difficulty exercising. People with afib also often feel faint and lightheaded. They may also experience some chest discomfort.
What is CHF in medical terms?
CHF is Congestive Heart Failure and describes the condition in which the heart does not pump adequately leading to fluids building up in the body because the failing heart has a bad effect on the kidneys. This accumulation of fluid in organs then causes congestion.
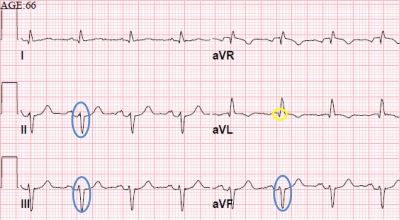
What is the diagnosis of AFIB?
Diagnosis: Echocardiography is how Afib is diagnosed and typically the P waves (which indicate atria contracting normally) are absent from the tracing. There is also often the presence of so-called fibrillatory or f waves that will be seen before the QRS complex and after each complex.
What are the risk factors for AFIB?
The risk factors for developing Afib include being over age 60, having hypertension (high blood pressure), coronary artery disease or cardiomyopathy. Diabetics are also at increased risk for Afib.

Introduction
- In an analysis of Framingham Heart Study, atrial fibrillation (AF) and congestive heart failure (CHF) have been found to be associated with each other, and the presence of either one increases the risk of developing the other and also increases the mortality risk associated with the other.1 Both the incidence and the prevalence of AF are increasing...
Temporal Relation of Af and CHF
- In a large cohort of patients from the Framingham Heart Study, at first diagnosis of AF, 26% of patients had a prior or concurrent diagnosis of CHF, and 16% of the remaining patients developed the condition during the follow up period of 5.6 years (Figure 1a). Among patients who developed CHF, 24% had a prior or concurrent diagnosis of AF, and 17% developed AF during the follow up …
Common Risk Factors For Af and CHF
- Genetics Epidemiological data point towards a heritable contribution to the development of AF. In the Framingham Heart study, the odds ratio of developing AF over 4 years among participants with a history of parental AF was 1.85.16 In a study conducted in Iceland of more than 5,000 patients, the relative risk of developing AF was 1.77 in those with an affected first-degree relativ…
Af and CHF: Therapeutic Approaches
- Rate or rhythm control Based upon the expectation that CHF would be more easily managed in AF patients if they could be kept in sinus rhythm, it has been postulated that restoration and maintenance of sinus rhythm would be of specific importance in such patients. The presence of sinus rhythm as opposed to AF was associated with improved survival in the AFFIRM trial, but a…
Device-Based Therapy
- Ablation and pacing Ablation of the AV node and placement of a pacemaker to regulate heart rate is an option for patients with AF refractory to medical therapies.92 This may improve exercise duration and quality of life.93 But right ventricular pacing may cause or aggravate mitral regurgitation and lead to worsening of heart failure in patients with pre-existing LV dysfunction a…
Conclusion
- AF and CHF are highly prevalent diseases in modern society, with considerable morbidity and mortality. Each disorder predisposes to the other, and both share common molecular and physiologic mechanisms. A variety of treatments, both pharmacologic and non-pharmacologic, have demonstrated benefit in the treatment of AF and CHF, and future therapies are on the horiz…
References
- Wang TJ, Larson MG, Levy D, et al. Temporal relation of atrial fibrillation and congestive heart failure and their joint influence on mortality: the Framingham Heart Study. Circulation 2003; 107:29...
- Tsang TS, Petty GW, Barnes M, et al. The prevalence of atrial fibrillation of incident stroke cases and matched population controls in Rochester, Minnesota: changes over three decade…
- Wang TJ, Larson MG, Levy D, et al. Temporal relation of atrial fibrillation and congestive heart failure and their joint influence on mortality: the Framingham Heart Study. Circulation 2003; 107:29...
- Tsang TS, Petty GW, Barnes M, et al. The prevalence of atrial fibrillation of incident stroke cases and matched population controls in Rochester, Minnesota: changes over three decades. J Am Coll Ca...
- Wolf PA, Benjamin E, Belanger A, et al. Secular trends in the prevalence of atrial fibrillation: The Framingham Study. Am Heart J 1996; 131:790–795. [CrossRef] [PubMed]
- Daniel Levy, Satish Kenchaiah, Martin GLarson, et al. Long-Term Trends in the Incidence of and Survival with Heart Failure. N Engl J Med 2002; 347: 1397–1402. [CrossRef] [PubMed]