According to the Mayo Clinic website, microscopic colitiscan be either collagenous or lymphocytic. Treatment includes a lifestyle change and a change in diet to alleviate the symptoms. Specific Carbohydrate Diet The Specific Carbohydrate Diet (SCD) is a popular diet for colitisand a grain-, lactose- and sucrose-free diet.
Full Answer
What is the best home remedy for colitis?
Home Remedies for Ulcerative Colitis
- Olive Oil. Olive oil is one of the most effective home remedies for mild to moderate ulcerative colitis. ...
- Aloe Vera. Studies have found that aloe vera can help treat mild to moderate ulcerative colitis due to its anti-inflammatory properties.
- Wheat Grass Juice. ...
- Fish Oil. ...
- Slippery Elm. ...
- Psyllium Seeds. ...
- Calendula. ...
- Fenugreek. ...
- Ginger. ...
- Chamomile. ...
How to fix colitis naturally?
Natural Remedies
- Keep a Food Journal. Because ulcerative colitis is triggered by a variety of foods, it’s important to evaluate which foods are problematic for you.
- Drink Plenty of Liquids. It’s common that people with ulcerative colitis become dehydrated. ...
- Acupuncture. ...
- Essential Oils. ...
- Eat Small Meals and Drink Smoothies. ...
What foods should you avoid with colitis?
You should avoid eating food made from any whole grain flour, such as:
- breads
- cereals
- pastas
- noodles
- macaroni
What is the best antibiotic for colitis?
ulcerative colitis, inflammation can develop in the pouch (pouchitis). Pouchitis is often effectively managed with antibiotics. Medication Details Although there are several antibiotics that may be effective, the most commonly prescribed in IBD are: • Metronidazole (Flagyl®) • Ciprofloxacin (Cipro®) • Vancomycin (Vancocin®)

How does a person get colitis?
The exact cause of ulcerative colitis is unknown, but there are things that appear to trigger or aggravate it. It may involve an abnormal immune response against some microorganism in which your tissues are also attacked. Genetics might also play a role. You are at higher risk if a first-degree relative has it.
What is the best treatment for colitis?
What is the best medication for colitis?Best medications for colitisImodium A-D (loperamide)Antidiarrheal agentOralAzulfidine (sulfasalazine)Anti-inflammatory agentOral, rectal, or enemaApriso (mesalamine)Anti-inflammatory agentOral, rectal, or enemaPrednisoneCorticosteroidOral7 more rows•Apr 6, 2021
What is the most common cause of colitis?
Causes of colitis include: Infections caused by a virus or a parasite. Food poisoning due to bacteria. Crohn disease.
How does doctor treat colitis?
People with ulcerative colitis typically need lifelong treatment with medicines unless they have surgery to remove the colon and rectum. aminosalicylates, which doctors prescribe to treat mild or moderate ulcerative colitis or to help people stay in remission.
What foods trigger colitis?
What foods trigger colitis? There are several foods that may trigger your symptoms, including fatty and greasy foods, spicy foods, high-sugar foods, caffeine, alcohol, and carbonated beverages.
How long does colitis take to heal?
Recovery depends on the severity of infection and the type of infection. Some mild-to-moderate cases in children can last for up to three days, while it is evidenced in adults less than a full week. More serious cases can last for up to four weeks.
What should I avoid eating with colitis?
Watch out for items that can be troublemakers if you have UC, including:Alcohol.Caffeine.Carbonated drinks.Dairy products, if you're lactose intolerant.Dried beans, peas, and legumes.Dried fruits.Foods that have sulfur or sulfate.Foods high in fiber.More items...•
What does colitis poop look like?
Stool-related symptoms of ulcerative colitis include: diarrhea. bloody stools that may be bright red, pink, or tarry. urgent bowel movements.
Does colitis go away on its own?
Ulcerative colitis tends to be a progressive condition that does not get better on its own. Without treatment, symptoms may persist and get worse, and inflammation may spread within the colon. There is also a risk for further damage to the lining of the colon with every flare-up.
What foods help heal colitis?
The following foods may be suitable for a person who has just had a flare-up of Crohn's disease or ulcerative colitis:diluted juices.applesauce.canned fruit.oatmeal.plain chicken, turkey, or fish.cooked eggs or egg substitutes.mashed potatoes, white rice, or noodles.sourdough or white bread.
Does colitis always show up on colonoscopy?
Gastroenterologists almost always recommend a colonoscopy to diagnose Crohn's disease or ulcerative colitis. This test provides live video images of the colon and rectum and enables the doctor to examine the intestinal lining for inflammation, ulcers, and other signs of IBD.
Is colitis treated with antibiotics?
Antibiotics can be used for treating the primary disease process of IBD (including luminal disease and fistulizing disease for CD and colitis in the case of UC), for treating bacterial overgrowth, or for treating septic complications of IBD, such as abscesses and post operative wound infections.
When does colitis start?
Ulcerative colitis usually begins before the age of 30. But it can occur at any age, and some people may not develop the disease until after age 60. Race or ethnicity. Although whites have the highest risk of the disease, it can occur in any race. If you're of Ashkenazi Jewish descent, your risk is even higher.
Why does ulcerative colitis occur?
Causes. The exact cause of ulcerative colitis remains unknown. Previously, diet and stress were suspected, but now doctors know that these factors may aggravate but don't cause ulcerative colitis. One possible cause is an immune system malfunction.
What are the different types of ulcerative colitis?
Doctors often classify ulcerative colitis according to its location. Types of ulcerative colitis include: Ulcerative proctitis. Inflammation is confined to the area closest to the anus (rectum), and rectal bleeding may be the only sign of the disease. Proctosigmoiditis.
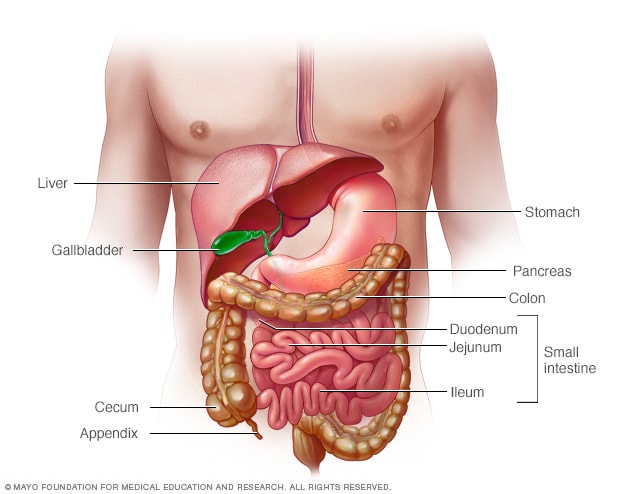
What is the name of the disease that affects the innermost lining of the large intestine?
Ulcerative colitis affects the innermost lining of your large intestine (colon) and rectum. Symptoms usually develop over time, rather than suddenly. Ulcerative colitis can be debilitating and can sometimes lead to life-threatening complications.
How do you know if you have ulcerative colitis?
Ulcerative colitis symptoms can vary, depending on the severity of inflammation and where it occurs. Signs and symptoms may include: Diarrhea, often with blood or pus. Abdominal pain and cramping. Rectal pain. Rectal bleeding — passing small amount of blood with stool. Urgency to defecate.
What is a hole in the colon?
A hole in the colon (perforated colon) Severe dehydration. Bone loss (osteoporosis) Inflammation of your skin, joints and eyes. An increased risk of colon cancer. A rapidly swelling colon (toxic megacolon) Increased risk of blood clots in veins and arteries. By Mayo Clinic Staff. Ulcerative colitis care at Mayo Clinic.
What are the symptoms of bowel movement?
See your doctor if you experience a persistent change in your bowel habits or if you have signs and symptoms such as: Abdominal pain. Blood in your stool. Ongoing diarrhea that doesn't respond to over-the-counter medications. Diarrhea that awakens you from sleep.
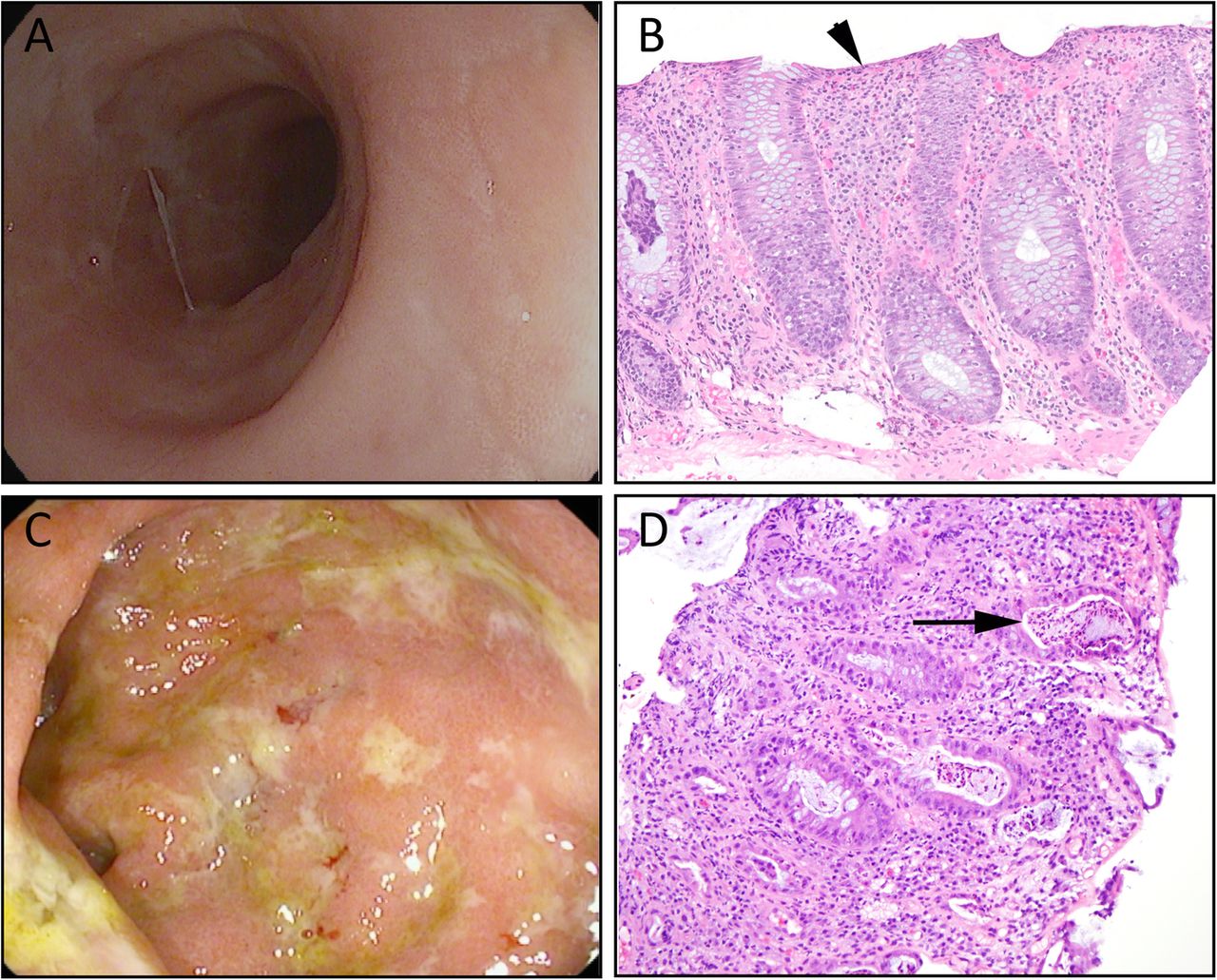
How to confirm microscopic colitis?
To help confirm a diagnosis of microscopic colitis, you may have one or more of the following tests and procedures: Colonoscopy. This exam allows your doctor to view your entire colon using a thin, flexible, lighted tube (colonoscope) with an attached camera. The camera sends images of your rectum and entire colon to an external monitor, ...
What medications can cause microscopic colitis?
Your doctor will also ask about any medications you are taking — particularly aspirin, ibuprofen (Advil, Motrin IB, others), naproxen sodium (Aleve), proton pump inhibitors, and selective serotonin reuptake inhibitors (SSRIs) — which may increase your risk of microscopic colitis.
How far can a doctor see the sigmoid colon?
This procedure is similar to a colonoscopy, but rather than viewing the entire colon, a flexible sigmoidoscopy allows your doctor to view the inside of the rectum and most of the sigmoid colon — about the last 2 feet (61 centimeters) of the large intestine.
What test is used to rule out diarrhea?
In addition to a colonoscopy or flexible sigmoidoscopy, you may have one or more of these tests to rule out other causes for your symptoms. Stool sample analysis to help rule out infection as the cause of persistent diarrhea. Blood test to look for signs of anemia or infection.
What steroid is used for diarrhea?
Steroids such as budesonide (Entocort EC) Medications that block bile acids (which can contribute to diarrhea) such as cholestyramine/aspartame or cholestyramine (Prevalite), or colestipol (Colestid) Anti-inflammatory medications such as mesalamine (Delzicol, Apriso, others) to help control colon inflammation.
How to treat persistent diarrhea?
Your doctor may recommend that you: Eat a low-fat, low-fiber diet. Foods that contain less fat and are low in fiber may help relieve diarrhea. Discontinue dairy products, gluten or both .
Can you take a tissue sample during a colonoscopy?
A tissue sample can be taken through the scope during the exam. Because intestinal issues often appear normal in microscopic colitis, a definite diagnosis of microscopic colitis requires a colon tissue sample (biopsy) obtained during a colonoscopy or flexible sigmoidoscopy. In both subtypes of microscopic colitis, ...
What is the Mayo Clinic for ulcerative colitis?
Pediatric experts at Mayo Clinic's Pediatric Inflammatory Bowel Disease Clinic specialize in providing the care that children require for ulcerative colitis, including diagnostic tests that don't expose your child to radiation and alternative medications that reduce the need for steroids.
What is the Mayo Clinic?
The Inflammatory Bowel Disease Clinic at Mayo Clinic focuses specifically on people with ulcerative colitis and other inflammatory bowel diseases. In addition to routine clinical care, Mayo Clinic doctors are actively involved in research and can provide investigational drug therapy with a variety of drugs for patients who do not respond to standard medical therapy.
Does ulcerative colitis slow growth?
Ulcerative colitis often takes an even greater physical and emotional toll on young people, slowing their growth. At Mayo Clinic, young people and their families work closely with psychologists who can help them navigate the day-to-day difficulties of living with ulcerative colitis.
Does Mayo Clinic treat colitis?
Mayo Clinic surgeons have experience diagnosing and treating ulcerative colitis using the most current management and surgical techniques. Mayo's colorectal surgeons are committed to using minimally invasive surgical procedures, which are associated with less pain and fewer complications.
Does Mayo Clinic require a referral?
In most cases, Mayo Clinic doesn't require a physician referral. Some insurers require referrals, or may have additional requirements for certain medical care.
Can ulcerative colitis be cured during pregnancy?
Women with ulcerative colitis can usually have successful pregnancies, especially if they can keep the disease in remission during pregnancy. It's important to work with a high-risk obstetrician and a gastroenterologist specializing in ulcerative colitis. Mayo Clinic doctors have expertise and experience guiding women with ulcerative colitis through pregnancy and delivery.
How to get rid of ulcerative colitis?
Manage stress. While stress doesn't cause ulcerative colitis, it may make your symptoms worse and may trigger flare-ups. Exercise may help reduce tension and keep your bowels functioning well. Focus on activities you like, such as biking, walking, yoga and swimming .
What foods can you eat to help ulcerative colitis?
However, if you have ulcerative colitis, these foods may make your symptoms worse. Steer clear of nuts, seeds, corn and popcorn, and see if you notice a difference in your symptoms.
What is ulcerative colitis flare up?
An ulcerative colitis flare-up is the return of symptoms after a period of remission. This may involve diarrhea, abdominal pain and cramping, rectal pain and bleeding, fatigue, and urgent bowel movements. Although you may feel helpless against these fluctuations, changes in your diet and lifestyle may help control your symptoms and lengthen ...
Can eating dairy cause ulcerative colitis?
Skip the dairy aisle. There's no firm evidence that diet causes ulcerative colitis. But certain foods and beverages can aggravate your signs and symptoms, especially during a flare-up. Dairy foods are one possible culprit. Try limiting or eliminating milk, yogurt, cheese, ice cream and other dairy products.
How long does it take for ischemic colitis to go away?
Treatment for ischemic colitis depends on the severity of your condition. Signs and symptoms often diminish in two to three days in mild cases. Your doctor may recommend: Treatment for any underlying medical condition, such as congestive heart failure or an irregular heartbeat.
What is the best test for ischemic colitis?
Colonoscopy. This test, which provides detailed images of your colon, can be helpful in diagnosing ischemic colitis. Colonoscopy can also be used to check for cancer, and to see how well a treatment worked. Stool analysis, to rule out infection as a cause of your symptoms.
Why is ischemic colitis confused with other disorders?
Ischemic colitis can often be confused with other disorders because their symptoms overlap, especially inflammatory bowel disease (IBD). Based on your signs and symptoms, your doctor may recommend these imaging tests:
How to repair a hole in the colon?
Remove dead tissue. Repair a hole in your colon. Remove part of the colon that has narrowed because of scarring and is causing a blockage. The likelihood of surgery may be higher if you have an underlying condition, such as heart disease, atrial fibrillation or kidney failure.
What doctor treats digestive disorders?
After an initial evaluation, you may be referred to a doctor who specializes in digestive disorders (gastroenterologist) or blood vessel disorders (vascular surgeon). Here's some information to help you get ready for your appointment, and what to expect from your doctor.
What to do if you can't sit still?
Go to the emergency room if you have severe abdominal pain that makes you so uncomfortable that you can't sit still. You may be referred for immediate surgery to diagnose and treat your condition. If your signs and symptoms are moderate and occasional, call your doctor for an appointment.
How to tell if you have microscopic colitis?
Microscopic colitis is a medical condition a doctor can only identify by looking at a tissue sample of the colon under a microscope. A doctor will view signs of inflammation, such as lymphocytes, which are a kind of white blood cell.
How do you know if you have colitis?
Depending on your condition, you may experience one or more of the following symptoms: abdominal pain or cramping. bloating in your abdomen. weight loss. diarrhea with or without blood. blood in your stool. urgent need to move your bowels. chills or fever.
Why is my colon thick?
Collagenous colitis occurs when the colon’s lining becomes thicker than usual due to a buildup of collagen under the outermost layer of tissue.
How long does it take for colitis to develop in a baby?
Allergic colitis is a condition that can occur in infants, usually within the first two months after birth . The condition can cause symptoms in infants that include reflux, excessive spitting up, fussiness, and possible flecks of blood in a baby’s stool. Doctors don’t know exactly what causes allergic colitis.
What is the name of the disease that occurs when the bacterium Clostridium difficile is overgrowth?
Pseudomembranous colitis. Pseudomembranous colitis (PC) occurs from overgrowth of the bacterium Clostridium difficile. This kind of bacteria normally lives in the intestine, but it doesn’t cause problems because it’s balanced by the presence of “good” bacteria.
What is IC in a patient?
Ischemic colitis. Ischemic colitis (IC) occurs when blood flow to the colon is suddenly cut off or restricted. Blood clots can be a reason for sudden blockage. Atherosclerosis, or buildup of fatty deposits, in the blood vessels that supply the colon is usually the reason for recurrent IC.
What foods can cause colitis in a newborn?
Examples include cow’s milk, eggs, and wheat. If baby stops having symptoms, these foods were likely the culprit.
What are the different types of ulcerative colitis?
Other types of ulcerative colitis include: proctosigmoiditis, in which the rectum and a section of your colon known as the sigmoid colon have inflammation and ulcers. proctitis, which affects just your rectum.
What is the best treatment for pancolitis?
The most common treatments for pancolitis and other forms of UC are anti-inflammatory drugs. These help treat the inflammation in your colon. These include medications such as oral 5-aminosalicylates (5-ASAs) and corticosteroids.
What is the most common cause of pancolitis?
Pancolitis is an inflammation of the entire colon. The most common cause is ulcerative colitis (UC). Pancolitis can also be caused by infections like C. difficile, or can be associated with inflammatory disorders like rheumatoid arthritis (RA).
Why is a flare up more severe than UC?
Flare-ups in pancolitis may be more severe than in other forms of UC, because more of the colon is affected in pancolitis. If UC is left untreated, potential complications include: colorectal cancer. gastrointestinal perforation, or a hole in your colon. toxic megacolon.
How do you know if you have pancolitis?
Symptoms of pancolitis. Common mild and moderate symptoms of pancolitis include: feeling exhausted. abnormal weight loss (without more exercise or dieting) pain and cramps in the area of your stomach and abdomen. feeling a strong, frequent urge for bowel movements, but not always being able to control the bowel movements.
What is UC in the colon?
UC is a chronic condition that affects the lining of your large intestine, or your colon. UC is caused by inflammation that leads to ulcers, or sores, in your colon. In pancolitis, inflammation and ulcers have spread to cover your entire colon. Other types of ulcerative colitis include:
Why does my colon hurt?
It’s thought that the immune system may mistakenly target your colon while attacking bacteria or viruses that cause infections in your colon. This can cause inflammation and damage to your colon, which can lead to ulcers. It can also make it harder for your body to absorb certain nutrients. Environment may play a role.
Diagnosis
- Endoscopic procedures with tissue biopsy are the only way to definitively diagnose ulcerative colitis. Other types of tests can help rule out complications or other forms of inflammatory bowel disease, such as Crohn's disease. To help confirm a diagnosis of ulcerative colitis, you may hav…
Clinical Trials
- Explore Mayo Clinic studiestesting new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Lifestyle and Home Remedies
- Sometimes you may feel helpless when facing ulcerative colitis. But changes in your diet and lifestyle may help control your symptoms and lengthen the time between flare-ups. There's no firm evidence that what you eat actually causes inflammatory bowel disease. But certain foods and beverages can aggravate your signs and symptoms, especially during a flare-up. It can be helpfu…
Alternative Medicine
- Many people with digestive disorders have used some form of complementary and alternative medicine (CAM). However, there are few well-designed studies showing the safety and effectiveness of complementary and alternative medicine. Although research is limited, there is some evidence that adding probiotics along with other medications may be helpful, but this has …
Preparing For Your Appointment
- Symptoms of ulcerative colitis may first prompt you to visit your primary care doctor. Your doctor may recommend you see a specialist who treats digestive diseases (gastroenterologist). Because appointments can be brief, and there's often a lot of information to discuss, it's a good idea to be well prepared. Here's some information to help you get ready, and what to expect from your doct…
Diagnosis
Treatment
Lifestyle and Home Remedies
Preparing For Your Appointment