How long will I live with chronic pancreatitis?
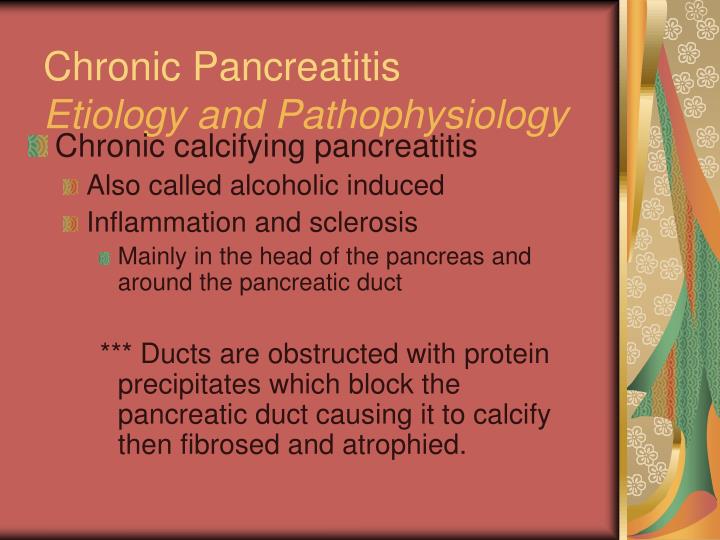
· Chronic calcifying/calcific pancreatitis (CCP) is a special form of chronic pancreatitis that tends to calcify or is associated with pancreatic lithiasis. Popular Trending
What is the best treatment for chronic pancreatitis?
· Chronic pancreatitis is an inflammation of your pancreas that doesn’t improve over time. The pancreas is an organ located behind your stomach. It makes enzymes, which are special proteins that help...
What are the stages of chronic pancreatitis?
chronic calcifying pancreatitis a form accompanying chronic hepatitis and precipitated by chronic alcohol abuse. Miller-Keane Encyclopedia and Dictionary of Medicine, Nursing, and Allied Health, Seventh Edition. © 2003 by Saunders, an imprint of Elsevier, Inc.
How can you cure pancreatitis?
Chronic pancreatitis is a painful disease of the pancreas in which inflammation has resolved, but with resultant damage to the gland characterized by fibrosis, calcification and ductal inflammation. It is possible for patients with chronic pancreatitis to have episodes of …
How serious is chronic calcific pancreatitis?
Chronic pancreatitis causes severe damage to your pancreas. This means that your body won't be able to make needed enzymes and hormones. This can result in malnutrition, because you won't be able to digest foods. Chronic pancreatitis can also cause diabetes.
Is chronic calcific pancreatitis curable?
Treatment for chronic pancreatitis focuses on reducing your pain and improving your digestive function. The damage to your pancreas can't be undone, but with the proper care, you should be able to manage many of your symptoms. Treatment for pancreatitis can include medication, endoscopic therapies, or surgery.
What is the treatment for calcification of the pancreas?
ESWL is a safe and effective preferred treatment for selected patients with painful calcified chronic pancreatitis. Combining systematic endoscopy with ESWL adds to the cost of patient care, without improving the outcome of pancreatic pain.
What causes calcification in chronic pancreatitis?
Pancreatic calcifications are being detected more frequently because of the widespread use of imaging, particularly CT. Pancreatic calcifications are most commonly associated with chronic pancreatitis related to alcohol abuse. Several other pathologic entities, however, can cause pancreatic calcifications.
Can you live a long life with chronic pancreatitis?
Chronic pancreatitis can have serious and long-lasting effects. But with lifestyle changes and effective treatments, patients with this condition can reduce their pain and live a more normal life.
How long can you survive with chronic pancreatitis?
The overall survival rate is 70% at 10 years and 45% at 20 years. In an international study, 559 deaths occurred among patients with chronic pancreatitis, compared with an expected number of 157, which creates a standard mortality ratio of 3.6.
What can you do for chronic pancreatitis?
Chronic Pancreatitis Treatment: MedicationAnalgesics. Analgesics are pain reducers. ... Enzyme Therapy. ... High-protein, High-calorie Diets. ... Puestow Procedure (Longitudinal Pancreaticojejunostomy) ... Whipple Procedure (Pancreaticoduodenectomy) ... Total Pancreatectomy and Auto Islet Transplantation.
Is chronic pancreatitis painful?
Pain is the predominant symptom in chronic pancreatitis; 80–90% of patients present with pain as the primary symptom either at the first attack of acute pancreatitis or as the main reason for hospital readmissions in the following months and years, as the disease progresses to what could be defined as chronic ...
What is end stage chronic pancreatitis?
Stage C is the end stage of chronic pancreatitis, where pancreatic fibrosis has led to clinical exocrine and/or endocrine pancreatic function loss (steatorrhea and/or diabetes mellitus). Complications of chronic pancreatitis might or might not be present.
Is chronic pancreatitis reversible?
The changes of chronic pancreatitis are not reversible. However, it is possible to have control of pain and steatorrhea with medical, endoscopic, percutaneous or surgical treatment.
What is the diet for pancreatitis?
To best achieve those goals, it is important for pancreatitis patients to eat high protein, nutrient-dense diets that include fruits, vegetables, whole grains, low fat dairy, and other lean protein sources. Abstinence from alcohol and greasy or fried foods is important in helping to prevent malnutrition and pain.
Can chronic pancreatitis be reversed?
The changes of chronic pancreatitis are not reversible.
Is there any hope for chronic pancreatitis?
Chronic pancreatitis affects children (pediatric pancreatitis) and adults. Unfortunately, for people suffering from chronic pancreatitis, there is no treatment. The only hope for some patients is the removal of the pancreas through a major surgery.
What is the newest treatment for chronic pancreatitis?
Combined treatment with extracorporeal shock-wave lithotripsy and endoscopic lithotripsy is a useful, minimally invasive, first-line treatment approach that can preserve pancreatic exocrine function.
Can you stop progression of chronic pancreatitis?
Chronic pancreatitis is a chronic condition characterized by pancreatic inflammation that causes fibrosis and the destruction of exocrine and endocrine tissues. Chronic pancreatitis is a progressive disease, and no physiological treatment is available to reverse its course.
Is pancreatitis a chronic disease?
Pancreatitis is considered acute when the inflammation comes on suddenly and only lasts for a short period of time. It’s considered chronic when it keeps coming back or when the inflammation doesn’ t heal for months or years.
Is pancreatitis an acute condition?
Pancreatitis is considered acute when the inflammation comes on suddenly and only lasts for a short period of time. It’s considered chronic when it keeps coming back or when the inflammation doesn’t heal for months or years. Chronic pancreatitis can lead to permanent scarring and damage.
Can pancreatitis cause scarring?
Chronic pancreatitis can lead to permanent scarring and damage. Calcium stones and cysts may develop in your pancreas, which can block the duct, or tube, that carries digestive enzymes and juices to your stomach. The blockage may lower the levels of pancreatic enzymes and hormones, which will make it harder for your body to digest food ...
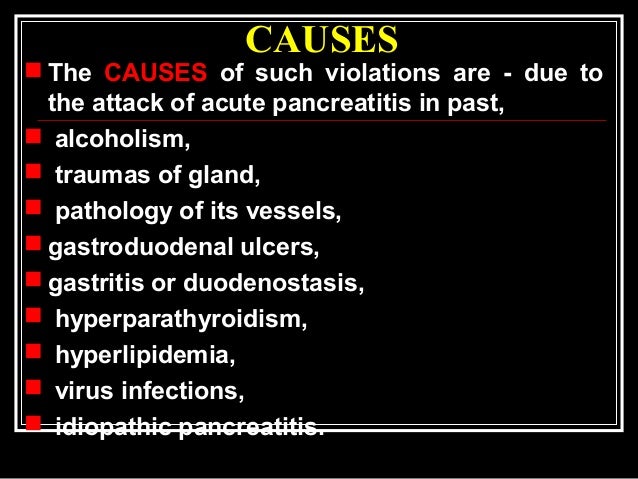
What causes pancreatitis?
There are numerous different causes of chronic pancreatitis. The most common cause is long-term alcohol abuse. Approximately 70 percent of cases are linked to alcohol consumption. Autoimmune disease occurs when your body mistakenly attacks your healthy cells and tissues.
Does alcohol cause pancreatitis?
Abusing alcohol increases your risk of developing chronic pancreatitis. Smoking is believed to increase the risk of pancreatitis among alcoholics. In some cases, a family history of chronic pancreatitis can increase your risk. Chronic pancreatitis most frequently develops in people between the ages of 30 and 40.
What is the cause of pancreatitis in children?
The exact cause of tropical pancreatitis is unknown, but it may be related to malnutrition.
How to treat pancreatitis?
Treatment for pancreatitis can include medication, endoscopic therapies, or surgery.
Is pancreatitis a chronic disease?
Pancreatitis can be acute (beginning suddenly, usually with the patient recovering fully) or chronic (progressing slowly with continued, permanent injury to the pancreas).
What is the difference between chronic pancreatitis and acute pancreatitis?
Inflammation of the pancreas. This may be a sharp, severe illness (acute pancreatitis) or a recurrent disorder (chronic pancreatitis). Acute pancreatitis is often due to blockage of the outflow from the gland by a gallstone stuck in the common outlet of the pancreatic and bile ducts, with digestion of the pancreatic tissue by its own enzymes. There is sudden severe pain in the abdomen, nausea, vomiting and shock. Chronic pancreatitis is usually related to heavy alcohol consumption. X-ray or CT scan shows that the pancreas is full of cysts, many of them filled with chalky stones. Attacks are short, severe and tend to recur. Extensive damage to the pancreas may result and this can cause DIABETES. Continued drinking by people with chronic pancreatitis carries a high mortality.
Where is the pancreas located?
Thepancreasislocated in the midline of the back of the abdomen, closely associated with the liver, stomach, and duodenum (the first part of the small intestine). The pancreas is considered a gland.
Is the pancreas a gland?
The pancreas is considered a gland. A gland is an organ whose primary function is to produce chemicals that pass either into the main blood circulation (called an endocrine function), or pass into another organ (called an exocrine function). The pancreas is unusual because it has both endocrine and exocrine functions.
Which hormones are produced by the pancreas?
Its endocrine function produces three hormones. Two of these hormones, insulin and glucagon, are central to the processing of sugars in the diet (carbohydrate metabolism or breakdown). The third hormone produced by the endocrine cells of the pancreas affects gastrointestinal functioning.
What is the function of the pancreas?
The pancreas's exocrine function produces a variety of digestive enzymes (trypsin, chymotrypsin, lipase, and amylase, among others). These enzymes are passed into the duodenum through a channel called the pancreatic duct.
What happens to the pancreas after a pancreatitis attack?
After an attack of acute pancreatitis, tissue and cells of the pancreas return to normal. With chronic pancreatitis, damage to the pancreas occurs slowly over time. Symptoms may be persistent or sporadic, but the condition does not disappear and the pancreas is permanently impaired.
Is pancreatitis a chronic disease?
More than 80 percent of the cases of acute pancreatitis are related to biliary stones or alcohol use. Acute pancreatitis may lead to chronic pancreatitis. Chronic pancreatitis is a painful disease of the pancreas in which inflammation has resolved, but with resultant damage to ...
Can pancreatitis cause chronic pancreatitis?
Acute pancreatitis may lead to chronic pancreatitis. Chronic pancreatitis is a painful disease of the pancreas in which inflammation has resolved, but with resultant damage to the gland characterized by fibrosis, calcification and ductal inflammation. It is possible for patients with chronic pancreatitis to have episodes of acute pancreatitis.
Can chronic pancreatitis be caused by alcohol?
It is possible for patients with chronic pancreatitis to have episodes of acute pancreatitis. The most common cause of chronic pancreatitis in Western societies is alcohol. Alcohol consumption has been implicated in approximately 70 percent of cases as a major cause of this disease.
What is the cause of pancreatitis in children?
Its cause is unknown, although malnutrition is suspected to play a role. Several major physiological factors contribute to the development of chronic pancreatitis in alcoholic patients.
Does alcohol cause pancreatitis?
Several major physiological factors contribute to the development of chronic pancreatitis in alcoholic patients. Alcohol may change the composition of proteins secreted by the pancreas, resulting in the formation of protein plugs within the small pancreatic ducts.
Can pancreatitis radiate to the back?
The pain of chronic pancreatitis often radiates to the back, although it may radiate to both upper and lower quadrants. Sitting up and leaning forward may relieve or reduce discomfort. Diarrhea may be chronic (six or more bowel movements per day).
What are the complications of chronic pancreatitis?
Nutrient malabsorption, diabetes mellitus and splenic vein thrombosis are common complications of chronic pancreatitis. Malabsorption is faulty absorption of nutrients from the digestive tract. In chronic pancreatitis, malabsorption occurs after the capacity for enzyme secretion is reduced by more than 90 percent.
What are the symptoms of chronic pancreatitis?
Symptoms are occasional and include: Severe belly (abdominal) pain that may be constant or that comes back. Chronic pancreatitis causes severe damage to your pancreas.
Can chronic pancreatitis cause diabetes?
Chronic pancreatitis causes severe damage to your pancreas. This means that your body won't be able to make needed enzymes and hormones. This can result in malnutrition, because you won't be able to digest foods. Chronic pancreatitis can also cause diabetes. This happens because your pancreas can't make insulin.
What organ makes insulin?
Your pancreas is an organ with many important functions. It makes enzymes that help you digest food. It also makes insulin to keep your blood sugar levels under control. Short-term (acute) pancreatitis is a sudden inflammation of your pancreas. This can be very painful.
Can pancreatitis cause nausea?
This can be very painful. You may have nausea, vomiting, and fever. If your acute pancreatitis doesn’t get better and slowly gets worse, you may have chronic pancreatitis.
Why does my pancreas hurt?
This causes pain and scarring. The trapped enzymes slowly cause severe damage to your pancreas. The most common cause of chronic pancreatitis is drinking a lot of alcohol over a long period of time.. Other causes include: An attack of acute pancreatitis that damages your pancreatic ducts.
How do you know if you have pancreatitis?
Symptoms are occasional and include: Pain in the upper belly that spreads into the back. Pain in the belly that gets worse when you eat or drink alcohol. Diarrhea or oily stools.
What does it mean when your belly hurts?
Symptoms are occasional and include: Severe belly (abdominal) pain that may be constant or that comes back. Chronic pancreatitis causes severe damage to your pancreas. This means that your body won't be able to make needed enzymes and hormones.
What is the etiology of pancreatitis?
Chronic pancreatitis is an irreversible and progressive disorder of the pancreas characterized by inflammation, fibrosis, and scarring. Exocrine and endocrine functions are lost, often leading to chronic pain. The etiology is multifactorial, although alcoholism is the most significant risk factor in adults. The average age at diagnosis is 35 ...
Is pancreatitis a progressive disease?
References. Chronic pancreatitis is an irreversible and progressive disorder of the pancreas characterized by inflammation, fibro sis, and scarring. Exocrine and endocrine functions are lost, often leading to chronic pain. The etiology is multifactorial, although alcoholism is the most significant risk factor in adults.
Does antioxidant therapy help with pancreatitis?
3. Antioxidant therapy does not improve pain control or mortality outcomes in patients with chronic pancreatitis. B. 10, 35. Pancreatic enzyme replacement is indicated for steatorrhea and malabsorption and may help relieve pain in patients with chronic pancreatitis.
What is the most common cause of pancreatitis in children?
Alcoholism is the most significant risk factor for the development of chronic pancreatitis, accounting for 70% of cases in adults. Genetic disease, especially cystic fibrosis, and anatomic abnormalities are the most common causes in children .
Can you have surgery for pancreatitis?
One-half of patients with chronic pancreatitis will eventually require surgery, 1 most commonly because of intractable, disabling pain. 51 Indications for surgery are listed in Table 5. 15 There are two types of surgeries for chronic pancreatitis. Decompression procedures are performed on patients with large duct disease, whereas resection procedures are performed on patients with small duct disease or pancreatic head enlargement.
Is pancreatic cancer a hereditary disease?
The risk of pancreati c cancer is increased in patients with chronic pancreatitis, especially hereditary pancreatitis. Although it is not known if screening improves outcomes, clinicians should counsel patients on this increased risk and evaluate patients with weight loss or jaundice for neoplasm.
How does alcohol and tobacco affect cancer?
Eliminating alcohol and tobacco use slows disease progression and lessens complications, such as cancer. 33 Dietary changes, particularly eating small, frequent, low-fat meals, can also help decrease pain and complications. 2, 3, 10, 34
What is chronic pancreatitis?
Chronic or calcifying pancreatitis is a continuing inflammatory response characterized by severe morphological changes (such as irregular sclerosis and permanent loss of exocrine parenchyma), which may be focal, segmental, or diffused. Clinically, chronic pancreatitis is characterized by recurrent or persisting abdominal pain, although chronic pancreatitis may also present without pain. Chronic pancreatitis does not resolve by itself and could progress to a slow destruction of the pancreatic gland. Irrespective of etiology, the clinical pattern of chronic pancreatitis is characterized by the recurrent episodes of acute pancreatitis in the early stages followed by pancreatic insufficiency, steatorrhea, pancreatic calcification and, maybe, diabetes mellitus at the chronic stage. However, an intra-acinar activation of zymogens in the gland itself is the primary cause of pancreatic injury and pancreatitis ( Lankisch and Banks, 1998 ).
What is the percentage of calcifications in the pancreas?
Typical pancreatic calcifications are diagnostic of chronic pancreatitis. They develop in 40% to 60% of patients with alcoholic pancreatitis, and approximately 90% of calcific pancreatitis is caused by alcoholism.
Can pancreatic calcification be seen on a plain abdominal radiograph?
The finding of diffuse pancreatic calcification on a plain abdominal radiograph is specific for chronic pancreatitis but is seen only in far-advanced disease. Focal pancreatic calcification may be due to other conditions such as trauma, islet-cell tumors, or hypercalcemia.
Where do calcifications occur?
Calcifications most commonly occur in pancreatic head (and may be clustered in that location) ○. Other CT stigmata of chronic pancreatitis include dilated, beaded pancreatic duct (± strictures), parenchymal atrophy, and pseudocysts. –.
Does pancreatitis cause pain?
Clinically, chronic pancreatitis is characterized by recurrent or persisting abdominal pain, although chronic pancreatitis may also present without pain. Chronic pancreatitis does not resolve by itself and could progress to a slow destruction of the pancreatic gland.
What is the sensitivity of a transabdominal ultrasound?
Overlying bowel gas can interfere with visualization of the pancreas, making the sensitivity of ultrasound greater than that of plain X rays but less than that of CT.
Is MRCP accurate?
MRCP is most accurate in advanced chronic pancreatitis but the accuracy with less-advanced chronic pancreatitis is substantially reduced.
Chronic Pancreatitis Treatment: Medication
For patients with chronic pain that cannot be controlled otherwise, we may recommend medication.
Chronic Pancreatitis Treatment: Surgery
When medical and endoscopic therapies have failed, we may recommend surgery. There are many surgical options. Different procedures work better for different patients. We will work closely with you to find the surgical approach that offers you the best outcome.
Chronic Pancreatitis Treatment: Celiac Nerve Block
In the advanced stages of chronic pancreatitis, oral drugs may not be enough to control the pain. Your doctor may recommend a nerve block, which is an injection of an anesthetic around your nerve. The injection stops the nerves from sending pain messages.
Chronic Pancreatitis Treatment: Endoscopic Therapy
Your doctor may be able to treat chronic pancreatitis using endoscopic procedures.
Chronic Pancreatitis: Treating Complications
Chronic pancreatitis can cause complications in other parts of the body. Part of treating the disease is to treat and manage those complications. Depending on the complication and the severity, we can treat it endoscopically, surgically or using percutaneous therapy.