TB blood tests (sometimes called IGRAs) use a blood sample to find TB infection. The tests measure the response of TB proteins when they are mixed with a small amount of blood. Only one visit is required to draw blood for this test.
Full Answer
What are the diagnostic considerations for tuberculosis (TB) disease?
The standard of care for initiating treatment of TB disease is four-drug therapy. Treatment with a single drug can lead to the . development of a bacterial population resistant to that drug. Study Questions. 6.1 The major goals for treatment of TB disease include which of the following? A. Curing the individual patient. B.
How is tuberculosis (TB) treated under the dot?
The medications used to treat latent TB infection include the following: Isoniazid (INH) Rifapentine (RPT) Rifampin (RIF) These medications are used on their own or in combination, as shown in the table below. CDC and the National Tuberculosis Controllers Association (NTCA) preferentially recommend short-course, rifamycin-based, 3- or 4-month ...
Is there a single test cutoff point for tuberculosis (TB)?
Apr 08, 2020 · The most common treatment for active TB is isoniazid INH in combination with three other drugs—rifampin, pyrazinamide and ethambutol. You may begin to feel better only a few weeks after starting to take the drugs but treating TB …
How often should patients with extrapulmonary tuberculosis (TB) be monitored?
May 14, 2019 · A tuberculosis (TB) infection control plan is part of a general infection control program designed to ensure the following: prompt detection of infectious TB patients, airborne precautions, and. treatment of people who have suspected or confirmed TB disease. In all health care settings, particularly those in which people are at high risk for ...
How do you monitor a patient for TB treatment?
What are the activities you would perform in order to monitor a patients response to treatment?
What are the measures of tuberculosis?
What three 3 measures can be taken to control tuberculosis on a community level?
How do you ensure a patient to follow up?
- Phone. Talking on the phone allows patients to ask questions and staff to reiterate important points.
- Secure email. Secure email is part of many patient portals and can be an effective way to communicate with patients. ...
- Texting. ...
- Postal mail. ...
- Automated calling system.
Why are follow up visits necessary in patient care?
What are the 3 stages of tuberculosis?
What measures are required for secondary prevention of tuberculosis?
What is the primary prevention of tuberculosis?
What do standard precautions measure?
How long does it take to treat TB?
As a general rule, the principles used for the treatment of pulmonary TB disease also apply to extrapulmonary forms of the disease. A 6-month treatment regimen is recommended for patients with extrapulmonary TB disease, unless the organisms are known or strongly suspected to be resistant to the first-line drugs. If PZA cannot be used in the initial phase, the continuation phase must be increased to 7 months. The exception to these recommendations is central nervous system TB, for which the optimal length of therapy has not been established but some experts recommend 9 to 12 months. Most experts do recommend corticosteroids to be used as additional therapy for patients with TB meningitis and pericarditis. Consultation with a TB expert is recommended.
How to educate patients about TB?
Educating patients about TB disease helps ensure their successful completion of therapy. Health-care providers must take the time to explain clearly to patients what medication should be taken, how much, how often, and when. Patients should be clearly informed about possible adverse reactions to the medications they are taking and when to seek necessary medical attention. Providing patients with the knowledge they need regarding the consequences of not taking their medicine correctly is very important. In addition, patients should be educated about infection control measures and potential need for isolation (Table 6.1). HIV testing and counseling is recommended for all patients with TB disease in all health-care settings. The patient must first be notified that testing will be performed. The patient has the right to decline HIV testing and counseling (opt-out screening).
What are the four drugs that are included in the initial treatment regimen?
Four drugs— INH, RIF, PZA, and EMB — should be included in the initial treatment regimen until the results of drug-susceptibility tests are available. Each of the drugs in the initial regimen plays an important role. INH and RIF allow for short-course regimens with high cure rates. PZA has potent sterilizing activity, which allows further shortening of the regimen from 9 to 6 months. EMB helps to prevent the emergence of RIF resistance when primary INH resistance is present. If drug-susceptibility test results are known and the organisms are fully susceptible, EMB need not be included. For children whose clarity or sharpness of vision cannot be monitored, EMB is usually not recommended except when the risk of drug resistance is high or for children who have “adult-type” (upper lobe infiltration, cavity formation) TB disease.
How long is the TB continuation phase?
The continuation phase of treatment is given for either 4 or 7 months. The 4-month continuation phase should be used in patients with uncomplicated, noncavitary, drug-susceptible TB, if there is documented sputum conversion within the first 2 months. The 7-month continuation phase is recommended only for
What is the recommended treatment regimen based on?
The recommended treatment regimens are based, in large part, on evidence from clinical trials and are rated on the basis of a system developed by the U.S. Public Health Service (USPHS) and the Infectious Diseases Society of America (IDSA) (Table 6.3).
What are the drugs that treat TB?
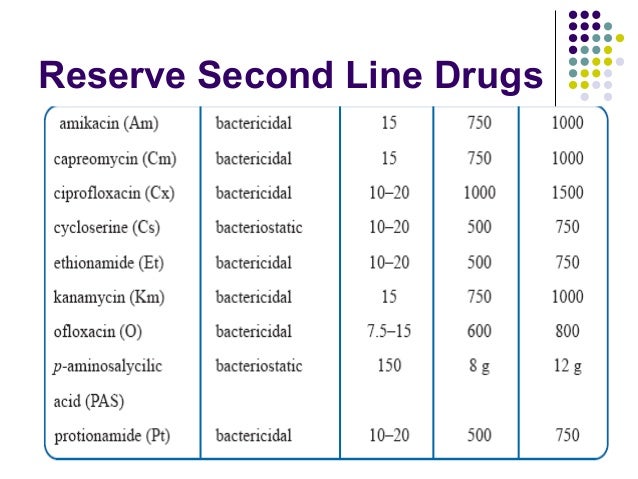
Food and Drug Administration (FDA) for the treatment of TB disease (Table 6.2). In addition, the fluoroquinolones (levofloxacin, moxifloxacin, and gatifloxacin), although not approved by the FDA for TB disease, are commonly used to treat TB disease caused by drug-resistant organisms or for patients who are intolerant of some first-line drugs. Rifabutin, approved for use in preventing Mycobacterium avium complex disease in patients with HIV infection but not approved for TB disease, is useful for treating TB disease in patients concurrently taking drugs that interact with rifampin (e.g., certain antiretroviral drugs). Amikacin and kanamycin, nearly identical aminoglycoside drugs used in treating patients with TB disease caused by drug-resistant organisms, are not approved by the FDA for treatment of TB.
How long does it take to develop a TB control plan?
For each patient with newly diagnosed TB disease, a specific treatment and monitoring plan should be developed in collaboration with the local TB control program within 1 week of the presumptive diagnosis. This plan should include:
What should a clinic decide on TB treatment?
Clinicians should choose the appropriate treatment regimen based on drug susceptibility results of the presumed source case (if known), coexisting medical conditions (e.g., HIV. ), and potential for drug-drug interactions. Consultation with a TB expert is advised if the known source of TB infection has drug-resistant TB.
What is the name of the drug that is used to treat TB?
Isoniazid (INH) Rifapentine (RPT) Rifampin (RIF) These medications are used on their own or in combination, as shown in the table below. CDC and the National Tuberculosis Controllers Association (NTCA) preferentially recommend short-course, rifamycin-based, 3- or 4-month latent TB infection treatment regimens over 6- or 9-month isoniazid ...
Is 6H a good treatment for TB?
If short-course treatment regimens are not a feasible or an available option, 6H and 9H are alternative, effective latent TB infection treatment regimens. Although effective, 6H and 9H have higher toxicity risk and lower treatment completion rates than most short-term treatment regimens.
Why should TB be encountered infrequently during the domestic medical screening examination?
TB disease should be encountered infrequently during the domestic medical screening examination because all new arrivals have been screened for TB disease prior to departure. Clinicians should be aware that the overseas medical exam is aimed at diagnosing pulmonary TB disease and may fail to detect extrapulmonary disease. Therefore, it is important for clinicians to perform a thorough history and physical examination aimed at identifying any refugee who may have pulmonary or extrapulmonary TB disease. Some persons with TB disease have minimal symptoms, and a high index of suspicion should be maintained for those with any concerning history, such as household exposure to TB, or signs of active disease.
What are the classifications for TB?
If the IGRA or TST is positive and there is no evidence of TB disease, there will be two classifications, B2 and B3; if negative, B3 only. Additional information can be found in the Contacts of Tuberculosis Cases section.
What is an IGRA test?
An IGRA is a blood test used to determine if a person is infected with M. tuberculosis. IGRAs measure the immune response to TB proteins in whole blood. Currently, QuantiFERON®-TB Gold Plus (as of March 2020 manufactured by Qiagen) and T-SPOT®. TB (Oxford Immunotec) are the two IGRAs currently approved in the United States. It is important to note that TB blood tests should not be performed on a person who has written documentation of either a previous positive TB test result (TB blood test or TST) or treatment for TB disease.
When is sputum collected for smear and culture?
When the CXR has suspicious findings, or other signs or symptoms of TB are present , sputum specimens must be collected for smear and culture testing. Further information on testing can be found in the ATS/CDC/IDSA Clinical Practice Guidelines: Diagnosis of Tuberculosis in Adults and Children
How long is a travel clearance valid for?
Travel clearance is valid for 6 months from the time the evaluation is complete.
Does LTBI have a negative sputum smear?
Usually has a normal chest x-ray and has negative sputum smears and cultures. May have an abnormal chest x-ray or positive sputum smear or culture. Needs treatment for LTBI to prevent TB disease. Needs treatment for TB disease. Source: CDC Division of Tuberculosis Elimination.
Can a TST test be performed on a child?
However, the test is contraindicated for persons who have had a local reaction with blistering or a systemic allergic response. False negative results may be more frequent in young children and in persons with a compromised immune system. False negatives also may occur more commonly in populations with highly prevalent M. tuberculosis infection (a high pretest probability). A TST should be administered and read by a specifically trained healthcare provider. For additional information about performing a TST, visit the CDC TB website.
How long does it take to treat TB?
The treatment for this type of TB takes much longer, 20 to 30 months to complete, and you may experience more side effects.
What is the best treatment for TB?
The most common treatment for active TB is isoniazid INH in combination with three other drugs—rifampin, pyrazinamide and ethambutol. You may begin to feel better only a few weeks after starting to take the drugs but treating TB takes much longer than other bacterial infections.
What is DOT therapy?
This means a healthcare worker will come to you to administer your medication and eliminate the concern of forgetting to take the treatment.
What are the side effects of TB?
While you are in treatment for active TB disease, you will need regular checkups to make sure your treatment is working. Everyone is different, but there are side effects associated with taking the medications, including: 1 Upset stomach, nausea and vomiting or loss of appetite 2 Tingling or numbness in the hands or feet 3 Itchy skin, rashes or bruising 4 Changes in your eyesight or blurred visions 5 Yellowish skin or eyes 6 Dark-colored urine 7 Weakness, fatigue or fever that for three or more days
What are the symptoms of TB?
Yellowish skin or eyes. Dark-colored urine. Weakness, fatigue or fever that for three or more days. It is important to tell your doctor or TB nurse immediately if you begin having any unusual symptoms while taking medicine for either preventive therapy or for active TB disease.
What to take for TB tingling?
If you are having trouble with tingling and numbness, your doctor may prescribe a vitamin B6 supplement while you are in treatment. It may also be possible to change TB medications if your side effects are serious.
Can you get TB from taking too much medicine?
You must finish your medicine and take the drugs exactly as prescribed. If you stop taking the drugs too soon you can become sick again and potentially spread the disease to others. Additionally, by taking the drugs incorrectly, TB germs that are still alive may become drug-resistant, making it harder for you to get better next time.
What is a TB control plan?
A tuberculosis (TB) infection control plan is part of a general infection control program designed to ensure the following: 1 prompt detection of infectious TB patients, 2 airborne precautions, and 3 treatment of people who have suspected or confirmed TB disease.
What are the measures to reduce the risk of exposure?
The following measures can be taken to reduce the risk for exposure: Implementing a respiratory protection program; Training health care personnel on respiratory protection; and. Educating patients on respiratory hygiene and the importance of cough etiquette procedures. Page last reviewed: May 14, 2019.
What are administrative measures?
Administrative measures. Environmental controls. Use of respiratory protective equipment. On May 17, 2019, the Centers for Disease Control and Prevention (CDC) and the National Tuberculosis Controllers Association.
What test is used to diagnose TB?
A TB skin test is the most common type of test used to diagnose suspected active TB. However, it is not suitable for everyone. Blood tests are also used, though not as frequently.
What is a TB skin test?
Interpreting Results. A TB skin test shows if your immune system has responded to the bacterium that causes tuberculosis (TB). It is also called a PPD test, tuberculin test, or Mantoux test. The test involves injecting a small amount of fluid containing certain components of the TB bacterium under the skin.
How much PPD is in a forearm?
During the test, 0.1 milliliters (mL) of tuberculin purified protein derivative (PPD), also referred to as tuberculin, will be injected just under the skin of your forearm. 5 The injection will be done with a small needle, so you should only feel a slight pinch and it should be over very quickly.
How many visits to a healthcare professional for a sex test?
The test requires two visits to your healthcare professional. The test itself will be administered on the first visit, with the results read on the second.
What does it mean when a skin test is positive for TB?
If your skin test is positive, it means you are infected with the TB bacteria but further testing will be needed to see whether it is a latent or active infection. 1. The test requires two visits to your healthcare professional.
How long does it take to get a blood test interpreted?
Remember to book your follow-up appointment to get your test interpreted. This needs to be done within 48-72 hours of the test being administered. If you do not come back for your follow-up within this time, you will need to get the test redone because they will not be able to interpret the test.
What is a false negative TB test?
False Negative TB Skin Tests. A false negative is a test result that wrongly indicates that you do not have TB when you do. Factors that might cause a false-negative are: 5. Anergy, the absence of the normal immune response to a particular antigen or allergen. Recent infection, within the past eight to 10 weeks.
What are the objectives of tuberculosis treatment?
The objectives of tuberculosis therapy are (1) to rapidly reduce the number of actively growing bacilli in the patient, thereby decreasing severity of the disease , preventing death and halting transmission of M. tuberculosis; (2) to eradicate populations of persisting bacilli in order to achieve durable cure (prevent relapse) after completion of therapy; and (3) to prevent acquisition of drug resistance during therapy.
What is the responsibility of a tuberculosis patient?
The responsibility for successful treatment of tuberculosis is placed primarily on the provider or program initiating therapy rather than on the patient. It is well established that appropriate treatment of tuberculosis rapidly renders the patient noninfectious, prevents drug resistance, minimizes the risk of disability or death from tuberculosis, and nearly eliminates the possibility of relapse [95]. Provider responsibility is a central concept in treating patients with tuberculosis, no matter what the source of their care.
What is DOT in chemo?
Among these, directly observed therapy (DOT), the practice of observing the patient swallow their antituberculosis medications, has been widely used as the standard of practice in many tuberculosis programs, and deserves special emphasis (see PICO Question 2 and Supplementary Appendix B, Evidence Profile 4). The systematic review conducted to obtain evidence in support of this practice guideline did not find any significant differences between self-administered therapy (SAT) and DOT when assessing several outcomes of interest, including mortality, treatment completion, and relapse. However, DOT was significantly associated with improved treatment success (the sum of patients cured and patients completing treatment) and with increased sputum smear conversion during treatment, as compared to SAT. Because DOT is a multifaceted public health intervention that is not amenable to the conventional clinical trial approaches to assessing benefits, and because participation in DOT can be advantageous for early recognition of adverse drug reactions and treatment irregularities, for allowing providers to establish rapport with the patient and for addressing treatment complications expeditiously, DOT remains the standard of practice in the majority of tuberculosis programs in the United States [33–35] and Europe [15] (Table 5). To be consistent with the principles of patient-centered care noted previously, decisions regarding the use of DOT must be made in concert with the patient [14–16]. For example, DOT can be provided in the office, clinic, or in the “field” (patient's home, place of employment, school, or any other site that is mutually agreeable) by appropriately trained personnel [32].
What is the ATS guideline?
The American Thoracic Society (ATS), Centers for Disease Control and Prevention (CDC), and Infectious Diseases Society of America (IDSA) jointly sponsored the development of this guideline on the treatment of drug-susceptible tuberculosis, which is also endorsed by the European Respiratory Society (ERS) and the US National Tuberculosis Controllers Association (NTCA). This guideline provides recommendations on the clinical and public health management of tuberculosis in children and adults in settings in which mycobacterial cultures, molecular and phenotypic drug susceptibility tests, and radiographic studies, among other diagnostic tools, are available on a routine basis. Nine PICO (population, intervention, comparators, outcomes) questions and associated recommendations, developed based on the evidence that was appraised using GRADE (Grading of Recommendations Assessment, Development, and Evaluation) methodology [1, 2], are summarized below. A carefully selected panel of experts, screened for conflicts of interest, including specialists in pulmonary medicine, infectious diseases, pharmacokinetics, pediatrics, primary care, public health, and systematic review methodology were assembled and used GRADE methods to assess the certainty in the evidence (also known as the quality of evidence) and strength of the recommendations (see Supplementary Appendix A: Methods and Table 1). This executive summary is a condensed version of the panel's recommendations. Additional detailed discussion of the management of pulmonary and extrapulmonary tuberculosis is available in the full-text version of this guideline.
What is the role of public health in treating tuberculosis?
Because of the public health implications of prompt diagnosis and effective treatment of tuberculosis, most low-incidence countries designate a government public health agency as legal authority for controlling tuberculosis [12, 13]. The optimal organization of tuberculosis treatment often requires the coordination of public and private sectors [14–16]. In most settings, a patient is assigned a public health case manager who assesses needs and barriers that may interfere with treatment adherence [17]. With active input from the patient and healthcare providers, the case manager, together with the patient, develops an individualized “case management plan” with interventions to address the identified needs and barriers [18–20] (see PICO Question 1 and Supplementary Appendix B, Evidence Profiles 1–3). The least restrictive public health interventions that are effective are used to achieve adherence, thereby balancing the rights of the patient and public safety. Given that tuberculosis treatment requires multiple drugs be given for several months, it is crucial that the patient be involved in a meaningful way in making decisions concerning treatment supervision and overall care. International standards have been developed that also emphasize the importance of using patient-centered approaches to the management of tuberculosis [14–16].
What is the decision to initiate combination chemotherapy for tuberculosis?
The decision to initiate combination chemotherapy for tuberculosis is based on clinical, radiographic, laboratory, patient, and public health factors (Figure 1). In addition, clinical judgment and the index of suspicion for tuberculosis are critical in making a decision to initiate treatment.
Is co-trimoxazole used for HIV?
Whereas the WHO recommends routine co-trimoxazole prophylaxis for all HIV-infected people with active tuberculosis disease regardless of the CD4 cell count [66], in high-income countries, co-trimoxazole prophylaxis is primarily used in tuberculosis patients coinfected with HIV with CD4 counts <200 cells/µL [67].

Documentation of Overseas TB Evaluation
Domestic Refugee Screening For Tuberculosis
- All refugees, including those classified with a TB condition overseas, should receive a comprehensive domestic medical screening within 90 days of arrival. The goal of the domestic screening for TB is to find persons with LTBI, in order to facilitate prompt treatment and control, and to find persons who may have developed TB disease since the overseas medical examinati…
Overview of Treatment
- A complete discussion of treatment for TB disease and LTBI is beyond this scope of this guidance document. CDC treatment guidelines call for clinicians to not only prescribe an appropriate regimen (length of course of treatment and treatment regimen), but also ensure adherence to the regimen until treatment is completed. TB disease should be diagnosed and treated in consultati…