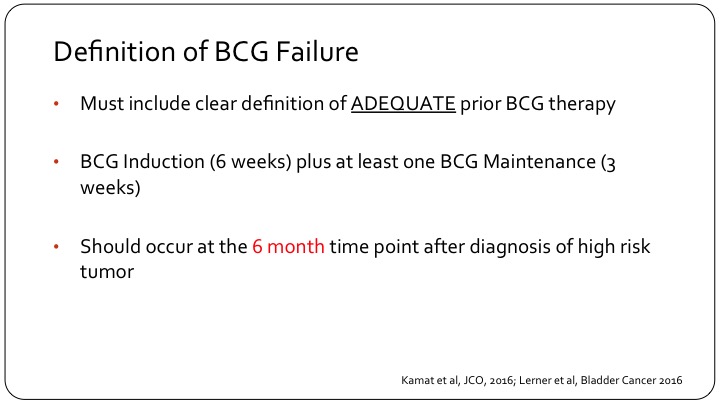
Bacillus Calmette-Guerin (BCG) treatment is a type of intravesical (in your bladder) immunotherapy. This liquid drug is made from a strain of Mycobacterium bovis — the same bacterium used to create the tuberculosis vaccine. When used in medicine, Mycobacterium bovis is weakened to reduce harm to your body.
Full Answer
What's new in BCR prostate cancer research?
androgen deprivation therapy, either through chemical castration or, far more rarely, through orchiectomy, is one reasonable standard of care for bcr prostate cancer after maximal local therapy. 24 gonadotrophin-releasing hormone (gnrh) agonists, including leuprolide and goserelin, have been the primary medical castration therapies in the western …
What is the prognosis of basal cell carcinoma (BCR)?
BCR/ABL1-like acute lymphoblastic leukemia (ALL) accounts for 15% to 30% of B-lineage ALL, with a peak of incidence occurring in adolescence. This subgroup of patients is characterized by a peculiar transcriptional profile that resembles that of true BCR/ABL1-positive cases, and have a heterogeneous genetic background and a poor outcome.
What are the main features of BCR/ABL1?
Feb 11, 2019 · Hello fellow travelers in the post surgery/post radiation journey in prostate ca treatment: After RARP in 2018 with bcr in 2020 i underwent 6 months ADT/+ Pelvic Radiation for pT3a with gleason 3+4 , primary pattern 3 12 months later 2022 i have bcr again with psa 0.4 Now a psma pet CT shows possible L common iliac node involvement at 3 mm So ...
Is there a standardized diagnostic and therapeutic approach for BCR/ABL1?
Apr 11, 2022 · BCR technologies are available across North America. We are transforming biosolids and organic waste management using our patented treatment solutions: Each treatment solution produces a safe, odor-reduced, nutrient-rich end product while minimizing the cost and risks associated with biosolids and organics process management. YouTube.
How is BCR test done?
A BCR-ABL test is usually a blood test or a procedure called a bone marrow aspiration and biopsy. If you are getting a blood test, a health care professional will take a blood sample from a vein in your arm, using a small needle.Sep 14, 2021
How long does BCR-ABL take?
BCR-ABL1 testing requires specialized equipment and expertise and your sample may be sent to a specialized hospital laboratory or a reference laboratory. It may take one to several days for your results to be available.Nov 6, 2020
What is BCR treatment?
Options for treatment of BCR after RP are RT at least to the prostatic bed, complete or intermittent ADT, or observation; for BCR after RT, salvage RP, cryotherapy, complete or intermittent ADT, brachytherapy, high-intensity focused ultrasound (HIFU), or observation can be considered.Nov 21, 2017
What foods should I avoid with chronic myeloid leukemia?
When following a neutropenic diet, you generally must avoid:all uncooked vegetables.most uncooked fruits, except those with a thick peel like banana or citrus fruits.raw or rare meat.uncooked fish.uncooked or undercooked eggs.most foods from salad bars and deli counters.More items...
What is the difference between AML and CML?
AML and CML are blood and bone marrow cancers that affect the same lines of white blood cells. AML comes on suddenly as very immature cells crowd out normal cells in the bone marrow. CML comes on more slowly, with the CML cells growing out of control.Sep 12, 2021
What does a CBC look like with CML?
CBC results that point to CML may include: high white blood cell count. too many blasts. low red blood cell count.Sep 9, 2021
What happens if PSA comes back?
Treatment options after recurrence. PSA levels are usually extremely low (below the normal range) about a month after surgery. You may hear your doctor saying that your PSA level is undetectable (< 0.01 ng/ml). If your PSA level starts to rise, this might mean the cancer has come back.Jun 17, 2019
What are the side effects of tyrosine kinase inhibitors?
Side Effects of Tyrosine Kinase Inhibitor (TKI) TherapyNausea, vomiting and diarrhea.Muscle cramps and bone pain.Fatigue.Rashes.
What should PSA level be after brachytherapy?
Recent studies have shown that for optimal results, PSA levels should be lower than 1 ng/ml, and even lower than 0.5 ng/ml. Levels that are above 1 or 2 ng/ml 12 to 18 months following completion of radiation treatments are very worrisome, because they indicate that the cancer may not have been eradicated.Mar 31, 2009
Is exercise good for CLL?
CLL and its treatments can leave you so tired that it's hard to even think about exercising. Yet staying active actually helps reduce fatigue. It can also help improve cancer symptoms. No single exercise program is best for CLL.Apr 9, 2019
Which fruit is best for leukemia?
The LLS recommends a diet for people who have leukemia should include: a variety of vegetables and legumes, which should make up around 50% of most meals. whole fruits, such as apples or blueberries.Oct 28, 2021
Can you live a normal life with chronic myeloid leukemia?
While patients with CML are fortunate to have excellent therapies available to control their disease, most do not lead normal lives due to the diminished health-related quality of life that is associated with long term treatment.
What is the most frequent copy number aberration in BCR/ABL1?
The most frequent copy number aberration in BCR/ABL1– like ALL is IKZF1 deletion, which is documented in approximately 27% of pediatric cases and in approximately 70% of high-risk pediatric patients with ALL. 16 IKZF1 deletions initially were recognized as a negative prognostic marker both in patients with BCR/ABL1 –positive and those with BCR/ABL1 -negative ALL. 7, 45 - 49
What is the most common cancer in children?
Acute lymphoblastic leukemia (ALL) is the most frequent cancer diagnosed in children. Although it decreases in adolescence and adulthood, a second peak can be recorded starting from the sixth decade of life onward. 1 The outcome of patients with ALL has improved in the last decades, particularly in children, for whom the intensification of treatment, patient stratification based on clinical risk factors, and minimal residual disease (MRD) monitoring have led to cure rates approaching 80% to 90%. 2 When applying the above mentioned principles to adolescents and young adults, the 5-year survival rates are reported to be approximately 50% to 60%. In adults and the elderly, the scenario still is disappointing because of the presence of poor-prognosis genetic subgroups and comorbidities, which hamper the possibility of the patient receiving high-dose chemotherapy and undergoing allogeneic transplantation procedures. 3
What is BCR/ABL1 like ALL?
Patients with BCR/ABL1 –like ALL often are of male sex, are mainly young adults, and are characterized by hyperleukocytosis at the time of onset of the disease. As already mentioned, in addition to the peculiar transcriptional profile, the interest in this subset of patients also derives from the worse outcome noted among pediatric patients with BCR/ABL1 –like ALL due to an inferior response to induction therapy, a higher incidence of relapse, and lower survival compared with the remaining B-cell ALL BCR/ABL1 –negative cases. 6, 7 Furthermore, in a multivariate analysis, the BCR/ABL– like ALL subtype represented an independent risk factor. 6 Subsequently, Roberts et al 26 studied a broad cohort of pediatric patients with ALL who were enrolled in MRD-driven protocols and highlighted that pediatric patients with BCR/ABL1 –like ALL, although demonstrating higher MRD levels at the end of induction, had a survival similar to that of patients with non– BCR/ABL1 -like ALL when treated with intensive therapies that included transplantation procedures. In contrast, Heatley et al, 20 who analyzed patients enrolled in the Australian and New Zealand Children’s Haematology/Oncology Group (ANZCHOG) ALL8 clinical trial, which was based on MRD evaluation for risk stratification, demonstrated that despite a risk-adjusted treatment approach, a high rate of disease recurrence was recorded among children who were retrospectively identified as having Ph–like ALL.
Should patients with BCR/ABL1 be treated differently?
As mentioned, it is not clear whether individuals with BCR/ABL1– like ALL (if adequately identified, which still remains a challenge) should be treated differently upfront or, instead, if a treatment switch (or intensification with allogeneic stem cell transplantation and targeted approaches) should be limited to those patients who are positive for MRD. In addition, although there is a general consensus that patients should receive a TKI, to the best of our knowledge the best TKI has not been defined to date because of the plethora of genetic lesions. Two alternative approaches have been proposed. The first is based on the underlying lesion, considering dasatinib for patients with ABL class genes and JAK2 inhibitors, particularly ruxolitinib, for those with JAK/STAT pathway lesions. However, this approach is not applicable to all hematologic centers; furthermore, the preliminary results from The University of Texas MD Anderson Cancer Center in Houston regarding 9 patients with recurrent/refractory BCR/ABL 1-like ALL have not shown significant responses. 22 Another approach could be the use of ponatinib, as suggested by our group and tested in a patient by Collette et al. 12, 52 Third, the role of immunotherapy, namely blinatumomab and inotuzumab as well as chimeric antigen receptor (CAR) T cells, remains to be determined conclusively.
Can BCR block ABL1?
The poor outcome of patients with BCR/ABL1– like ALL and the identification of actionable lesions has opened the way to the treatment of patients with genetic-driven approaches because the majority of lesions converge on a limited number of pathways. Indeed, it is possible to block the aberrant fusion protein as ABL class lesions or JAK alterations, or to interfere with the aberrantly activated downstream pathways because cytokine receptor and JAK alterations result in the phosphorylation of molecules of the JAK/STAT, phosphatidylinositide 3-kinase (PI3K)/mammalian target of rapamycin (mTOR), and/or MEK/ERK pathways (Fig. 4 ). 44
The Early-Stage Bladder Cancer Treatment
Jennifer Welsh is a Connecticut-based science writer and editor with over ten years of experience under her belt. She’s previously worked and written for WIRED Science, The Scientist, Discover Magazine, LiveScience, and Business Insider.
Who Can Use BCG?
BCG is a treatment for early-stage bladder cancer that has not yet invaded the muscle of the bladder wall. Called non-muscle invasive bladder cancers (NMIBCs) or in situ bladder cancers, these account for about half of all bladder cancers. 3
What to Expect During BCG Treatment
First, make sure you haven’t had any fluids for four hours before the treatment. Right before you go into the treatment room your doctor or nurse will have you empty your bladder. 2
How to Prepare
To prepare for the BCG treatment, your doctor will likely have you undergo surgery to remove any visible cancer in the bladder. The surgery is called transurethral resection of bladder tumor (TURBT) and is usually done about two weeks before BCG therapy.
When to See a Doctor
There are a few side effects that can be especially dangerous, so make sure to talk to your doctor if you notice that you: 2
Other Treatments for Bladder Cancer
For many early-stage bladder cancers, BCG is the best option for treatment. Other treatments for bladder cancer include:
Summary
BCG treatment is a form of immunotherapy for non-muscle invasive bladder cancer. It is administered into the bladder through a catheter. It then activates the body's immune system to attack the cancer cells.
How does a BCG catheter work?
A urinary catheter is inserted through your urethra and into your bladder. Then the BCG solution is injected into the catheter. The catheter is clamped off so the solution stays in your bladder. Some doctors may remove the catheter at this time. You have to hold the medicine in your bladder.
How long does it take for a bladder catheter to unclamp?
You’ll be instructed to lie on your back and to roll from side to side to make sure the solution reaches your entire bladder. After about two hours, the catheter is unclamped so the fluid can be drained. If the catheter was already removed, you’ll be asked to empty your bladder at this time.
What is the procedure called to remove bladder cancer?
It usually follows a procedure called transurethral resection of bladder tumor (TURBT). It’s intended to help prevent recurrence. This treatment only affects cells inside the bladder. It’s not useful for later stage bladder cancer that has spread into or beyond the bladder lining, or to other tissues and organs.
How to get rid of BCG in men?
Disinfect the urine by adding 2 cups of bleach into the toilet. Let it stand for about 20 minutes before flushing. You should also wash your genital area very carefully after you urinate, so your skin doesn’t become irritated from the BCG. Wash your hands thoroughly, too. Men can pass BCG to their partner during sex.
How long after BCG treatment can you have sex?
Men can pass BCG to their partner during sex. For that reason, you should avoid sex for 48 hours after each treatment. Use a condom between treatments and for six weeks following your final treatment. Women should avoid getting pregnant or breastfeeding while on BCG therapy.
What to do before BCG?
Tell your doctor about all the medications you take. Certain immunosuppressants, antimicrobial therapies, and radiation therapies can interfere with BCG treatment. You’ll be advised to limit your fluid intake for four hours prior to ...
Can you have more than one cancer treatment?
how well you tolerate certain treatments. Cancer treatment usually involves more than one type of therapy, which can be given at the same time or one at a time. That makes it difficult to compare one treatment to another.
What is a Ph-like all?
Philadelphia chromosome (Ph)-like acute lymphoblastic leukemia (ALL), also referred to as BCR - ABL1 –like ALL, is a high-risk subset with a gene expression profile that shares significant overlap with that of Ph-positive (Ph +) ALL and is suggestive of activated kinase signaling. Although Ph + ALL is defined by BCR - ABL1 fusion, Ph-like ALL cases contain a variety of genomic alterations that activate kinase and cytokine receptor signaling. These alterations can be grouped into major subclasses that include ABL-class fusions involving ABL1, ABL2, CSF1R, and PDGFRB that phenocopy BCR-ABL1 and alterations of CRLF2, JAK2, and EPOR that activate JAK/STAT signaling. Additional genomic alterations in Ph-like ALL activate other kinases, including BLNK, DGKH, FGFR1, IL2RB, LYN, NTRK3, PDGFRA, PTK2B, TYK2, and the RAS signaling pathway. Recent studies have helped to define the genomic landscape of Ph-like ALL and how it varies across the age spectrum, associated clinical features and outcomes, and genetic risk factors. Preclinical studies and anecdotal reports show that targeted inhibitors of relevant signaling pathways are active in specific Ph-like ALL subsets, and precision medicine trials have been initiated for this high-risk ALL subset.
What are Sentinel genetic aberrations?
Sentinel genetic aberrations define Ph-like ALL genomic subsets ( Figure 1 ), 34, 51 with their relative frequency differing based on patient characteristics, including age and ethnicity, and the method used to define Ph-like ALL.
What is ALL genetics?
Acute lymphoblastic leukemia (ALL) is a constellation of genetic diseases driven by sentinel genetic alterations commonly derived from structural chromosome rearrangements, aneuploidy, and cooperative mutations in genes that encode for transcription factors regulating lymphoid development, tumor suppressors, proteins that regulate cell cycle progression, and epigenetic modifiers. 1 Subtypes of ALL can be defined based on the nature of specific sentinel genetic aberrations, particularly chromosome translocations and interstitial rearrangements that create fusion genes encoding chimeric proteins or hijack gene promoters causing dysregulated oncogene expression. 2
What is the Philadelphia chromosome?
Philadelphia chromosome (Ph)-like acute lymphoblastic leukemia (ALL), also referred to as BCR-ABL1–like ALL, is a high-risk subset with a gene expression profile that shares significant overlap with that of Ph-positive ( Ph+) ALL and is suggestive of activated kinase signaling . Although Ph+ALL is defined by BCR-ABL1fusion, ...
Is Ph-like all a therapeutic target?
Although the Ph-like gene expression signature is useful diagnostically, it is not a therapeutic target. The prognostic significance and potential for therapeutic targeting of the IKZF1 deletion remains unclear given its association to date with both unfavorable (Ph +, Ph-like) 9, 10, 23, 28, 31, 48, 58, 82-84 and favorable ( DUX4 / ERG -dysregulated) 85-87 B-ALL subtypes. ALL-associated IKZF1 alterations have been linked with upregulation of multiple genes involved in cellular proliferation and chemoresistance. 88 One study found that IKZF1 -deleted ALL patients benefited from periodic vincristine/steroid pulses during maintenance therapy, 83 prompting the Dutch Childhood Oncology Group to extend maintenance therapy and to include vincristine and steroid pulses for patients with IKZF1 deletions (www.trialregister.nl; NTR3379). The benefit of maintenance vincristine/steroid pulses for patients with IKZF1 -deleted ALL was not confirmed by other groups. 89 Furthermore, the COG uses many more maintenance vincristine/steroid pulses than other groups and still finds IKZF1 deletion to be an adverse prognostic factor. Preclinical studies have demonstrated the therapeutic potential of retinoic acid compounds and FAK inhibitors in IKZF1 -deleted ALL models, but these approaches have not yet been tested clinically. 90, 91 Deletions involving other B-lymphoid transcription factor genes, such as EBF1 and PAX5, are also recurrent alterations in Ph-like ALL, but strategies to target these lesions therapeutically have not yet been developed. The greatest opportunity for precision medicine approaches in Ph-like ALL is to use therapies targeted at the underlying sentinel molecular lesions, many of which are likely to be drivers of leukemogenesis. Different diagnostic approaches to identify these lesions have been used. As more cases are analyzed, more fusion partners and splice variants of known fusions have been identified for the ABL-class, JAK2, and rarer kinase genes ( Table 1 ), emphasizing the need to use unbiased sequencing technologies, such as RNAseq. 34, 51, 52 Analysis that relies only on RT-PCR for known fusions will invariably miss some, and perhaps many, targetable alterations.
Is PAX5 isolated in Ph-like all cases?
34 Isolated mutations in the Ras pathway also occur in a small number of Ph-like ALL cases, but have been reported in conjunction with CRLF2 overexpression with and without JAK alterations. 34, 50
What type of doctor is responsible for radiation therapy?
Radiation oncologist. This type of doctor specializes in giving radiation therapy to treat cancer. A radiation oncologist oversees radiation therapy treatments. They work closely with other team members to develop the treatment plan. Radiation oncology nurse.
What is simulation in radiation therapy?
Simulating and planning treatment. Your first radiation therapy session is a simulation. This means it is a practice run without giving radiation therapy. Your team will use imaging scans to identify the tumor location.
How long does radiation therapy last?
It is the most common radiation therapy treatment for cancer. Each session is quick, lasting about 15 minutes. Radiation does not hurt, sting, or burn when it enters the body.
Why is it important to be in the same position for radiation?
It is important for your body to be in the same position for each treatment. Your radiation oncology team cares about your comfort. Talk with the team to find a comfortable position that you can be in every time you come in for radiation therapy.
How often should you check for radiation?
During your treatment, your radiation oncologist will check how well it is working. Typically, this will happen at least once a week. If needed, they may adjust your treatment plan.
What is informed consent for radiation?
Giving permission for radiation therapy. If you choose to receive radiation therapy, your health care team will ask you to sign an "informed consent" form. Signing the document means: Your team gave you information about your treatment options. You choose to have radiation therapy.
How long does it take for radiation to go away?
The 2-day break in treatment each week allows your body some time to repair this damage. Some of the effects may not go away until the treatment period is completed. Let the health care professionals if you are experiencing side effects. Read more about the side effects of radiation therapy.