
Discussion
- Antiresorptive treatment. Various studies point out that the antiresorptive treatment not only increases bone mineral density in the hip and decreases bone remodelling, but could also protect of osteoporotic fractures ...
- Treatment that acts on the CNS. ...
- Living institutionalised. ...
- Limitations. ...
What is the meaning of antiresorptive?
: slowing or blocking the resorption of bone Since postmenopausal osteoporosis is characterized by bone resorption that exceeds bone formation, antiresorptive agents can help to restore skeletal balance by reducing bone turnover, primarily at the tissue level. — Ernesto Canalis et al. What does 'poke' refer to in the expression 'pig in a poke'?
What is antiresorptive therapy for osteoporosis?
: slowing or blocking the resorption of bone Since postmenopausal osteoporosis is characterized by bone resorption that exceeds bone formation, antiresorptive agents can help to restore skeletal balance by reducing bone turnover, primarily at the tissue level. — Ernesto Canalis et al.
How many prescribers supply antiresorptives during the first 12 months of treatment?
During the first 12 months of antiresorptive therapy, the majority of the patients received their prescriptions from one or two prescribers (71% and 24%, respectively). Were enough antiresorptives supplied during the first 12 months of treatment?
What was the first prescribed antiresorptive in 2007?
Combination bisphosphonates overtook single formulation of bisphosphonate as the first-prescribed antiresorptive in the year between July 2006 and June 2007. Who prescribed antiresorptive drugs?
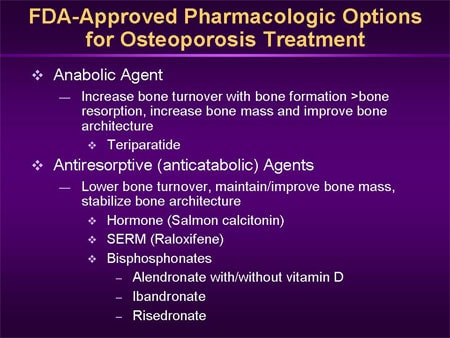
What does antiresorptive therapy mean?
Antiresorptive agents are bone preserving medications which can slow down the bone loss associated with osteoporosis (O'Neil et al. 2004). These reduce bone loss by inhibiting bone degeneration activity and/or promoting bone formation.
How do antiresorptive drugs work?
Antiresorptive drugs work by slowing the resorption or breakdown part of the remodeling cycle. Anabolics work by stimulating the formation part of the remodeling process. More bone is formed than is taken away. The result is stronger bone that is less likely to break.
What is the most effective osteoporosis treatment?
Bisphosphonates are usually the first choice for osteoporosis treatment. These include: Alendronate (Fosamax), a weekly pill. Risedronate (Actonel), a weekly or monthly pill.
Is estrogen an antiresorptive?
Antiresorptive agents such as estrogens, SERMs (in postmenopausal women) and calcitonin are considered to be second-line agents that are appropriate in special circumstances.
What is the newest treatment for osteoporosis?
Romosozumab (Evenity). This is the newest bone-building medication to treat osteoporosis. It is given as an injection every month at your doctor's office and is limited to one year of treatment.
What are the long term side effects of alendronate?
Serious side effects and their symptoms can include the following:Ulcers or erosions of your esophagus. Symptoms can include: ... Bone death of your jaw. Symptoms can include: ... Unusual bone breaks in your hip and leg bones. ... Hypocalcemia (low calcium levels in your blood). ... Severe bone, joint, or muscle pain.
What is the safest osteoporosis drug 2020?
The U.S. Food and Drug Administration today approved Evenity (romosozumab-aqqg) to treat osteoporosis in postmenopausal women at high risk of breaking a bone (fracture).
What foods to avoid if you have osteoporosis?
7 Foods to Avoid When You Have OsteoporosisSalt. ... Caffeine. ... Soda. ... Red Meat. ... Alcohol. ... Wheat Bran. ... Liver and Fish Liver Oil.
What is the life expectancy of a person with osteoporosis?
This excess risk is more pronounced in the first few years on treatment. The average life expectancy of osteoporosis patients is in excess of 15 years in women younger than 75 years and in men younger than 60 years, highlighting the importance of developing tools for long-term management.
What is the most commonly prescribed drug for osteoporosis?
Bisphosphonates: Most Commonly Prescribed For OsteoporosisAlendronate (Fosamax, Binosto): may be taken orally daily or a weekly tablet is also available.Ibandronate (Boniva): can be taken orally monthly or given by intravenous injection every three months.More items...•
What are the side effects of bisphosphonates?
General side effects of bisphosphonates and denosumabFever and flu-like symptoms. ... Low levels of calcium in your blood (hypocalcaemia) ... Bone and joint pain. ... Changes in bowel movements. ... Tiredness and low energy levels. ... Feeling sick. ... Changes to your kidneys. ... Irritation of the food pipe (oesophagus)More items...•
Can estrogen reverse osteoporosis?
Estrogen replacement therapy used to be the only FDA-approved treatment to prevent osteoporosis. There are now many other drugs and medications for osteoporosis, but estrogen remains a fairly common treatment to conserve bone mass and prevent osteoporosis-related fractures in post-menopausal women.
What are the antiresorptive agents used for?
Antiresorptive therapies are used to increase bone strength in individuals with osteoporosis and include five principal classes of agents: bisphosphonates, estrogens, selective estrogen receptor modulators (SERMs), calcitonin and monoclonal antibodies such as denosumab. However, no head-to-head studies have compared different antiresorptive agents ...
Who is likely to derive clear benefits from a particular antiresorptive therapy according to an assessment of?
Men and women who are likely to derive clear benefits from a particular antiresorptive therapy according to an assessment of the individual patient's circumstances
What are the benefits of bisphosphonates?
Bisphosphonates reduce the risk of vertebral fractures in postmenopausal women. 30 In addition, nitrogen-containing bisphosphonates, such as alendronate, risedronate and zoledronate, reduce the risk of hip fracture and nonvertebral fractures ( Table 1 ). 14, 17, 18.
What is the best treatment for osteoporosis?
Several antiresorptive agents can safely reduce fracture risk in various high-risk populations. Bisphosphonates or denosumab should be recommended as first-line therapy for patients with osteoporosis. Selective estrogen receptor modulators (SERMs) are currently not used as first-line therapy except, occasionally, ...
How do bisphosphonates help with osteoporosis?
Bisphosphonates suppress bone resorption by binding to bone at sites of active remodeling and blocking osteoclast activity. 29 These agents have made a major contribution to the management of patients with osteoporosis and are currently the most widely used antiresorptive therapies. Bisphosphonates reduce the risk of vertebral fractures in postmenopausal women. 30 In addition, nitrogen-containing bisphosphonates, such as alendronate, risedronate and zoledronate, reduce the risk of hip fracture and nonvertebral fractures ( Table 1 ). 14, 17, 18
Which estrogen receptor modulator is most commonly used for osteoporosis?
SERMs inhibit bone resorption through the same mechanism as do estrogens. Raloxifene is the most widely used SERM in osteoporosis treatment.
Does antiresorptive therapy increase BMD?
Antiresorptive therapies suppress bone turnover and also increase BMD; 26, 27 however, the increase in BMD generally accounts for only a modest portion of the antifracture efficacy. 28 For this reason, fracture is the most important clinical end point in efficacy trials of these therapies. Most studies of antiresorptive therapies have, therefore, been carried out in postmenopausal women, who have a high prevalence of osteoporosis and an increased risk of fractures. The Cochrane Collaboration has reviewed the antifracture efficacy of various individual antiresorptive agents in postmenopausal women ( Table 1 ); however, these data do not enable any conclusions to be drawn with regard to which agents are most effective, since no head-to-head studies have compared different antiresorptive agents using fracture as an end point.
What is the difference between anabolic and antiresorptive drugs?
Most are antiresorptive drugs that slow down the activity of cells that break down old bone, while anabolic drugs stimulate cells that build new bone.
Is teriparatide more expensive than antiresorptive?
While effective, teriparatide is significantly more expensive than antiresorptive osteoporosis drugs, partially because there hasn't been competition, the review authors noted--until now.
Can denosumab prevent vertebral fractures?
Although there is actually no study showing that such a strategy would prevent the risk of vertebral fractures, several authors and medical societies advocate, at denosumab discontinuation, for a period of treatment with a bisphosphonate or another antiresorptive agent (estrogens or SERMs) to preserve BMD gain and avoid the risk of vertebral fracture [7, 11, 12].
Is denosumab an antiresorptive agent?
There have been reports of AFF with denosumab which is another antiresorptive agent (8,9).
How to prevent ONJ in patients?
Many studies have proposed practical guidelines for dental care for preventing ONJ in patients taking ARDs [3,5,21,35,49]. Generally, it is important to educate patients on the importance of maintaining oral hygiene. Furthermore, the causes of infection such as caries, dental plaque, periodontitis, and apical periodontitis need to be treated with conservative procedures. Lastly, if possible, invasive dental procedures should be avoided. To provide proper dental care, dentists need to evaluate the medical history specifically and assess the risk of ARONJ during an examination. The dentist should confirm whether ARD treatment is scheduled or has already started. If treatment has started, the dose of BPs or Dmab the patient is receiving, the treatment duration, and whether any other medication likely to increase the risk of ARONJ is being used should be determined. Based on this information, patients can be categorized as being at low or high risk for developing ARONJ (Table 2) [23]. Patients who have received a low dose of an ARD for less than 4 years with no additional risk factors are regarded to have low risk. Otherwise, all other patients taking an ARD are considered to be at high risk [3,50,51,52].
Does osteonecrosis of the jaw respond to treatment?
Osteonecrosis of the jaw (ONJ) does not respond well to treatment once it has occurred. Therefore, the focus has been on the prevention of ONJ, i.e., avoiding surgical procedures. When the advanced lesion is found, the patient is usually referred to the oral surgeon. However, all dentists could play an important role in the detection of intraoral changes in patients using ARD, thus, helping in preventing complications such as ONJ. When dentists do not have clear guidelines on managing patients using ARD, they might hesitate to provide dental care, or even miss providing necessary treatment. Therefore, this review summarizes our current understanding of ARD-related ONJ based on a literature search. It also suggests guidelines to general dentists when providing dental care to patients using ARD.
What is the FDA approved medication for osteoporosis?
What are the FDA-approved medications for osteoporosis? Antiresorptive medication prevents bone loss, may increase bone density, and lowers the risk of broken bones. Anabolic medication builds new bone, increases bone density, and lowers the risk of broken bones. Antiresorptive medications include a class of drugs called bisphosphonates.
How do osteoporosis medications get FDA approval?
The efectiveness and safety of the medication is rigorously tested before it is approved by the Food and Drug Administration (FDA). FDA approval means the medication has been proven to:
How do you take your osteoporosis medication?
The medication will say how it should be taken and how often. Medications come in pill form, an injection, or are given intravenously (in the vein).
Can you take medication for osteoporosis?
If you have been told you have osteoporosis, lifestyle changes may not be enough. Medication may be needed to stop bone loss and to prevent broken bones. Talk to your health care provider and review your medical history and risk factors about whether you need medication. You can discuss the benefits and potential risks of a medication. While on medication, it's still important to:
