What is a vesicant in an infusion?
These two terms defined by the Infusion Nurses Society means: Vesicant – an agent capable of causing blistering, tissue sloughing or necrosis when it escapes from the intended vascular pathway into surrounding tissue.
Are chemotherapeutic agents vesicants?
Some chemotherapeutic agents, such as the vinca alkaloids and the anthracyclines, are universally accepted as vesicants with well-described physicochemical properties and supportive literature detailing the consequences of extravasation.
What is extravasation of a vesicant?
Introduction Extravasation of a vesicant is a potentially disfiguring event associated with many commonly used intravenous antineoplastics. There are numerous reports of paclitaxel causing tissue damage including blistering following extravasation [Stanford and Hardwicke, 2003].
What should I look for when administering vesicant drugs?
- Even if there is an existing IV route, secure a new route when administering vesicant drugs. - If in doubt, re-insert the cannula and administer the drug. - Watch for edema, inflammation, and pain around the cannula during administration.

What is a vesicant cancer?
(VEH-sih-kunt ek-STRA-vuh-SAY-shun) The leakage of certain drugs called vesicants out of a vein into the tissue around it. Vesicants cause blistering and other tissue injury that may be severe and can lead to tissue necrosis (tissue death).
What is vesicant therapy?
Vesicants are IV solutions and medications that cause ischemia and necrosis. Vesicants are extremely acidic or basic (pH less than 5 or greater than 9), hyperosmolar (extremely concentrated), or vasoconstrictive (cause the blood vessels to constrict). Many chemotherapy drugs are vesicants.
Is chemotherapy a vesicant or irritant?
Extravasation, the inadvertent leakage of vesicant chemotherapy outside of the vein and into surrounding tissue, is a significant risk for patients. It can cause pain, swelling, erythema, tissue damage, blistering, sloughing, tis- sue necrosis, and significant morbidity that may require surgical interven- tion.
How is vesicant chemotherapy administered?
Peripheral vesicants are administered by gravity infusions or i.v. bolus and should not be infused using an infusion pump since the pump may continue to deliver a vesicant into the tissue until the pump alarm is triggered (AIII).
Which chemotherapy drugs are vesicants?
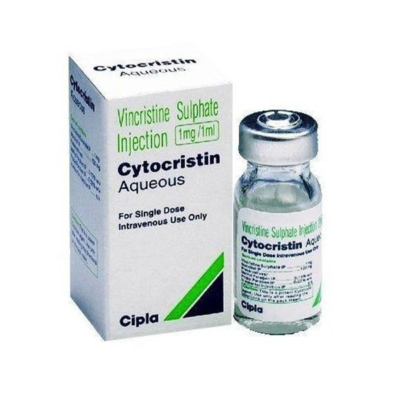
Vesicants: Drugs that can result in tissue necrosis or formation of blisters when accidentally infused into tissue surrounding a vein[14]. They include Actinomycin D, Dactinomycin, Daunorubicin, Doxorubicin, Epirubicin, Idarubicin, Mitomycin C, Vinblastine, Vindesine, Vincristine, and Vinorelbine.
What are known vesicants?
The following chemotherapeutic agents are vesicants: actinomycin-D. daunorubicin. doxorubicin. idarubicin. mechlorethamine.
What do you mean by vesicant?
Definition of vesicant : an agent (such as a chemical weapon) that induces blistering.
What is the difference between vesicants and irritants?
Vesicant: Medication that may causes severe and/or irreversible tissue injury and necrosis. Irritant: Medication that can cause local inflammatory reactions at the infusion site, which may include: burning, swelling, pain, inflammation, tightness, or phlebitis.
Which chemotherapy agent is considered an irritant with vesicant properties?
Drugs that are classified as irritants with vesicant properties include docetaxel, liposomal doxorubicin, melphalan, mitozantrone, oxaliplatin, paclitaxel and nab-paclitaxel.
What is the safest way to administer vesicant therapy?
If there is any doubt, don't use the catheter for vesicant infusions. Prevention is key, as there are no viable or reliable treatments for most vesicant extravasations. The Infusion Nurse Society Standards of Practice mandate that continuous vesicant infusions should be administered through a central venous catheter.
When is a vesicant drug administered?
for adult patients, vesicant drugs should be diluted during administration by injection into a side port of a fast running drip or via a minibag.
Is Herceptin a vesicant?
Anti-cancer drug extravasation assessment tool. Clinical procedure - extravasation management - irritants with vesicant properties general care....Extravasation management table.Drug nameTrastuzumab (Herceptin®)Class/clinical procedureNon-irritant (neutral)Warm or cold compressNot indicatedAntidoteNot indicated84 more columns
Specific Chemical Agents
The following chemicals were chosen to represent the entire class of vesicants. Vesicants include distilled mustard (HD), mustard gas (H), mustard/lewisite, mustard/T, nitrogen mustard, sesqui mustard, and sulfur mustard.
Info for Clinicians
Case Definition: Vesicant (Mustards, Dimethyl Sulfate, and Lewisite) Includes clinical description, lab criteria for diagnosis, & case classification.
What is the difference between vesicant and extravasation?
Vesicant – an agent capable of causing blistering, tissue sloughing or necrosis when it escapes from the intended vascular pathway into surrounding tissue. Extravasation – the inadvertent infiltration of vesicant solution or medication into surrounding tissue.
What non-chemo drugs cause extravasation?
Listed below are a few non-chemo agents: Vancomycin. Nafcillin. Calcium Chloride. Potassium Chloride. Sodium Chloride. Calcium Gluconate. Dobutamine.
What is the role of contrast agents in nursing?
As nurses, it is our responsibility to take preventive measures, monitor, identify signs/symptoms and institute prompt treatment per policy or as ordered. If you administer any of these agents, prevention is key and consider the following: 1.
Is it better to use a small IV catheter or a large IV catheter?
2. Bigger is not better: Use the smallest gauge IV catheter to administer the prescribed therapy. Good flow rates are possible even with a small gauge catheter. Using an IV catheter too large for the vein will obstruct blood flow and might cause thrombosis distal to the IV site. 3.
Can IV vesicant cause blisters?
There are several chemotherapeutic agents with vesicant properties, and when inadvertently infused into the surrounding tissue from an infiltrated IV, these agents may have the potential to cause blisters, severe tissue injury or necrosis, known as extravasation.
Can an IV pump tell if an IV site is infiltrating?
Infusion pumps will not tell you if an IV site in infiltrating. Always aspirate for positive blood return prior to use, but remember, checking for blood return or back flow of blood is good for patency but not a reliable method for assessing infiltration at IV site.
What is the frequency of extravasation of drugs?
Incidence. The frequency of extravasation in adults is reported to be between 0.1% and 6%.
What is local warming therapy?
The use of local warming therapy (dry heat) is based on the theory that it enhances vasodilation, thus enhancing the dispersion of the vesicant agent and decreasing drug accumulation in the local tissue. The use of local warming is recommended for the extravasation of non–DNA-binding vesicants.
What is extravasation in medicine?
Extravasation refers to the leakage of injected drugs from blood vessels causing damage to the surrounding tissues. Common symptoms and signs of extravasation include pain, stinging or burning sensations, and edema around the intravenous (IV) injection site.
Why is IV fluid administration considered a high risk?
Documentation. Because errors associated with IV administration can result in fatal or life-threatening outcomes , administration of IV fluids and medications can be a high-risk, with adverse outcomes potentially leading to malpractice claims. An incident of extravasation must be correctly documented and reported.
What happens if a patient's condition worsens?
Depending on the situation, patients will bear the cost of hospitalization and medical expenses for cosmetic surgeries, and secondary medical problems might occur if the condition worsens. Disease control . Treatment suspension wastes time and other problems can occur due to delayed treatment.
Why does venous shock occur?
Occurs due to contraction of the vessel wall and usually happens as soon as the fluid injection begins. For the most part, blood does not backflow. Discoloration and edema do not occur. Venous shock can occur when injecting very cold medication or when medication is injected at a rapid pace.
What happens if you have a tendon injury?
While the injury is usually minor and resolves spontaneously, some cases result in serious complications, including full-thickness skin loss and muscle and tendon necrosis requiring reconstructive surgery or even amputation, leading to longer hospital stays, increased morbidity, and increased costs. Pain .
Use in Cancer
Daratumumab is approved to be used alone or with other drugs to treat:
More About Daratumumab
Definition from the NCI Drug Dictionary - Detailed scientific definition and other names for this drug.
Clinical Trials Accepting Patients
Find Clinical Trials for Daratumumab - Check for trials from NCI's list of cancer clinical trials now accepting patients.