Treatment Authorization Code The purpose of the treatment authorization code is so the payer can recalculate the hipps code based on actual number of therapy visits in the episode. It is NOT needed when a patient is billed per visit, only when billed per episode.
What does Medicare require prior authorization?
- Blepharoplasty
- Botulinum toxin injections
- Panniculectomy
- Rhinoplasty
- Vein ablation
Does Medicare require prior authorization?
Traditionally, both parts of Original Medicare (Medicare Parts A and B) rarely require pre-approval. Originally, Medicare Part A required no prior authorization whatsoever. Now however, the law has been changed to allow this process for certain limited Durable Medical Equipment items on very rare occasions.
What is the CMS for Medicare?
The CARES Act also:
- Increases flexibility for Medicare to cover telehealth services.
- Authorizes Medicare certification for home health services by physician assistants, nurse practitioners, and certified nurse specialists.
- Increases Medicare payments for COVID-19-related hospital stays and durable medical equipment.
What are Medicare codes?
The Centers for Medicare & Medicaid Services has released Medicare payment codes effective Feb. 11 for administering the monoclonal antibody bebtelovimab, effective against the omicron COVID-19 variant. The Food and Drug Administration last week authorized ...
Why do we need authorization codes?
How long do authorization codes last?
About this website
What are UB-04 codes?
What are UB04 Condition Codes? This form, also known as the UB-04, is a uniform institutional provider bill suitable for use in billing multiple third party payers. Because it serves many payers, a particular payer may not need some data elements.
What is Box 39 on UB04?
Box 39-41; a-d – Value codes and amounts: (Optional) Use these locators to indicate codes and amounts essential to the proper adjudication of the submitted claim. Each form locator contains a three digit field in which to key the indicator code, and a larger free text field in which to designate an applicable amount.
What is PPS code on UB04?
71 Prospective Payment System (PPS) Code Not required This code identifies the DRG based on the grouper software and is required only when the provider is under contract with a health plan using DRG codes.
What is Revenue Code 0023?
Revenue Code 0023 indicates that the billing is for services under the Home Health Prospective Payment System (HHPPS).
What is Box 59 on a ub04?
59. Patient's Relation to Insured Enter the code for the patient's relationship to the insured. 60. Insured's Unique Identifier Enter recipient's nine-digit Medical Assistance ID.
What is Box 81 on ub04?
Billing Tip: Enter code “81” when billing for emergency services, or the claim may be reduced or denied. An Emergency Certification Statement must be attached to the claim or entered in the Remarks field (Box 80).
What is PPS healthcare?
A Prospective Payment System (PPS) is a method of reimbursement in which Medicare payment is made based on a predetermined, fixed amount. The payment amount for a particular service is derived based on the classification system of that service (for example, diagnosis-related groups for inpatient hospital services).
What is PPS in medical terms?
The Palliative Performance Scale (PPS) is a useful tool for measuring the progressive decline of a palliative resident. It has five functional dimen- sions: ambulation, activity level and evidence of disease, self-care, oral in- take, and level of consciousness.
What is Box 17 on a UB?
17. * Patient Status Enter the 2-digit patient status code that best describes the patient's discharge status. 05-Discharged/transferred to another type of institution for inpatient care or referred for outpatient services to another institution.
What is revenue code 510 used for?
Usually the facility bills on the UB and uses the revenue codes to indicate the department in the facility the patient was in. 510 is the outpatient clinic, 450 is the ER and so on. The revenue code is usually accompanied by a CPT code to indicate the level of the service provided.
What is revenue code 0258?
***Revenue code 0258 requires specific HCPCS when billed on all surgical and medical claims. This revenue code is part of the surgical roll-up for surgical claims. Surgical codes should be submitted on the same claim for the same stay.
What is revenue code 581?
Licensed Practical Nurse (LPN) 581. S9124. 1= visit. Physical Therapy.
What Is an Authorization Code in a Bank Transaction? | Sapling
Payment systems efficiently verify the authorization of transactions on a purchase-by-purchase basis. The approach provides merchants a flexible and high-speed method to conclude the sale of products and services while avoiding transaction errors. The bank authorization code is key to this system.
Authorization Code Grant - OAuth 2.0 Simplified
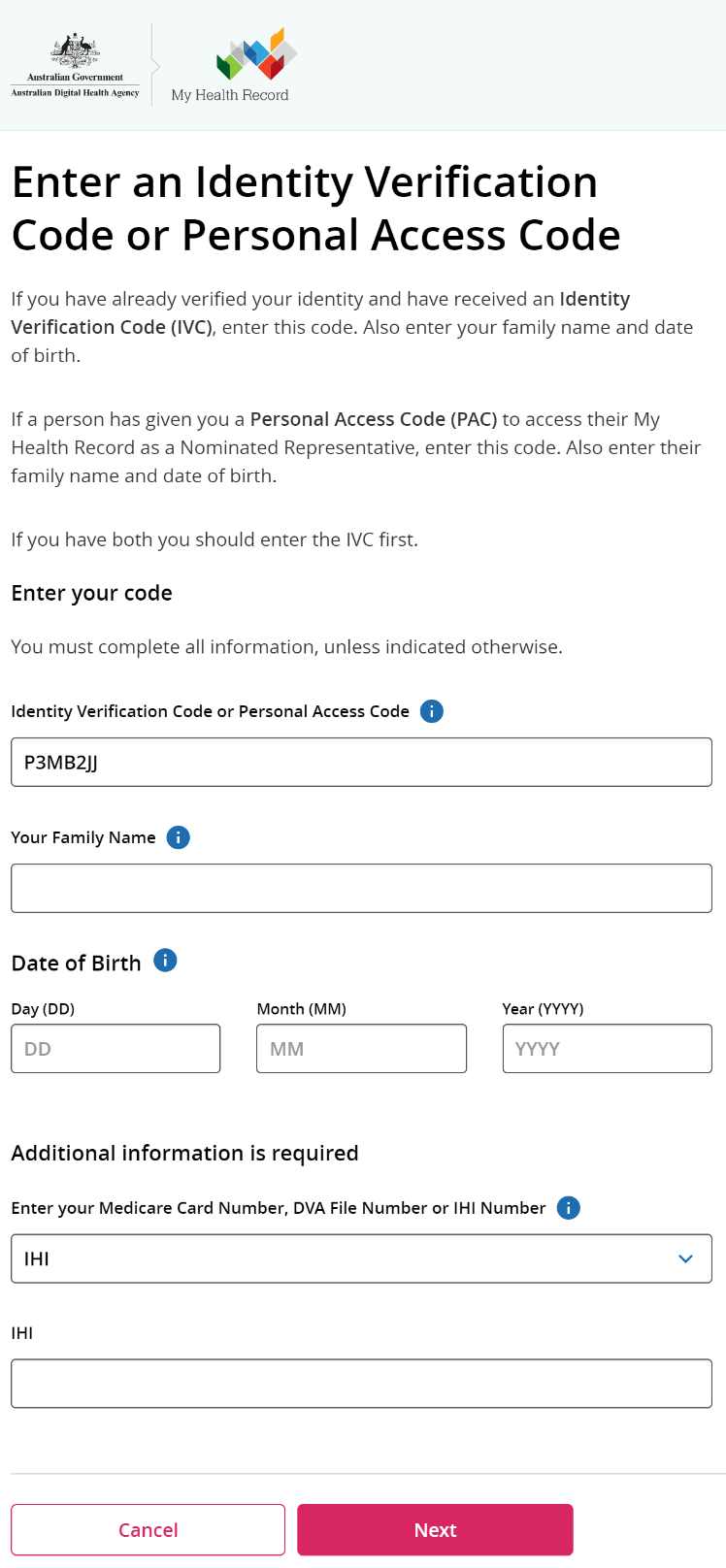
The authorization code is a temporary code that the client will exchange for an access token. The code itself is obtained from the authorization server where the user gets a chance to see what the information the client is requesting, and approve or deny the request.
Why do we need authorization codes?
Authorization codes are transmitted digitally and are used to accelerate credit card processing. If vendors had to call the issuer for a verbal authorization code, in order to complete each and every transaction, it would drastically reduce the speed of commerce.
How long do authorization codes last?
There are also one-time authorization codes or tokens that only last for the length of a single session.
What is authorization code?
The authorization code is a temporary code that the client will exchange for an access token. The code itself is obtained from the authorization server where the user gets a chance to see what the information the client is requesting, and approve or deny the request. The authorization code flow offers a few benefits over the other grant types.
What is redirect_uri?
The redirect_uri may be optional depending on the API, but is highly recommended. This is the URL to which you want the user to be redirected after the authorization is complete. This must match the redirect URL that you have previously registered with the service.
What happens if you allow a request in a service?
If they allow the request, they will be redirected back to the redirect URL specified along with an authorization code in the query string. The app then needs to exchange this authorization code for an access token.
Is OAuth 2.0 a security spec?
OAuth Security. Up until 2019, the OAuth 2.0 spec only recommended using the PKCE extension for mobile and JavaScript apps. The latest OAuth Security BCP now recommends using PKCE also for server-side apps, as it provides some additional benefits there as well.
What is an ICD?
This Interface Control Document (ICD) describes the relationship between the Accountable Care Organizations – Operational System (ACO-OS) and the Fee-for-Service Shared System Maintainers (FFS SSMs), and specifies the interface the requirements participating systems must meet. It describes the concept of operations for the interface, defines the message structure and protocols governing the interchange of data, and identifies the communication paths along which the project team expects data to flow.
What is a CMS waiver?
CMS proposed and finalized, through rulemaking (80 FR 32692), a waiver of the prior 3-day inpatient hospitalization requirement. The waiver is available to Shared Savings Program ACOs who demonstrate the capacity and infrastructure to identify and manage patients who would be either directly admitted to a Medicare Skilled Nursing Facility (SNF) or admitted to a SNF after an inpatient hospital stay of fewer than three days, for services otherwise covered under the Medicare SNF benefit. (Historical note: The waiver originally became available to Track 3 ACOs starting from January 2017 and Track 1+ Model ACOs starting from January 2018.)
What is ACO-OS in CMS?
All the components in the ACO-OS (such as DB2 Servers and Informatica Servers) reside within the CMS environment. Access and authentication to this environment is managed through CMS user credential authentication.
What is an ICD in a project?
This Interface Control Document (ICD) describes and tracks the necessary information required to effectively define the ACO-OS interface. The purpose of this ICD is to give the development teams guidance on the architecture of the systems to be developed, and to clearly communicate all possible inputs and outputs from the ACO-OS for all potential actions. The intended audience is the project manager, project team, development team, and stakeholders interested in interfacing with the ACO-OS.
What is Medicare Administrative Contractor?
The Medicare Administrative Contractor is hereby advised that this constitutes technical direction as defined in your contract. CMS does not construe this as a change to the MAC Statement of Work. The contractor is not obligated to incur costs in excess of the amounts allotted in your contract unless and until specifically authorized by the Contracting Officer. If the contractor considers anything provided, as described above, to be outside the current scope of work, the contractor shall withhold performance on the part(s) in question and immediately notify the Contracting Officer, in writing or by e-mail, and request formal directions regarding continued performance requirements.
Does the revision date apply to red italicized material?
Disclaimer for manual changes only: The revision date and transmittal number apply only to red italicized material. Any other material was previously published and remains unchanged. However, if this revision contains a table of contents, you will receive the new/revised information only, and not the entire table of contents.
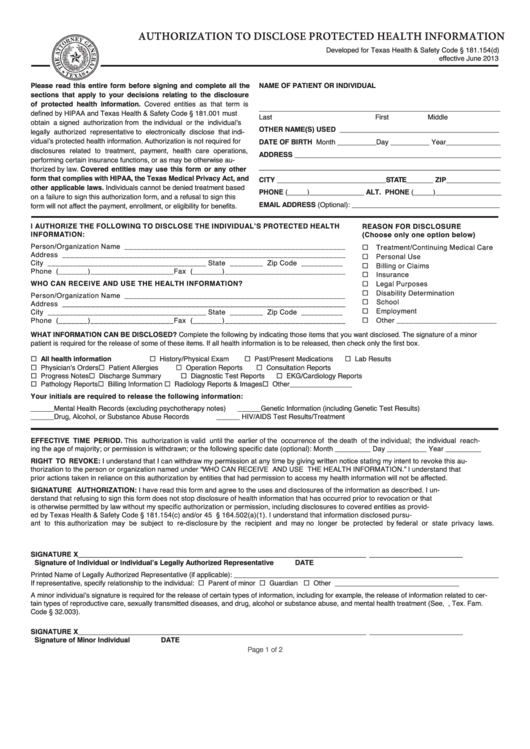
What does authorization mean in medical terms?
Authorization means physician has to obtain permission from insurance company for rendering certain medical services to patient. If authorization has not obtained to treat those healthcare service, then claim will be denied (not paid) from an insurance company.
What is a prior authorization?
Prior authorization also called as Pre authorization. Physician has to obtain permission for certain health care services from the insurance company before rendering those services to patient, in order to get the claim reimbursed.
Why do we need authorization codes?
Authorization codes are transmitted digitally and are used to accelerate credit card processing. If vendors had to call the issuer for a verbal authorization code, in order to complete each and every transaction, it would drastically reduce the speed of commerce.
How long do authorization codes last?
There are also one-time authorization codes or tokens that only last for the length of a single session.
