Radiation boost
- Don't wash the ink marks off your skin.
- Check with your radiation therapy team before putting any lotions or powders on the affected area.
- Wear clothing that’s easy to take off in case you need to change into a hospital gown.
- Use reliable birth control to prevent pregnancy (radiation can harm a fetus).
- Keep the treated area out of the sun.
What does radiation treatment boost mean?
May 08, 2008 · Answer: When we talk about a radiation boost in general, we're talking about some additional radiation to a very small component or part of our initial targeted field or body part that we're treating or tumor.
What to expect during and after radiation treatments?
A radiation boost is one or more extra treatments, given at a higher dose than routine treatments, and targeted at the tumor bed. This extra dose covers a small area and affects the tissue where cancer is most likely to return. Radiation boost treatments are given after the regular sessions of radiation are complete.
What to expect when having radiation therapy?
After radiation therapy to the whole breast, you may have more radiation (called a boost) to the part of the breast that had the tumor. This boost increases the amount of radiation given to the area at highest risk for breast cancer recurrence. Your boost radiation session is similar to a regular session.
Which types of radiation are harmful?
Radiation boosts are supplemental boosts usually given at the end of radiation treatments and usually at slightly higher doses with each boost to ensure your radiation treatments were and remain successful. They are akin to an end treatment bolus. Best of luck to you, Carm RN.

What is the success rate of radiation treatment?
What is boost in radiation therapy for prostate cancer?
How long does it take to heal after radiation therapy?
What is the best radiation treatment for cancer?
What is a normal PSA level after radiation?
What are the chances of prostate cancer returning after radiation?
Do tumors grow back after radiation?
What should I avoid after radiation?
What can you not do during radiation treatment?
What are the 3 types of radiation therapy?
- Brachytherapy involves radioactive material that is implanted in the body. ...
- Intraoperative radiation therapy (IORT) is used to treat an exposed tumor during cancer surgery. ...
- Stereotactic radiosurgery (SRS) is not actually surgery.
How does the body get rid of dead cancer cells?
At what stage of cancer is radiotherapy used?
What is radiation therapy for breast cancer?
Radiation therapy is planned specifically for your breast cancer, the shape of your body and your internal anatomy. This is why sessions can’t be split between different treatment centers. Your treatment plan is based on: The tumor size, type and location. The number of lymph nodes with cancer. The type of breast surgery (and lymph node surgery) ...
How long does radiation treatment last?
Each session lasts about 10-20 minutes.
What is hypofractionated breast irradiation?
This is called hypofractionated whole-breast irradiation. It’s like standard whole-breast radiation therapy except it uses a slightly higher dose of radiation per session (hypofractionation). This reduces the number of treatment sessions, making the overall course shorter. For most women with early breast cancer, ...
What is a boost breast?
After radiation therapy to the whole breast, you may have more radiation (called a boost) to the part of the breast that had the tumor. This boost increases the amount of radiation given to the area at highest risk for breast cancer recurrence. Your boost radiation session is similar to a regular session.
What is brachytherapy in cancer?
Brachytherapy uses targeted radiation placed inside the tumor bed. Implanted radiation “seeds” (interstitial radiation therapy) or a single small balloon device (intracavitary radiation therapy) can be used to deliver the radiation. External beam radiation therapy uses standard external beam radiation therapy, but only targets the tumor bed.
Why do you hold your breath during a radiation plan?
You may be asked to hold your breath during the planning session. This is one way to minimize radiation exposure to the heart.
Where does radiation go in breast?
Radiation therapy often delivers radiation to the whole breast. Partial breast irradiation delivers radiation only to the area around the tumor bed (the space where the tumor was removed during lumpectomy).
What is the main aim of radiation therapy?
Radiation therapy is the core treatment strategy with curative intent and organ preservation for many inoperable cancer types. The main aim of radiation therapy is the local control of the tumor.
How does breast radiotherapy help with cancer?
Breast-conserving surgery followed by whole breast radiotherapy has become the standard approach for early stage breast cancer since the survival rates have proved to be similar to those with radical surgery. Local control can be improved by an additional boost of 16 Gy to the lumpectomy cavity after administration of 50 Gy to the whole breast. Breast irradiation with a boost to the tumor bed provides significantly higher local recurrence rates than whole breast irradiation alone, namely, 93.8% vs. 89.8% at 10 years. In the EORTC study 22881–10882, the absolute benefit of a boost in terms of local control was most pronounced in young patients [ 52 – 55 ].
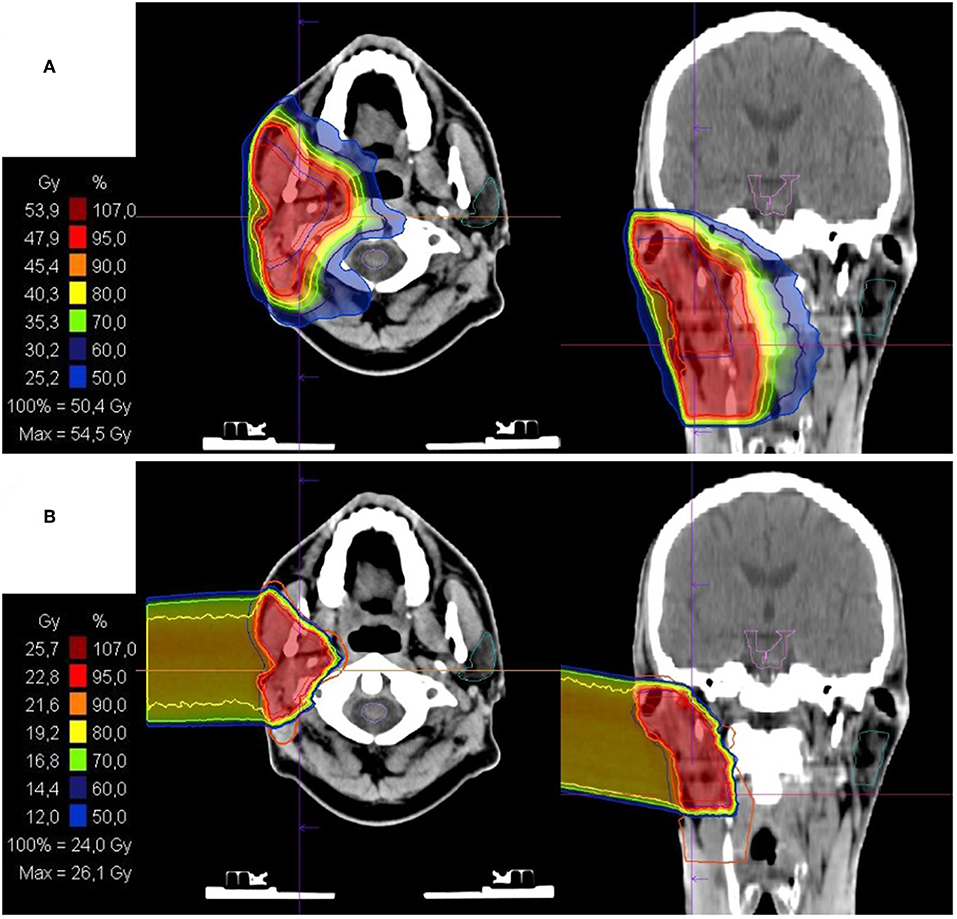
What is SIB radiotherapy?
The newly developed approach of applying different radiation doses to different areas in one single session is called SIB or simultaneous integrated boost-intensity-modulated radiotherapy (SIB-IMRT). By increasing the dose per fraction focally to the tumor itself while maintaining lower dose to the elective areas of interest, a more accurate dose distribution can be achieved, in order to improve local tumor control without putting the neighboring organs at risk. The advances, improvements and clinical usage of this technique will be expanded in full detail [ 7 ].
What is radiotherapy for cancer?
Radiotherapy has an established role in the treatment of cancer and represents a definitive, less invasive approach for various cancer types. Its main aim is to deliver the maximum dose to the tumor with minimal toxicity on neighboring healthy tissues.
How is radiation therapy applied?
In the past, radiation therapy was applied using a shrinking field approach or sequential boost, starting with large fields and shrinking gradually depending on the pre-planned total dose to each region. Inevitably, the high-risk target volume or GTV, the intermediate risk target volume or CTV and the low risk volume or PTV were exposed to different total doses, which have been delivered sequentially (SeqB-IMRT intensity-modulated radiotherapy sequential boost). This risk adaptive strategy now is modified to deliver a single efficient treatment plan with dose levels and intensities appropriate for each elected region. The SIB-IMRT is more conformal and potentially enables a slightly higher dose escalation to high-risk volumes compared to the SeqB-IMRT. Higher conformity in combination with smaller PTV allows 25% RT dose escalation and increases the effectiveness of therapy. A dose escalation of 10 Gy to lung cancer patients treated with 3D-CRT is correlated with 36% decrease in local failure rates [ 18 – 20 ].
What is the main concern of radiation oncology?
The radiation oncologist's main concern is local recurrence after definitive radiation therapy. The combined chemo-radiation protocols have led to the increased tumor control and survival rates, but the results have remained unchanged for a long time.
Is confined to the thorax a good treatment for lung cancer?
The true value of radiotherapy confined to the thorax is indisputable in the treatment of locally advanced nonsmall cell lung cancer. However, even with standard chemo-radiation, it is difficult to achieve durable local control, and this contributes to the high morbidity and mortality of patients with NSCLC. Results of RTOG 0617 clinical (Phase III) trial showed that the overall survival of stage III NSCLC patients given a high-dose (74 Gy) conformal radiation therapy with concurrent chemotherapy was no better than that of patients given the standard dose (60 Gy) [ 44 – 46 ]. The new idea is, instead of escalating the dose to the whole PTV, to selectively increase the treatment dose using SIB-IMRT to deliver a higher dose to the GTV and a relatively lower dose to the subclinical disease PTV [ 47 – 51 ].
What is boost in medicine?
Addition of a boost is an established technique for improving local control in higher-risk patients. However, improved local control can come at the cost of worse cosmetic outcomes ( 1, 4, 6, 7, 10 – 12 ). There is a lack of consensus between published guidelines on exactly which patients benefit from a boost, and largely, the decision is left to the discretion of individual physicians with or without the guidance of institutional policies and guidelines.
What is breast cancer treated with?
A considerable proportion of patients with early-stage breast cancer are treated with breast-conserving surgery (BCS) followed by whole breast radiation (WBI). In this group, an additional dose of radiation—a boost—can be delivered in order to reduce the risk of local recurrence ( 1 – 8 ). There is variation of boost dose, planning technique, ...
What is the best age to boost?
The benefit of boost in younger patients is appropriately reflected in the pattern-of-practice data, where age exerts a strong influence on the decision to add a boost ( 16 – 18 ), as well as in the guideline recommendations from collaborative groups and national agencies ( Table 1 ). Within these guidelines, age is the most consistently cited factor, with most using a cut-off of 50 years. However, beyond age, other determinants of boost utilization such as tumor grade, presence of lymphovascular invasion (LVI), hormone receptor status, and presence of positive margins are not supported by high-level evidence, creating the potential for variation in recommendations and practice, as reflected in the available guidelines ( Table 1 ).
Is a boost used in breast fractionation?
Instead, the data shows that a boost is used far less frequently in cases of hypofractionation, at least at some jurisdictions. The reason for lower utilization of a boost in hypofractionation could be from concern about inferior cosmesis. However, the current evidence shows similar toxicity profile and benefit for a boost with conventional vs. hypofractionated WBI. Therefore, the lower rates of boost utilization with hypofractionation represent an area of potential future research focus to support practice. Further studies specifically on the effect of adding a boost to hypofractionation will help elucidate this issue, but it will take years for relevant outcomes data to become available. In the meantime, it seems most reasonable to make decisions on addition of a boost independent from fractionation schedule.
Does a boost help with breast cancer?
Adding a boost to whole breast radiation (WBI) following breast-conserving surgery (BCS) may help improve local control, but it increases the total cost of treatment and may worsen cosmetic outcomes. Therefore, it is reserved for patients whose potential benefit outweighs the risks; however, current evidence is insufficient to support comprehensive and consistent guidance on how to identify these patients, leading to a potential for significant variations in practice. The use of a boost in the setting of close margins and hypofractionated radiotherapy represents two important areas where consensus guidelines, patterns of practice, and current evidence do not seem to converge. Close margins were previously routinely re-excised, but this is no longer felt to be necessary. Because of this recent practice change, good long-term data on the local recurrence risk of close margins with or without a boost is lacking. As for hypofractionation, although there is guidance recommending that the decision to add a boost be independent from the whole-breast fractionation schedule, it appears that patterns-of-practice data may show underutilization of a boost when hypofractionation is used. The use of a boost in these two common clinical scenarios represents important areas of future study for the optimization of adjuvant breast radiation.
Does boost reduce local recurrence?
3–4 mm or ≤ 2 mm ( p = 0.63). However, in an earlier analysis of the same data, Jones et al. ( 29) found that addition of a boost significantly reduced local recurrence in patients with negative margins >2 mm (HR 0.47, p = 0.0004), but not for patients with negative margins <2 mm or positive margins ( p = 0.65) . This study grouped <2-mm and positive margins together; however, there were relatively few patients with positive margins ( 29 ). Nevertheless, this may offer an explanation for the difference between Vrieling et al. ( 28) and Jones et al. ( 29 ). Additionally, Jones et al. ( 29) had a shorter median follow-up time of 10 years and it is possible that, with the shorter follow-up time, the effect of boost could not reach statistical significance for the <2-mm and positive margin group, which was roughly 4-fold smaller than the >2-mm group.
Does radiation boost affect cosmetic outcomes?
However, studies have shown that the higher radiation dose associated with the addition of a boost may lead to worse cosmetic outcomes ( 10 – 12 ). In a recent Cochrane review, adding a boost led to worse cosmesis when scored by a review panel (OR 1.41, 95% CI 1.07–1.85), but no difference in cosmetic outcomes when scored by a physician (OR 1.58, 0.93–2.69) ( 10 ). Immink et al. ( 11) assessed long-term cosmetic outcomes of 348 patients enrolled in the European Organization for Research and Treatment of Cancer (EORTC) boost vs. no boost trial. At 3 years, there was no significant difference between the patients that received a boost and those who did not; however, over longer-term follow-up it became clear that addition of a boost increased the degree of fibrosis ( 11 ). Another, larger analysis that included over 3,000 patients from this same trial found similar results ( 12 ). Specifically, they found that after a 10-year follow-up, the addition of a boost led to increased rates of moderate or severe fibrosis ( 12 ). In an older study that included just over 100 patients, addition of a boost was linked to other long-term side effects such as telangiectasis and depigmentation ( 13 ). Beyond cosmetic outcomes, use of a boost adds to the cost of radiation therapy. Lanni et al. ( 14) estimated that the cost of WBI was US$11,725 using opposed tangents and US$20,637 with 3D-CRT/IMRT. With the addition of a boost, this increased to $13,829 and $22,130, respectively ( 14 ).
What to expect when getting radiation therapy?
What to Expect When Having Radiation Therapy. It is normal to feel worried or overwhelmed when you learn that you will need radiation therapy. However, learning more about this type of cancer treatment may help you feel more prepared and comfortable.
How long does radiation therapy last?
It is the most common radiation therapy treatment for cancer. Each session is quick, lasting about 15 minutes. Radiation does not hurt, sting, or burn when it enters the body.
What is the role of a dosimetrist in radiation?
Dosimetrist. The dosimetrist helps your radiation oncologist calculate the right dose of radiation.
What type of doctor is responsible for radiation therapy?
Radiation oncologist. This type of doctor specializes in giving radiation therapy to treat cancer. A radiation oncologist oversees radiation therapy treatments. They work closely with other team members to develop the treatment plan. Radiation oncology nurse.
What is simulation in radiation therapy?
Simulating and planning treatment. Your first radiation therapy session is a simulation. This means it is a practice run without giving radiation therapy. Your team will use imaging scans to identify the tumor location.
What is radiation oncology nurse?
Radiation oncology nurse. This nurse specializes in caring for people receiving radiation therapy. A radiation oncology nurse plays many roles, including:
Why is it important to be in the same position for radiation?
It is important for your body to be in the same position for each treatment. Your radiation oncology team cares about your comfort. Talk with the team to find a comfortable position that you can be in every time you come in for radiation therapy.