What does the final section of the treatment plan mean?
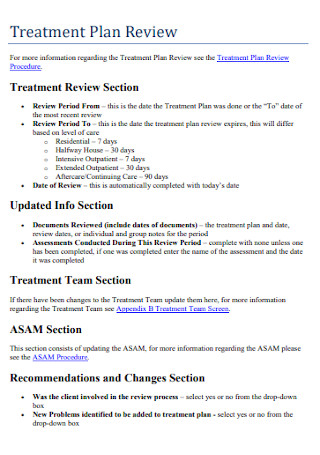
Jan 17, 2019 · Treatment planning is a team effort between the patient and health specialist. Both parties work together to create a shared vision and set attainable goals and objectives. Treatment Plan Template. A treatment plan is simple but specific. Although treatment plans vary, a treatment plan template or form generally contains the following fields:
What is a treatment plan?
Sep 25, 2019 · Here is a treatment plan example template, complete with objectives, interventions, and progress: GOAL 1: Chris will implement a parenting plan that promotes improved behavior in his son, as rated ...
What should the third section of a treatment plan include?
2. Planning o Develop a client treatment plan (and if applicable, obtain medication consent) with the client; then 3. Treating o Provide treatment services to address the identified mental health condition and assist the client in reaching his/her objectives.
What are the progress sections of a treatment plan?
Treatment Planning • Person Centered approach • Focus on the individual and their goals • Strengths, preferences, support systems • Necessary to identify current issues • Provides guidance for treatment • Allows for assessing progress over time • Collaborative effort • Responsibility and motivation is shared
What is midpoint billing?
This means the total time for therapy is the maximum number of units to bill (using the midpoint rule). For example, if the total time for all procedures in a day is equal to or greater than 23 minutes and less than 38 minutes, then two units should be billed.
Who can bill for 96156?
Clinical PsychologistCoding Guidelines The CPT codes 96156, 96158, 96159, 96164, 96165, 96167 and 96168 may be used only by a Clinical Psychologist (CP), (Specialty Code 68).
What is CPT 96156 health behavior assessment?
Group 1CodeDescription96156HEALTH BEHAVIOR ASSESSMENT, OR RE-ASSESSMENT (IE, HEALTH-FOCUSED CLINICAL INTERVIEW, BEHAVIORAL OBSERVATIONS, CLINICAL DECISION MAKING)96158HEALTH BEHAVIOR INTERVENTION, INDIVIDUAL, FACE-TO-FACE; INITIAL 30 MINUTES7 more rows
Who can Bill 90899?
E. CPT code 90899: Use CPT code 90899 when a psychiatric service cannot be described by any other psychiatric CPT code(s) (90801-90880).Mar 18, 2010
How Much Does Medicare pay for 99483?
Effective January 1 2021, Medicare increased payment for these services to $282 (may be geographically adjusted) when provided in an office setting, added these services to the definition of primary care services in the Medicare Shared Savings Program, and permanently covered these services via telehealth.
How often can 96156 be used?
Assessment services are now event-based and CPT code 96156 is billed only once per day regardless of the amount of time required to complete the overall service. Only report 96156 for assessment of a patient with a primary diagnosis that is physical in nature.
How often can 96132 be billed?
- The first hour of neuropsychological evaluation is billed using 96132 and each additional hour needed to complete the service is billed with code 96133. - CPT Time Rules allow an additional unit of a time-based code to be reported as long as the mid-point of the stated amount of time is passed.Jan 1, 2019
Does Medicare pay for 96160?
Medicare plans to pay an average of $4.67 for codes 96160 and 96161.
Who can bill for 98966?
non-physician practitionersDuring the COVID-19 Public Health Emergency (PHE), non-physician practitioners who are eligible to bill Medicare directly, including registered dietitians and nutrition professionals, may bill for audio-only telephone assessment and management services: CPT codes 98966-98968.Nov 18, 2020
IS 99211 being deleted in 2021?
CPT code 99211 (established patient, level 1) will remain as a reportable service. History and examination will be removed as key components for selecting the level of E&M service. Currently, history and exam are two of the three components used to select the appropriate E&M service.
Is 90853 covered by Medicare?
Medicare does not include the following services as part of coding CPT Code 90853: Teaching grooming skills. Monitoring daily living activities. Recreational therapy (dance, art, play)
How Much Does Medicare pay for 90833?
Medicaid Reimbursement Rates for PsychiatristsPsychiatry CPT CodeCPT Code DescriptionMedicaid Reimbursement Rate for Psychiatrists90832Individual Psychotherapy, 30 Minutes$42.9090833Individual Psychotherapy with Evaluation and Management Services, 30 minutesN/a90834Individual Psychotherapy, 45 Minutes$60.3117 more rows
Why are treatment plans important?
Treatment plans are important for mental health care for a number of reasons: Treatment plans can provide a guide to how services may best be delivered. Professionals who do not rely on treatment plans may be at risk for fraud, waste, and abuse, and they could potentially cause harm to people in therapy.
What is a mental health treatment plan?
Mental health treatment plans are versatile, multi-faceted documents that allow mental health care practitioners and those they are treating to design and monitor therapeutic treatment. These plans are typically used by psychiatrists, psychologists, professional counselors, therapists, and social workers in most levels of care.
What is HIPAA treatment plan?
Treatment Plans and HIPAA. The Health Insurance Portability and Accountability Act (HIPAA) Privacy Rule grants consumers and people in treatment various privacy rights as they relate to consumer health information, including mental health information.
What does a therapist do for Chris?
Therapist will provide psychoeducation on positive parenting and will support Chris in developing a concrete parenting plan. Therapist will provide materials for Chris to document the new house rules, rewards, and consequences system.
Why do people need treatment plans?
Treatment plans can also be applied to help individuals work through addictions, relationship problems, or other emotional concerns. While treatment plans can prove beneficial for a variety of individuals, they may be most likely to be used when the person in therapy is using insurance to cover their therapy fee.
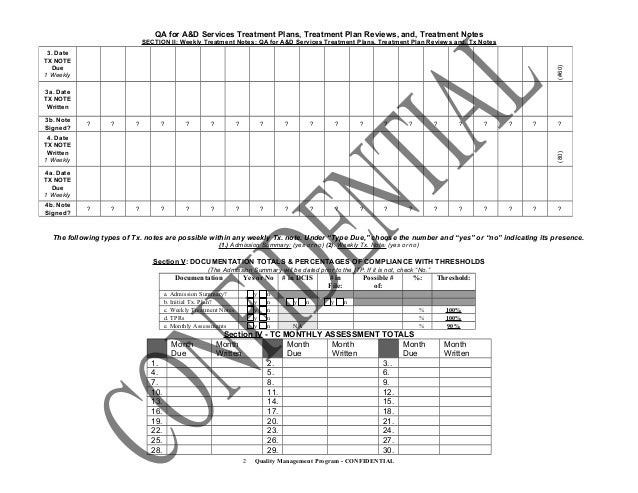
What is progress and outcomes?
Progress and outcomes of the work are typically documented under each goal. When the treatment plan is reviewed, the progress sections summarize how things are going within and outside of sessions. This portion of the treatment plan will often intersect with clinical progress notes.
What is goal language?
The language should also meet the person on their level. Goals are usually measurable—rating scales , target percentages , and behavioral tracking can be incorporated into the goal language to ensure that it is measurable .
What is a lockout in a mental hospital?
Medi-Cal Lockout = when Specialty Mental Health Services are not reimbursable by Medi-Cal(i .e. client is in an IMD, jail/prison setting, psychiatric inpatient/psychiatric health facility/crisis residential facility, excluding the dates of admission and discharge)
What is the PHQ 9 score?
Administered the PHQ-9 –client’s current score 14 (moderate): endorsed feeling depressed, feeling like a failure, difficulties falling asleep, and fatigue. Reviewed client’s homework (mood diary) focusing on the triggers of his depressed mood and patterns of negative self-talk and self-defeating beliefs. Focused on challenging his underlying
What is client-treatment matching?
Client–treatment matching attempts to place the client in those treatments most appropriate to his or her needs. There are a number of dimensions on which treatments may vary and which need to be considered in attempting to make an appropriate referral or match (Marlatt 1988; W.R. Miller 1989 b; Institute of Medicine 1990; Donovan et al. 1994; Gastfriend and McLellan 1997). Among these dimensions are treatment setting (e.g., inpatient, residential, outpatient), treatment intensity, specific treatment modalities, and the degree of therapeutic structure. A number of possible variables may interact with these dimensions to lead to differential outcomes, making the clinician’s task more difficult.
What is the primary goal of assessment?
Within the clinical context, the primary goal of assessment is to determine those characteristics of the client and his or her life situation that may influence treatment decisions and contribute to the success of treatment (Allen 1991). Additionally, assessment procedures are crucial to the treatment planning process.
What is Shiffman's theory of relapse proneness?
Shiffman (1989) suggested that three levels of information are necessary in order to gain a sense of the individual’s “relapse proneness,” and thus are relevant to treatment planning. These fall along a continuum of their proximity, in both time and influence, to the probability of relapse.
What is the locus of control?
The concept of locus of control, originally developed by Rotter (1966, 1975), refers to the extent to which an individual believes that the outcomes of important life events are under personal control (internal locus of control) or under the influence of chance, fate, or powerful others (external locus of control). Rotter suggested that the predictive utility of the locus of control construct is increased by using measures directly related to the behavior under consideration rather than ones assessing a more generalized perception of control.
What are the stages of alcohol abuse?
The first two stages involve screening, case finding, and identification of a substance use disorder; an evaluation of the parameters of drinking behavior, signs, symptoms, and severity of alcohol dependence, and negative consequences of use; and formal diagnosis of alcohol abuse or dependence.
Is drinking behavior multidimensional?
Drinking behavior and alcohol problems are multidimensional. As such, it is often important to have a broad overview of the parameters of drinking, the expectancies that accompany and potentially maintain alcohol use, and the biopsychosocial aspects of the individual’s life that are affected by drinking (Donovan 1988). Assessments thus need to be relatively broad to capture the extent and complexity of the multiple facets of alcohol problems. This can be done by the use of instruments derived from a variety of assessment domains or that assess a broad range of factors within a single interview or questionnaire. A number of such instruments are reviewed in this section.
What is a mental health treatment plan?
At the most basic level, a mental health treatment plan is simply a set of written instructions and records relating to the treatment of an ailment or illness. A treatment plan will include the patient or client’s personal information, the diagnosis (or diagnoses, as is often the case with mental illness), a general outline ...
Why do we need treatment plans?
Treatment plans can reduce the risk of fraud, waste, abuse, and the potential to cause unintentional harm to clients. Treatment plans facilitate easy and effective billing since all services rendered are documented.
What is the treatment contract?
Treatment Contract – the contract between the therapist and client that summarizes the goals of treatment. Responsibility – a section on who is responsible for which components of treatment (client will be responsible for many, the therapist for others)
What is the part of effective mental health?
Part of effective mental health treatment is the development of a treatment plan. A good mental health professional will work collaboratively with the client to construct a treatment plan that has achievable goals that provide the best chances of treatment success. Read on to learn more about mental health treatment plans, how they are constructed, ...
What is intervention in therapy?
Interventions – the techniques, exercises, interventions, etc., that will be applied in order to work toward each goal. Progress/Outcomes – a good treatment plan must include space for tracking progress towards objectives and goals (Hansen, 1996)
What is blended care in therapy?
Blended care involves the provision of psychological services using telecommunication technologies.
What is a goal in counseling?
Goals are the broadest category of achievement that clients in mental health counseling work towards. For instance, a common goal for those struggling with substance abuse may be to quit using their drug of choice or alcohol, while a patient struggling with depression may set a goal to reduce their suicidal thoughts.
Why do treatment plans go hand in hand with progress notes?
2. Progress Notes. Treatment plans and progress notes tend to go hand in hand because progress notes need to incorporate one or more treatment objectives.
How does a mental health treatment plan complement other therapy notes?
A treatment plan is a tool that promotes good communication between staff members and helps provide documentation necessary for billing.
What is the role of a counselor in a treatment plan?
A counselor must use their skills to help a client establish the best goals and objectives for their unique condition. Counselors can ask themselves these questions to help uncover the best goals for their patients:
What is the goal of a mental health treatment plan?
Both parties work together to create a shared vision and set attainable goals and objectives. A goal is a general statement of what the patient wishes to accomplish .
What is objective in medical?
An objective, on the other hand, is a specific skill a patient must learn to reach a goal. Objectives are measurable and give the patient clear directions on how to act. Examples of objectives include: An alcoholic with the goal to stay sober might have the objective to go to meetings.
How to evaluate the effectiveness of a treatment plan?
To evaluate the effectiveness of the treatment plan, you need to keep score of how the patient is doing. Ask the patient to count and keep track of their thoughts, feelings and behaviors in a log so you can monitor their progress.
What is a treatment plan?
A treatment plan is a detailed plan tailored to the individual patient and is a powerful tool for engaging the patient in their treatment. Treatment plans usually follow a simple format and typically include the following information: The patient’s personal information, psychological history and demographics.
What is a treatment plan?
In both mental and general healthcare settings, a treatment plan is a documented guide or outline for a patient’s therapeutic treatment. Treatment plans are used by professionals such as psychologists, psychiatrists, behavioral health professionals, and other healthcare practitioners as a way to: Design. Blueprint. Evaluate, and.
Why is it important to involve patients in the treatment planning process?
Involving patients in the treatment planning process, and especially in the goal-setting stage, is often a great way for therapists and psychologists to build patient health engagement for optimal involvement and motivation.
What is therapeutic objective?
Therapeutic objectives or goals: Both over the longer term, and broken down into shorter-term subgoals. Treatment modalities: For example, the behavioral, social, or psychological treatments that will be targeted. Interventions/Methods: A description of the techniques and approaches to be implemented.
What is a treatment plan in healthcare?
Treatment plans are a crucial part of any mental healthcare solution and feature regularly in practitioners’ day-to-day work with patients.
What is specific goal and objectives?
With specific goals and objectives, healthcare professionals and their patients can clarify the desired outcomes that they will be working toward. As well as helping practitioners identify the most appropriate techniques and psychological tools for a client’s therapy, they can give a useful overview of what resources will be required, as well as the time frame for the treatment itself. [4]
What are the responsibilities of behavioral health practitioners?
Behavioral health practitioners have specific responsibilities when they accept reimbursement from a government program. They “have a duty to ensure that the claims submitted to Federal health care programs are true and accurate,”[7] and that their medical record documentation supports and justifies billed services. All practitioners’ documentation is open to scrutiny by many, including employers, Federal and State reviewers, and auditors.[8, 9] Practitioners can protect themselves and their practices by implementing an internal self-auditing strategy.
What is behavioral health?
Behavioral health practitioners are in the business of helping their patients. Patients are their priority. Meeting ongoing patient needs, such as furnishing and coordinating necessary services, is impossible without documenting each patient encounter completely, accurately, and in a timely manner. Documentation is often the communication tool used by and between professionals. Records not properly documented with all relevant and important facts can prevent the next practitioner from furnishing sufficient services. The outcome can cause unintended complications.
Problem Recognition, Motivation, and Readiness to Change
- An important construct within the alcoholism field is the degree to which drinkers are aware of the extent of their drinking patterns, such as quantity and frequency of drinking, the negative physical and psychosocial consequences of their drinking, and their perception of these patterns and consequences as problematic. The goal of using screening ...
Alcohol–Related Expectancies and Self–Efficacy
- Clinicians and clinical researchers have increasingly focused on the role of cognitive factors in decisions to drink and in drinkers’ responses to alcohol (Oei and Jones 1986; Young and Oei 1993; Oei and Baldwin 1994; Oei and Burrow 2000; B.T. Jones et al. 2001). Two broad categories of such cognitive factors having implications for the development and maintenance of drinking pro…
Perceived Locus of Control of Drinking Behavior
- A final set of cognitions that have played a role in some cognitive–behavioral models of problem drinking and alcoholism is the individual’s perception of control (e.g., Donovan and O’Leary 1983; Carlisle 1991). The concept of locus of control, originally developed by Rotter (1966, 1975), refers to the extent to which an individual believes that the outcomes of important life events are unde…
Measures of Family History of Alcohol Problems
- Shiffman (1989) indicated that in addition to assessing factors that are relatively proximal in time to a relapse episode (e.g., temptation and confidence levels), a comprehensive assessment should also measure factors in the individual’s life that are more distal, both in time and influence, on drinking. These more distant, often relatively enduring and unchanging personal characteristi…
Extra–Treatment Social Support
- An important area to consider as part of the assessment process is the extent and nature of the individual’s social support system. Perceived social support may serve as a moderator of the relationship between a positive family history of alcoholism and the development of alcohol problems (Ohannessian and Hesselbrock 1993). Litman (1986) noted that the ability to access s…
Multidimensional Assessment Measures
- Drinking behavior and alcohol problems are multidimensional. As such, it is often important to have a broad overview of the parameters of drinking, the expectancies that accompany and potentially maintain alcohol use, and the biopsychosocial aspects of the individual’s life that are affected by drinking (Donovan 1988). Assessments thus need to be relatively broad to capture t…
Measures to Assist in Differential Treatment Placement
- Client–treatment matching attempts to place the client in those treatments most appropriate to his or her needs. There are a number of dimensions on which treatments may vary and which need to be considered in attempting to make an appropriate referral or match (Marlatt 1988; W.R. Miller 1989b; Institute of Medicine 1990; Donovan et al. 1994; Gastfriend and McLellan 1997). A…
Summary
- This chapter’s review of instruments potentially helpful in the treatment planning process should not be seen as exhaustive. Other measures of similar assessment domains likely exist and may be useful to the clinician. There are also a number of other important assessment domains that were not included in this review. Examples include affective states, such as anxiety and depressi…
Acknowledgments
- The preparation of this chapter was supported, in part, by the National Institute on Alcohol Abuse and Alcoholism Cooperative Agreement on Combining Pharmacological and Behavioral Treatments for Alcoholism, U10–AA11799.
References
- Abellanas, L., and McLellan, A.T. “Stage of change” by drug problem in concurrent opioid, cocaine, and cigarette users. J Psychoactive Drugs25:307–313, 1993. Adams, S.L., and McNeil, D.W. Negative alcohol expectancies reconsidered. Psychol Addict Behav5:9–14, 1991. Addiction Research Foundation. Directory of Client Outcome Measures for Addictions Treatment Program…