Benchmark plans About half the states have a benchmark plan that includes some form of infertility treatment coverage (the benchmark plan in each state serves as the model for the minimum level of coverage that individual and small group plans in the state must provide; see definition number two).
Which benchmark plans include diagnosis of infertility and insemination?
Infertility treatment is included in the Rhode Island Benchmark Plan that defines the EHBs for RI QHPs. Federal mandates regarding EHBs supersede RI state mandates with regards to removing any annual and lifetime dollar limits. § 27-20-20 Coverage for infertility.
Does New Mexico’s benchmark health plan include infertility coverage?
Infertility treatment is included in the Rhode Island Benchmark Plan that defines the EHBs for RI QHPs. Federal mandates regarding EHBs supersede RI state mandates with regards to removing any annual and lifetime dollar limits. The following is the State of Rhode Island Mandate regarding coverage of infertility services for females § 27-20-20.
What is a benchmark plan?
May 14, 2013 · Fertility Within Reach has reviewed the Essential Health Benefit (EHB) plans for states with some form of mandated infertility benefit. The objective was to identify which states would have infertility treatment as a minimum benefit among it’s state insurance plans and which states are at risk of losing their mandated infertility benefits.
Should all health plans provide access to infertility treatment?
Individual plan—both on and off the Marketplace—that took effect after 2013 must cover EHBs for new and renewing members. We offer two plan variations that satisfy the mandate. Our Benchmark plans only cover EHBs, while our standard plans cover EHBs as well as additional services. Below is a list of the most common
What is benchmark plan?
Benchmark plan is the term used to describe the second-lowest-cost Silver plan available in the exchange, and it's also the term for the plan that each state designates as the standard for essential health benefits (EHBs).
What is an ACA benchmark plan?
Benchmark plan refers to: The second-lowest-cost silver plan in the exchange (marketplace) in each area, in the individual/family insurance market, OR. The plan that each state uses to define essential health benefits within that state for individual/family and small group plans.Nov 28, 2021
What does ehb deductible mean?
DEDUCTIBLES FOR EHB COVERED SERVICES—The deductible per individual per benefit year is $50 for basic and major services. The deductible does not apply to diagnostic and preventive and orthodontic services. ANNUAL AND LIFETIME MAXIMUM PAYMENTS FOR EHB.
What are the benefits of the Affordable Care Act?
The Far-Reaching Benefits of the Affordable Care Act's Medicaid ExpansionIncreased health coverage.Better access to health care.Better health outcomes, including fewer premature deaths.More financial security and opportunities for economic mobility.Lower uncompensated care costs.A stronger response to COVID-19.Oct 21, 2020
What is a benchmark meeting?
Benchmarking is the practice of comparing business processes and performance metrics to industry bests and best practices from other companies. Dimensions typically measured are quality, time and cost.
What coinsurance means?
The percentage of costs of a covered health care service you pay (20%, for example) after you've paid your deductible. Let's say your health insurance plan's allowed amount for an office visit is $100 and your coinsurance is 20%. If you've paid your deductible: You pay 20% of $100, or $20.
What is a minimum essential coverage plan?
Minimum Essential Coverage is defined as the type of health insurance coverage that you must have in order to comply with the individual mandate set forth by the Affordable Care Act (ACA) . From January 1, 2014, and onward, individuals must have MEC insurance or they will be subject to a tax penalty.
What does high PPO mean?
A preferred provider organization (PPO) is a plan type with lower deductibles but higher monthly premiums. With a PPO, you pay more money each month but have lower out-of-pocket costs for medical services and may be able to access a wider range of providers.
What is the Affordable Care Act 2020?
The act required that all Americans purchase (or otherwise obtain) health insurance and prohibited insurance companies from denying coverage (or charging more) due to pre-existing conditions. It also allows children to remain on their parents' insurance plan until age 26.
What is wrong with Obamacare plan?
The ACA has been highly controversial, despite the positive outcomes. Conservatives objected to the tax increases and higher insurance premiums needed to pay for Obamacare. Some people in the healthcare industry are critical of the additional workload and costs placed on medical providers.
What are the four major components of the Affordable Care Act?
The Affordable Care Act: A Brief Summary - March 2011Expand Access to Insurance Coverage. ... Increase Consumer Insurance Protections. ... Emphasize Prevention and Wellness. ... Improve Health Quality and System Performance. ... Curb Rising Health Costs.
What are the drawbacks of Obamacare?
Cons:The cost has not decreased for everyone. Those who do not qualify for subsidies may find marketplace health insurance plans unaffordable. ... Loss of company-sponsored health plans. ... Tax penalties. ... Shrinking networks. ... Shopping for coverage can be complicated.Sep 29, 2021
How much does fertility treatment cost?
Most patients pay out of pocket for fertility treatment, which can amount to well over $10,000 depending on the services received. This means that in the absence of insurance coverage, fertility care is out of reach for many people.
What is the diagnostic service for fertility?
Diagnostics typically include lab tests, a semen analysis and imaging studies or procedures of the reproductive organs.
What is iatrogenic infertility?
Iatrogenic, or medically induced, infertility refers to when a person becomes infertile due to a medical procedure done to treat another problem, most often chemotherapy or radiation for cancer. In these situations, persons of reproductive age may desire future fertility, and may opt to freeze their eggs or sperm (cryopreservation) for later use. The American Society for Reproductive Medicine ( ASRM) encourages clinicians to inform patients about fertility preservation options prior to undergoing treatment likely to cause iatrogenic infertility.
What is the most common cause of infertility?
Both female and male factors contribute to infertility, including problems with ovu lation (when the ovary releases an egg), structural problems with the u terus or fallopian tubes, problems with sperm quality or motility, and hormonal factors ( Figure 1 ). About 25% of the time, infertility is caused by more than one factor, and in about 10% of cases infertility is unexplained. Infertility estimates, however do not account for LGBTQ or single individuals who may also need fertility assistance for family building. Therefore, there are varied reasons that may prompt individuals to seek fertility care.
Why do people need fertility aid?
This could either be due to a diagnosis of infertility, or because they are in a same-sex relationship or single and desire children. While there are several forms of fertility assistance, many services are out of reach for most people because of cost.
Is infertility covered by Medicare?
According to the Medicare Benefit policy manual, “reasonable and necessary services associated with treatment for infertility are covered under Medicare.”. However, specific covered services are not listed, and the definition of “reasonable and necessary” are not defined.
Can you pay for fertility care out of pocket?
Because eligibility for Medicaid is based on being low-income, people enrolled in the program likely could not afford to pay for services out of pocket. The relative lack of Medicaid coverage for fertility services stands in stark contrast to Medicaid coverage for maternity care and family planning services.
What is a benchmark plan?
Benchmark plans. About half the states have a benchmark plan that includes some form of infertility treatment coverage (the benchmark plan in each state serves as the model for the minimum level of coverage that individual and small group plans in the state must provide; see definition number two ). Most of those states overlap with the states ...
Which states have benchmark plans?
For example: The benchmark plans in Arizona , DC, and Tennessee only include coverage for the diagnosis of infertility. The benchmark plans in Kansas, Michigan, Missouri, New Hampshire, New Mexico (as of 2022), Virginia, and West Virginia only include diagnosis of infertility and treatment of the underlying causes of infertility.
What states have infertility mandates?
They include: Arizona, DC, Iowa, Michigan, Missouri, Nevada, North Carolina, Pennsylvania, Tennessee, and Virginia. (Note that although Colorado’s infertility mandate does not take effect until 2022, the state’s benchmark plan does include some infertility coverage, but it’s limited to diagnosis and artificial insemination.
How many states have infertility insurance?
Nineteen states have laws that require at least some coverage for infertility treatment on state-regulated health plans: Arkansas, California, Colorado ( effective as of 2022), Connecticut, Delaware, Hawaii, Illinois, Louisiana, Maryland (coverage enhanced as of 2021 as a result of SB988), Massachusetts, Montana, New Hampshire, New Jersey, New York, Ohio, Rhode Island, Texas, Utah, and West Virginia. Four of these states — Colorado, Delaware, New Hampshire, and Utah — have joined this list since 2018.
Which states have IVF coverage?
The benchmark plans in Connecticut, Hawaii, Illinois, Maryland, and Massachusetts all include more comprehensive coverage, including IVF (note that these are all states with laws requiring infertility coverage).
Is infertility covered by the ACA?
A. No. Treatment for infertility is not one of the ten essential benefits, and coverage for it is not mandated by the ACA or any other federal law. But that doesn’t mean it’s never covered, as states can have regulations that go beyond the minimum requirements laid out by the federal government. Whenever a health insurance benefit is not mandated ...
Does IVF insurance cover in vitro fertilization?
In those 19 states, the mandated coverage varies quite a bit from one state to another. Some do not cover in vitro fertilization (IVF) or medications, some have specific diagnosis requirements or lifetime benefit maximums, others only require coverage on large group plans, and/or HMOs, etc.
What is an EHB benchmark plan?
In plan years 2014 through 2016, the EHB-benchmark plan is a plan that was sold in 2012. Those 2014-2016 EHB-benchmark plans and associated materials can be found here. For plan years 2017, 2018, and 2019, each State’s EHB-benchmark plan is based on a plan that was sold in 2014. For plan year 2020 and after, the Final 2019 HHS Notice ...
What is the HHS notice of benefits and payment parameters for 2020?
For plan year 2020 and after, the Final 2019 HHS Notice of Benefits and Payment Parameters promulgated 45 CFR 156.111, which provides States with greater flexibility by establishing new standards for States to update their EHB-benchmark plans, if they so choose. For the 2020 plan year, CMS approved changes to the Illinois EHB-benchmark plan (ZIP).
Does EHB have preventive services?
The EHB-benchmark plans displayed may not offer the preventive services described in 45 CFR 147.130. However, as described in 45 CFR 156.115 (a) (4), EHB plans must comply with that section.
Does EHB cover abortion?
Please also note that although the EHB-benchmark plan may cover abortion services, section 156.115 (c) provides that no health plan is required to cover abortion services as part of the requirement to cover EHB .
What is IUI policy?
The policy addresses medical necessity criteria and coverage guidelines related to the treatment of female infertility using assisted reproductive technology such as artificial intrauterine insemination (IUI) or in vitro fertilization (IVF). While IUI is addressed in this policy, this service is not impacted by benefit limits or the prior authorization process. However, the member must meet eligibility criteria for coverage of IUI.
Is cryopreservation covered by the iatrogenic infertility insurance?
Retrieval and cryopreservation of eggs, embryos and sperm are covered for members not in active infertility treatment when a medically necessary medical treatment may directly or indirectly cause iatrogenic infertility. Iatrogenic infertility means an impairment of fertility by surgery, radiation, chemotherapy, or other medical treatment affecting reproductive organs or processes.
Is infertility treatment included in the Rhode Island Benchmark Plan?
Infertility treatment is included in the Rhode Island Benchmark Plan that defines the EHBs for RI QHPs. Federal mandates regarding EHBs supersede RI state mandates with regards to removing any annual and lifetime dollar limits.
What is EHB in fertility?
Fertility Within Reach has reviewed the Essential Health Benefit (EHB) plans for states with some form of mandated infertility benefit. The objective was to identify which states would have infertility treatment as a minimum benefit among it’s state insurance plans and which states are at risk of losing their mandated infertility benefits.
Does the default plan include infertility benefits?
The recommended plan may or may not provide infertility benefits. The default plan does not include infertility benefits.
Does EHB cover infertility?
Therefore, any state with infertility treatment within their EHB plan would also see infertility treatment within other insurance policies. States that did not include infertility benefits in the EHB plan, but have a mandated infertility benefit, face having to pay the cost associated with the mandated coverage.
Can an EHB mandate eliminate infertility?
States with an infertility mandate, but lack EHB infertility coverage may create legislation to eliminate the current mandated infertility benefit. It is critical to contact your legislator and ask them to protect the infertility mandated benefit in your state.
What is the ASRM evaluation?
An ASRM committee opinion on the diagnostic evaluation for infertility in women addresses several tests and procedures, starting with a comprehensive medical, reproductive and family history, as well as a thorough physical exam. Subsequent evaluation should be conducted in a systematic, expeditious and cost-effective manner so as to identify all relevant factors, with initial emphasis on the least invasive methods for detection of the most common causes of infertility. Diagnostic tests and procedures include evaluation for ovulatory dysfunction, ovarian reserve, cervical factors, uterine abnormalities, tubal disease and peritoneal factors (ASRM, 2015).
Do you have to have a mandate for infertility?
Infertility services are always subject to mandate review . Several states mandate benefit coverage for certain Infertility services, but the requirements for coverage vary from state to state. Legislative mandates and the member specific benefit document must be reviewed when determining benefit coverage for Infertility services. Where legislative mandates exist, they supersede benefit plan design. Benefit coverage for testing and treatment of Infertility are available only for the person(s) who are covered under the benefit document, and only when the member's specific plan provides benefits for Infertility diagnosis and/or treatment. The member specific benefit document should be reviewed for applicable benefits, limitations and/or exclusions.
Is ovarian tissue banking considered experimental?
An ASRM committee opinion states that ovarian tissue banking is an acceptable fertility preservation technique and is no longer considered experimental. However, data on the efficacy, safety, and reproductive outcomes after ovarian tissue cryopreservation are still limited. Given the current body of literature, ovarian tissue cryopreservation should be considered an established medical procedure with limited effectiveness that should be offered to carefully selected patients (ASRM, 2019c).
Is there evidence for uterine receptivity testing?
There is insufficient evidence supporting the safety and efficacy of uterine receptivity testing and/or treatment. More studies are needed to support improved outcomes such as successful pregnancies with delivery of liveborn children.
Is inhibin B a measure of ovarian reserve?
There is insufficient evidence to permit conclusions regarding the use of inhibin B as a measure of ovarian reserve. More studies are needed to support improved outcomes (i.e., increased successful pregnancies with delivery of liveborn children) with the use this test.
Does cryopreservation restore fertility?
Hayes report (2019; updated 2021) concluded that a low-quality, limited body of evidence suggests that ovarian tissue cryopreservation and transplantation have the potential to restore ovarian function and may result in preserved fertility in patients who have undergone gonadotoxic cancer treatment. Limitations include an evidence base composed of 2 poor-quality cohort studies, 6 poor-quality singe-arm studies and 1 very-poor-quality cross-sectional study. Better quality prospective studies ensuring that all patients are followed after receiving transplantation would provide better assurance that the effects of ovarian tissue cryopreservation and subsequent transplantation on fertility and pregnancy outcomes are consistent with these findings. Future evidence should evaluate the long-term safety and efficacy in populations who are unable to undergo current standard fertility preservation techniques (i.e., embryo or oocyte cryopreservation).
Is there evidence for sperm function test?
There is insufficient evidence to permit conclusions regarding the use of this sperm function test . Study results to date have demonstrated low specificity, low sensitivity and a high rate of false positives.
Introduction
- The other type of benchmark plan is the reference plan in each state for determining what benefits are covered by individual and small group plans in the state. All individual/family and small group plans—with effective dates of 2014 or later—must cover the ACA's ten essential hea…
Diagnosis and Treatment Services
Utilization of Fertility Services
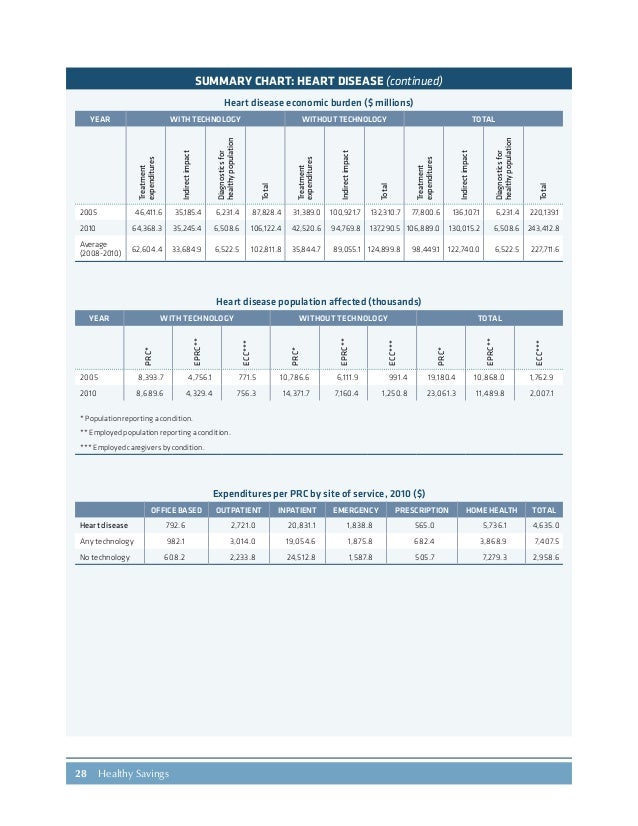
Cost of Services
Insurance Coverage
- Infertility is most commonly defined1 as the inability to achieve pregnancy after 1 year of regular, unprotected heterosexual intercourse, and affects an estimated 10-15% of heterosexual couples. Both female and male factors contribute to infertility, including problems with ovulation (when the ovary releases an egg), structural problems with the u...
Key Populations
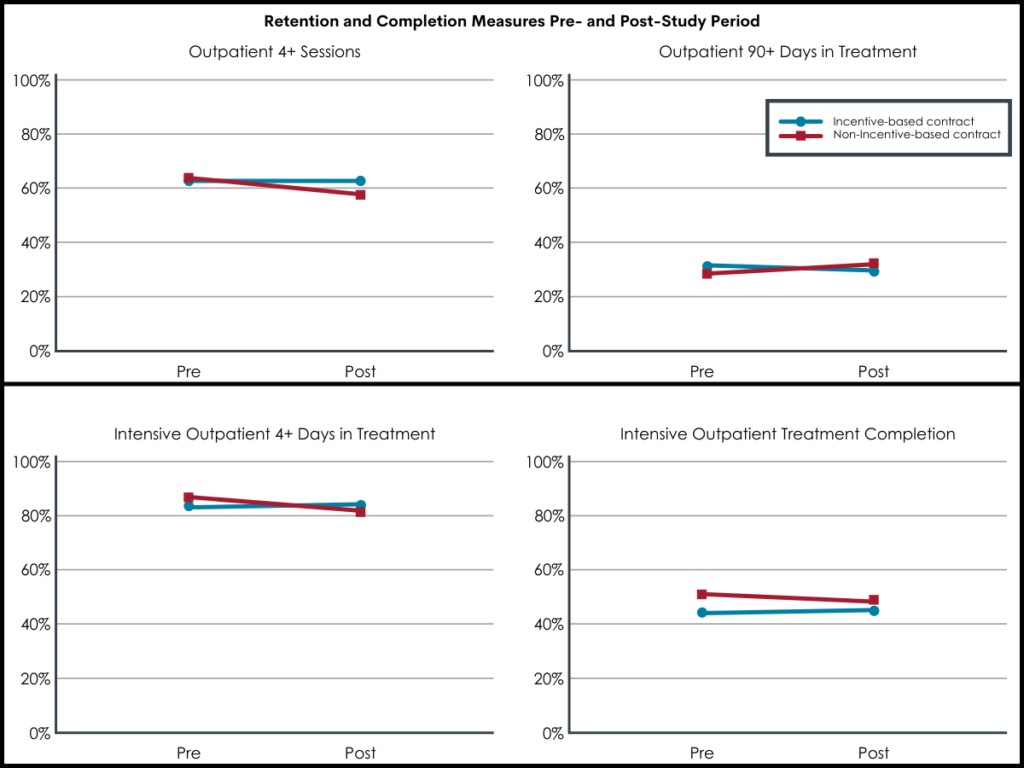
- Our analysis of the 2015-2017 National Survey of Family Growth (NSFG) finds that 10% of women2 ages 18-49 say they or their partner have ever talked to a doctor about ways to help them become pregnant (data not shown).3 Among women ages 18-49, the most commonly reported service is fertility advice (Figure 2). The CDC finds that use of IVF has steadily increased since it…
Looking Forward
- Many patients lack access to fertility services, largely due to its high cost and limited coverage by private insurance and Medicaid. As a result, many people who use fertility services must pay out of pocket, even if they are otherwise insured. Out of pocket costs vary widely depending on the patient, state of residence, provider and insurance plan. Generally, diagnostic lab tests, semen a…
Plan Year 2020 and Beyond Ehb-Benchmark Plans
- Insurance coverage of fertility services varies by the state in which the person lives and, for people with employer-sponsored insurance, the size of their employer. Many fertility treatments are not considered “medically necessary” by insurance companies, so they are not typically covered by private insurance plans or Medicaid programs. When coverage is available, certain ty…
Overview of Current Essential Health Benefits (EHB) Benchmark Plans
- The ability to have and care for the family that you wish for is a fundamental tenet of reproductive justice. For those who need it, this includes access to fertility services. The share of racial and ethnic minorities who utilize medical services to help become pregnant is less than that of non-Hispanic White women, despite research that has found higher rates of infertility among wome…
Annual and Lifetime Dollar Limits
- On a federal level, efforts to pass legislation to require insurers to cover fertility services are largely stalled. The proposed Access to Infertility Treatment and Care Act(HR 2803 and S 1461), which would require all health plans offered on group and individual markets (including Medicaid, EHBP, TRICARE, VA) to provide infertility treatment, is still in committee (and never made it out o…
Coverage Limits
- EHB-Benchmark Plan Selection Process for Plan Year 2020 and Beyond
CMS provided States with greater flexibility to select its EHB-benchmark plan by providing three new options for selection in plan year 2020 and beyond, including: 1. Option 1:Selecting the EHB-benchmark plan that another State used for the 2017 plan year. 2. Option 2:Replacing one or mo… - Template and Documentation Requirements for Plan Year 2020 and Beyond
In accordance with 45 CFR 156.111(a), States may choose to select a new EHB-benchmark plan to be applicable starting in plan year 2020. To select a new EHB-benchmark plan, the State must submit: 1. EHB State Confirmation Template, 2. Actuarial Certification/Report, 3. EHB-Benchmar…
EHB Benchmark Plan Prescription Drug Coverage by Category and Class
- Please click here (PDF)to view a consolidated list of the EHB-benchmark plans for the 50 states and D.C. that states used for at least plan years 2017, 2018, and 2019. Additional information regarding each of these plans is available by selecting a particular State below. During the public comment period for selection of the plan year 2017-2019 EHB-benchmark plans, which closed o…
Excluded Benefits
- The EHB-benchmark plans displayed may include annual and/or lifetime dollar limits; however, in accordance with 45 CFR 147.126, these limits cannot be applied to the essential health benefits. Annual and lifetime dollar limits can be converted to actuarially equivalent treatment or service limits.
Habilitative Services and Devices
- Pursuant to 45 CFR 156.115(a)(2), with the exception of coverage for pediatric services, a plan may not exclude an enrollee from coverage in an entire EHB category, regardless of whether such limits exist in the EHB-benchmark plan. For example, a plan may not exclude dependent children from the category of maternity and newborn coverage.
Mental Health Parity
- Please note that in some cases a prescription drug category is listed without a United States Pharmacopeia (USP) class because there are some drugs within the category that have not been assigned to a specific class. Please also note that, pursuant to 45 CFR 156.122, if the EHB-benchmark plan does not include any coverage in a USP category and/or class (count is zero), E…
Preventive Services
- Pursuant to 45 CFR 156.115, the following benefits are excluded from EHB even though an EHB-benchmark plan may cover them: routine non-pediatric dental services, routine non-pediatric eye exam services, long-term/custodial nursing home care benefits, and/or non-medically necessary orthodontia. Please also note that although the EHB-benchmark plan may cover abortion service…
State-Required Benefits
- The EHB benchmark plans displayed may not include coverage of habilitative services and devices. Pursuant to 45 CFR 156.110(f), the State may determine which services are included in the habilitative services and devices category if the base-benchmark plan does not include such coverage. If the State does not supplement the missing habilitative services and devices catego…