Explore
What intervention is most appropriate for the treatment of a patient in asystole? When treating asystole, epinephrine can be given as soon as possible but its administration should not delay initiation or continuation of CPR. After the initial dose, epinephrine is given every 3-5 minutes. Rhythm checks should be performed after 2 minutes (5 ...
What are the treatment options for asystole?
Standard asystole treatment involves cardiopulmonary resuscitation, or CPR, and intravenous administration of epinephrine given every three to five minutes as needed. When a reversible underlying cause is found, that cause should be treated directly to reverse asystole.
What is the first drug/dose to administer for asystole?
Jul 19, 2021 · Asystole should be treated following current American Heart Association BLS and ACLS guidelines. High-quality CPR is the mainstay of treatment and the most important predictor of favorable outcomes. Asystole is a non-shockable rhythm. Therefore, if asystole is noted on the cardiac monitor, no attempt at defibrillation should be made.
Is defibrillation an effective treatment for asystole?
The only two drugs recommended or acceptable by the American Heart Association (AHA) for adults in asystole are epinephrine and vasopressin. Atropine is no longer recommended for young children and...
When should epinephrine be given to a patient with asystole?
Which is the most appropriate intervention to perform next? Obtain a 12 lead ECG. A patient in respiratory failure becomes apneic but continues to have a strong pulse. The heart rate is dropping rapidly and now shows a sinus bradycardia at a rate of 30/min. ... Which intervention is most appropriate for the treatment of a patient in asystole ...
What is treatment during asystole?
Why do you not defibrillate asystole?
When is it recommended to administer epinephrine to a patient with asystole?
Administer first dose at the onset of cardiac resuscitation.Mar 24, 2010
What drug do you give first for asystole?
When can you defibrillate a patient?
Should we shock asystole?
How do hospitals administer epinephrine?
Can you give epinephrine and amiodarone together?
When do you give epinephrine IV?
What happens when a patient is in asystole?
What does atropine do in asystole?
What is the only intervention that can restore an organized rhythm?
What is the definition of asystole?
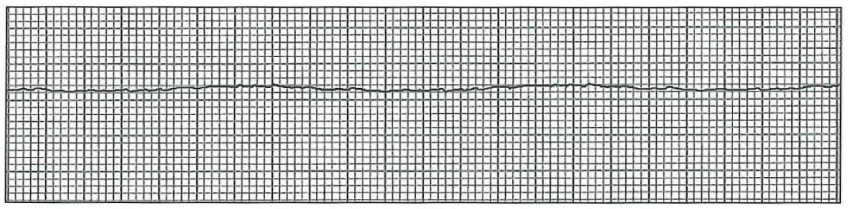
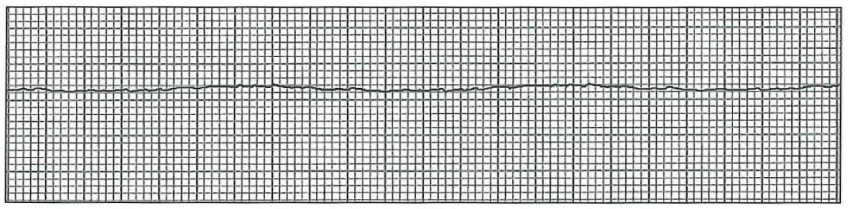
Asystole is defined as a cardiac arrest rhythm in which there is no discernible electrical activity on the ECG monitor. Consequently, it is sometimes referred to as a “flat line.” Confirmation that a “flat line” is truly asystole is an important step in the ACLS protocol.
What is a vasopressor?
A vasopressor is a medication that produces vasoconstriction and a rise in blood pressure. The vasopressor that is used for the treatment within the right branch of the Cardiac Arrest Algorithm is epinephrine. Epinephrine is primarily used for its vasoconstrictive effects. Vasoconstriction is important during CPR because it will help increase blood ...
Why is epinephrine used in CPR?
Epinephrine is primarily used for its vasoconstrictive effects. Vasoconstriction is important during CPR because it will help increase blood flow to the brain and heart. When treating asystole, epinephrine can be given as soon as possible but its administration should not delay initiation or continuation of CPR.
What is the best medicine for asystole?
For asystole, the standard medication to use is epinephrine.
What is the term for a state of cardiac standstill in which all electrical activity has ceased?
Asystole, otherwise known as a flatline, is a state of cardiac standstill in which all electrical activity has ceased. It is diagnosed following a physical examination where no pulse is detected in conjunction with ECG monitoring.On an ECG tracing, asystole appears as a flatline:
Is vasopressin a good substitute for epinephrine?
Previous versions of the AHA guidelines have suggested that higher doses of epinephrine (greater than the standard 1mg dose), or an alternative vasopressor, called vasopressin, could be more effective alternatives to the standard dose of epinephrine.
What is the best medicine for asystole?
The only two drugs recommended or acceptable by the American Heart Association (AHA) for adults in asystole are epinephrine and vasopressin. Atropine is no longer recommended for young children and infants since 2005, and for adults since 2010 for pulseless electrical activity (PEA) and asystole.
Why is continuous cardiac monitoring important?
Continuous cardiac monitoring is useful during attempts at resuscitation to determine rhythm and effects of intervention. Endotracheal intubation is indicated during resuscitation. Central venous access or intraosseous access may be needed for vascular access.